Magnesium for muscle pain is a crucial topic for understanding the role of this vital mineral in maintaining healthy muscles. Magnesium plays a significant part in muscle function, and deficiencies can lead to a range of issues, including persistent muscle aches and discomfort. This article explores the intricate connection between magnesium and muscle pain, examining…
Papilledema Symptoms Causes, Diagnosis, and Treatment
Papilledema symptoms causes diagnosis treatment – Papilledema symptoms, causes, diagnosis, and treatment are crucial for understanding this potentially serious condition. This comprehensive guide delves into the various visual and non-visual symptoms, exploring the underlying causes from intracranial pressure to tumors. We’ll examine diagnostic methods, from ophthalmoscopy to imaging, and discuss the diverse treatment approaches, from…
Skin Boils Picture Gallery Visual Guide
Skin boils picture gallery sets the stage for a comprehensive visual guide to understanding these common skin conditions. This resource will provide clear images and descriptions of skin boils at various stages, helping you identify them accurately. We’ll explore different types, potential causes, and even treatment options. Learn how to distinguish skin boils from similar…
Your Rights to Your Medical Records Under HIPAA
Your rights to your medical records under HIPAA are crucial for maintaining control over your health information. This guide delves into the specifics, exploring your ability to access, amend, and understand the disclosure of your medical records, along with your rights in the event of a security breach. Understanding these rights empowers you to navigate…
Baby Rash on Face A Comprehensive Guide
Baby rash on face can be a common and sometimes concerning issue for parents. This guide delves into the various types of rashes, their causes, symptoms, diagnosis, treatment options, and preventative measures. We’ll explore everything from heat rash to allergic reactions, providing a comprehensive understanding to help you identify and manage these skin conditions effectively….
What is Barretts Esophagus A Deep Dive
What is barretts esophagus – What is Barrett’s esophagus? This condition occurs when the lining of your esophagus, the tube connecting your mouth and stomach, changes. It’s a significant health concern that can lead to serious complications if not properly managed. This in-depth exploration will delve into the causes, symptoms, diagnosis, complications, treatment options, and…
Secondary Headache Overview and More Understanding the Causes
Secondary headache overview and more delves into the complexities of headaches beyond the familiar. This exploration examines the crucial distinction between primary headaches, often idiopathic, and secondary headaches, where an underlying medical condition triggers the pain. Understanding the causes, symptoms, and diagnostic processes is key to effective management and treatment. Knowing how to differentiate these…
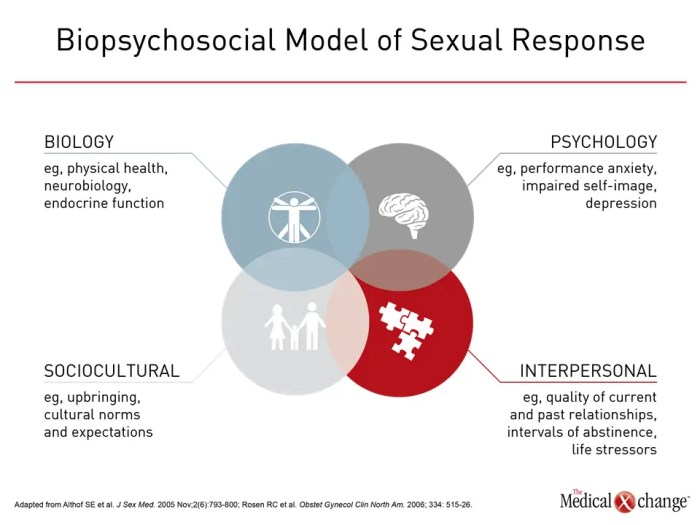
Hypoactive Sexual Desire Disorder A Comprehensive Guide
Hypoactive sexual desire disorder symptoms causes diagnosis treatment and coping is a multifaceted issue affecting many individuals. This in-depth exploration delves into the complexities of this condition, examining its symptoms, potential causes, diagnostic processes, available treatments, and effective coping strategies. We’ll cover the nuances of low libido versus HSDD, exploring the biological, psychological, and relational…
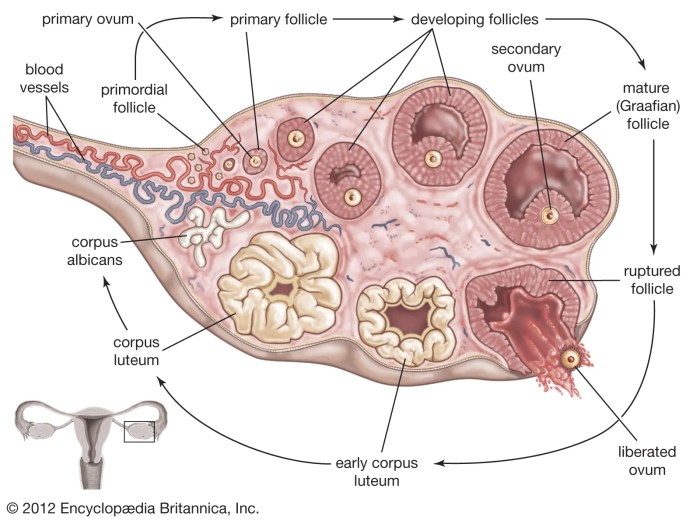
Things to Know About Your Ovaries and Ovulation
Things to know about your ovaries and ovulation: Dive deep into the fascinating world of female reproductive health. This comprehensive guide explores the intricate workings of your ovaries, the crucial ovulation process, and the overall menstrual cycle. From understanding ovarian anatomy to recognizing potential health concerns and fertility, you’ll gain valuable insights into your body’s…
Is Coconut a Tree Nut? Unveiling the Truth
Is coconut a tree nut? This question sparks curiosity and debate, especially among those with allergies or a keen interest in botany. Unraveling the truth requires a deep dive into botanical classifications, nutritional comparisons, and historical contexts. This exploration will demystify the differences between coconuts and true tree nuts. We’ll dissect the scientific characteristics that…