Unexplained weight loss definition and causes: This post delves into the complexities of weight loss that happens without a clear reason. We’ll explore the definition, common medical conditions, nutritional factors, lifestyle influences, diagnostic procedures, illustrative cases, and preventative strategies. Understanding these factors can be crucial for early detection and effective treatment. The definition of unexplained…
Can I Use Topical Steroid Creams on My Face?
Can I use topical steroid creams on my face? This question is frequently asked by those experiencing facial inflammation. Understanding the benefits, risks, and alternatives is crucial for making informed decisions. Topical steroids can effectively reduce inflammation, but their use comes with potential side effects. Careful consideration and consultation with a dermatologist are essential for…
Surgery for Bowel Obstruction A Comprehensive Guide
Surgery for a bowel obstruction is a critical procedure for restoring normal bowel function when blockages prevent waste passage. This comprehensive guide delves into the intricacies of this procedure, from understanding the causes and types of obstructions to the pre-operative assessments, surgical techniques, post-operative care, and potential complications. We’ll explore the differences between mechanical and…
What are Cancer Cells A Deep Dive
What are cancer cells? They’re essentially rogue cells, out of control and wreaking havoc on the body’s delicate balance. Unlike healthy cells that follow specific instructions for growth and division, cancer cells ignore these rules, multiplying rapidly and aggressively. This relentless growth disrupts normal bodily functions, potentially leading to severe health consequences. Understanding what drives…
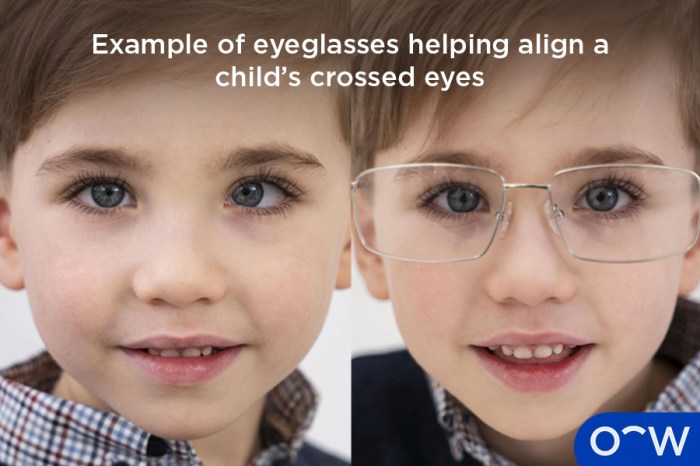
Esotropia Crossing of the Eyes A Comprehensive Guide
Esotropia crossing of the eyes is a condition where one or both eyes turn inward, creating a “crossed-eyes” appearance. Understanding this complex condition requires exploring its various types, from accommodative to non-accommodative, and the underlying mechanisms that cause these misalignments. This guide will delve into the causes, symptoms, diagnostic methods, treatment options, and the lasting…
Top Surgery Day of Surgery A Deep Dive
Top surgery day of surgery is a critical moment, filled with anticipation and careful preparation. This detailed look covers everything from pre-operative evaluations and the surgical procedure itself, to post-operative care and the surgical facility environment. We’ll explore the crucial steps involved, the different considerations, and the vital role of the surgical team. This guide…
Herbs for Menstrual Cramps Natural Relief
Herbs for menstrual cramps offer a natural approach to easing those painful periods. This guide explores various herbs, their potential mechanisms of action, and important safety considerations. We’ll delve into popular choices, research findings, and even how to combine herbs for personalized relief. From understanding the science behind herbal remedies to practical recipes, this comprehensive…
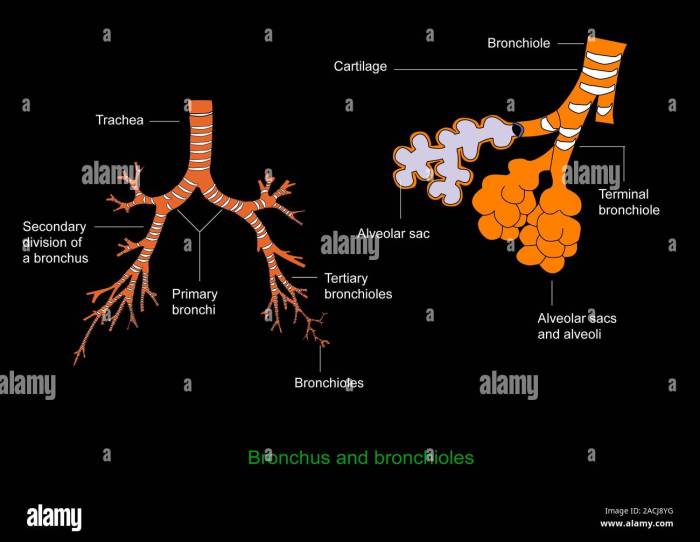
What is the Bronchus Structure, Function, and Conditions?
What is the bronchus structure function and conditions? This exploration delves into the intricate world of the bronchi, the air passages that carry oxygen deep into our lungs. We’ll uncover their anatomical layout, their vital physiological roles, and the common diseases that can affect them. From the branching patterns of the bronchi to the mechanisms…
FDA Approves Velsipity for Ulcerative Colitis
FDA approves velsipity to treat ulcerative colitis, marking a significant advancement in the management of this chronic inflammatory condition. This new treatment, Velsipity, promises to offer a fresh approach for patients struggling with ulcerative colitis, potentially improving their quality of life and long-term outcomes. This article delves into the details of Velsipity’s mechanism of action,…
What is Spider Angioma? A Deep Dive
What is spider angioma? This fascinating skin condition, often appearing as a central red vessel with radiating blood vessels, can be intriguing and sometimes concerning. Understanding its various characteristics, causes, and treatment options is crucial for anyone who encounters it. This article explores the intricacies of spider angiomas, from their appearance and potential origins to…