Risks of too much niacin can be serious, affecting your health in various ways. Understanding the potential dangers of excessive niacin intake is crucial for maintaining optimal well-being. This comprehensive guide delves into the various forms of niacin, its role in the body, and the risks associated with consuming too much. We’ll explore potential symptoms,…
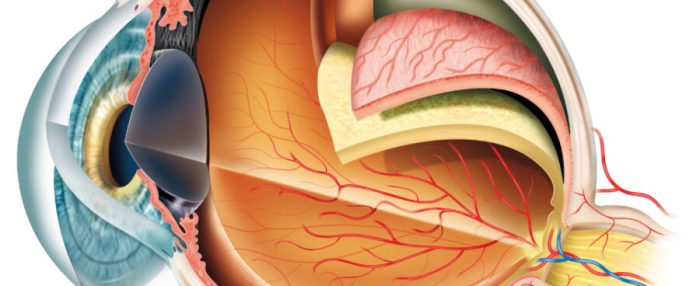
Eye Injections for AMD A Comprehensive Guide
Eye injections for AMD offer a potential lifeline for those struggling with age-related macular degeneration. This guide delves into the intricacies of these treatments, exploring the different types of AMD, the medications used in eye injections, and the procedures involved. We’ll also discuss the potential benefits, risks, and post-injection care. Understanding the specifics of eye…
Purified vs Distilled Water A Deep Dive
Purified vs distilled water is a common topic of debate, especially for those concerned about the quality of their drinking water. This in-depth look will explore the differences between these two types of water, examining their purification methods, chemical composition, health implications, applications, cost, environmental impact, and more. We’ll delve into the science behind each…
What is Palliative Care A Comprehensive Guide
What is palliative care? It’s a specialized approach to care that focuses on improving the quality of life for people facing serious illnesses. Unlike curative care, which aims to cure disease, palliative care aims to provide comfort and support, both for the patient and their loved ones. This comprehensive guide explores the various aspects of…
Should You Put Mouthwash in Your Water Flosser?
Should you put mouthwash in your water flosser? This intriguing question sparks a fascinating debate about enhancing oral hygiene. Adding mouthwash to your water flosser might seem like a logical next step, but is it actually beneficial, or could it introduce unwanted complications? Let’s dive deep into the potential benefits, risks, and practical considerations of…
Does Milk Make You Taller? Unveiling the Truth
Does milk make you taller? This age-old question sparks curiosity and debate. We’ll delve into the intricate relationship between milk consumption and height, exploring the science behind growth and development, the nutritional value of various milk types, and the evidence from scientific studies. This exploration promises to shed light on whether that glass of milk…
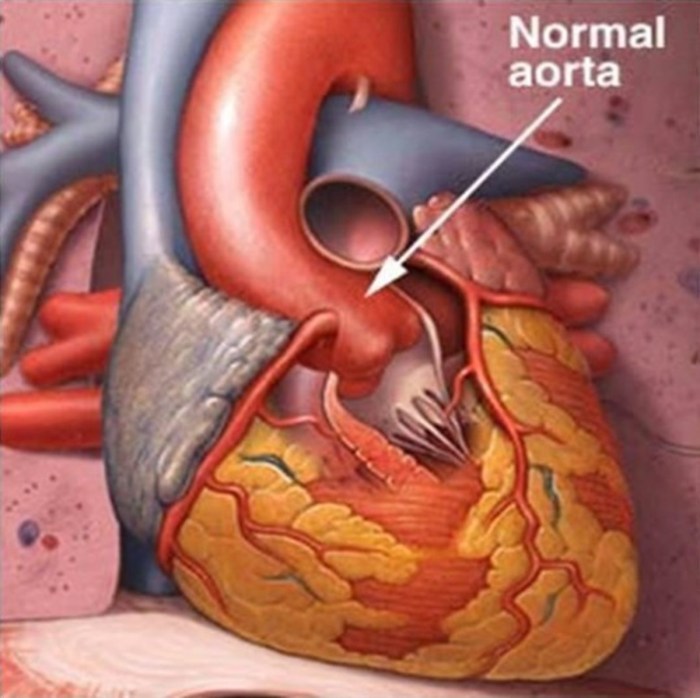
How Long Does Metoprolol Take to Work?
How long does it take for metoprolol to work? This crucial question often arises for patients prescribed this beta-blocker. Understanding the factors influencing its onset, from dosage to individual physiology, is key to managing expectations and ensuring effective treatment. This exploration delves into the intricacies of metoprolol’s action, examining the timeframes involved in achieving its…
Opill OTC Available for Retail A Deep Dive
Opill OTC available for retail is a significant development with implications for consumer access and healthcare. This post explores the legal frameworks, pharmacy practices, consumer demand, supply chain management, and marketing strategies surrounding the retail availability of these medications. We’ll examine the differences in regulations across various regions and how these factors impact the retail…
How Long Does Valium Take to Work?
How long does it take Valium to work? This question is crucial for anyone considering or currently taking this medication. Valium, or diazepam, is a powerful benzodiazepine used to treat anxiety, muscle spasms, and seizures. Understanding the factors influencing its onset of action is key to managing expectations and ensuring optimal results. Different factors like…
Adenosis Enlarged Breast Lobules A Comprehensive Guide
Adenosis enlarged breast lobules is a condition characterized by the abnormal growth of the milk-producing glands within the breasts. Understanding the intricacies of this condition, including its causes, symptoms, diagnosis, and management, is crucial for both patients and healthcare professionals. This guide delves into the various aspects of adenosis enlarged breast lobules, providing a clear…