Whats the difference between delirium and dementia? These two conditions, though both affecting cognitive function, have vastly different characteristics, onsets, and courses. Understanding these distinctions is crucial for accurate diagnosis and effective treatment. Delirium typically emerges suddenly, often triggered by an underlying medical issue, and involves fluctuating attention and awareness. Dementia, on the other hand, is a progressive decline in cognitive abilities, developing gradually over time.
This post delves into the key characteristics of both conditions, comparing their symptoms, diagnostic approaches, and treatment strategies. We’ll explore the various factors contributing to each condition and provide a clearer picture of how to differentiate between them. The content will be presented in a way that is both informative and easy to understand, with illustrative examples to highlight the differences.
Defining Delirium and Dementia: Whats The Difference Between Delirium And Dementia
Understanding the differences between delirium and dementia is crucial for accurate diagnosis and appropriate treatment. Both conditions significantly impair cognitive function, but their underlying causes, progression, and symptoms differ markedly. This section delves into the key characteristics of each condition, providing a clear comparison to help differentiate them.Delirium and dementia, while both impacting cognitive abilities, are distinct neurological conditions.
Delirium is an acute confusional state, characterized by a rapid onset and fluctuating symptoms, while dementia represents a progressive decline in cognitive function over a longer period. Understanding these differences is critical for timely intervention and effective management.
Defining Delirium
Delirium is an acutely disturbed state of mind that comes on suddenly. It’s often characterized by confusion, disorientation, and a fluctuating level of consciousness. The onset is typically rapid, occurring within hours or days. The duration is also typically shorter, resolving within a few days to a few weeks if treated properly.Underlying causes of delirium are varied and often linked to medical conditions, such as infections, electrolyte imbalances, medication side effects, or even surgery.
Figuring out the difference between delirium and dementia can be tricky, but it boils down to how quickly the confusion sets in and how long it lasts. Sometimes, these cognitive changes can be linked to other conditions, like dissociative and conversion disorder, which can manifest as sudden memory problems or altered states of consciousness. Ultimately, though, a proper diagnosis requires a thorough medical evaluation to distinguish these conditions from simple forgetfulness or age-related cognitive decline.
Understanding the nuanced distinctions between these conditions is crucial for effective treatment.
Risk factors for delirium include age, pre-existing medical conditions, and the use of multiple medications. Delirium often presents as a sudden change in the patient’s baseline mental status.
Defining Dementia
Dementia encompasses a broad range of progressive neurological disorders that lead to a decline in cognitive functions, including memory, language, and problem-solving skills. The onset is typically gradual, progressing over months or years. The duration is considerably longer, with a steady deterioration of cognitive abilities.Underlying causes of dementia are complex and multifaceted. Factors like genetics, lifestyle choices, and exposure to certain environmental toxins may play a role.
Alzheimer’s disease is the most common type of dementia, characterized by the abnormal build-up of proteins in the brain. Other forms include vascular dementia, Lewy body dementia, and frontotemporal dementia. Risk factors for dementia often include age, family history of dementia, and certain lifestyle choices.
Comparing Delirium and Dementia Symptoms
| Characteristic | Delirium | Dementia | Example |
|---|---|---|---|
| Onset | Rapid (hours to days) | Gradual (months to years) | A patient suddenly becomes confused after a surgery, versus a patient slowly forgetting appointments over several years. |
| Attention | Impaired | Often preserved (early stages) | A patient with delirium struggles to focus on conversation, whereas a patient with early-stage dementia might still be able to engage in conversation but with occasional lapses in memory or recall. |
| Cognitive Function | Fluctuating | Progressive decline | A patient with delirium might be alert and oriented one moment and confused the next, whereas a patient with dementia shows a consistent decline in memory and other cognitive abilities over time. |
These differences in onset, duration, and underlying causes are vital in distinguishing delirium from dementia. A timely and accurate diagnosis is critical for appropriate treatment and management.
Distinguishing Symptoms
Spotting the difference between delirium and dementia can be tricky, as both conditions affect cognitive function. However, careful observation of behavioral and cognitive changes, along with the fluctuating nature of delirium, can help clinicians and caregivers distinguish between the two. The key lies in understanding the unique patterns of symptom presentation for each condition.Understanding the nuanced differences in symptoms is crucial for appropriate diagnosis and treatment.
Early intervention is vital for both conditions, but the approaches to management differ based on the specific cause and nature of the cognitive impairment. The fluctuating nature of delirium often requires immediate medical attention to address the underlying cause.
Behavioral Symptoms of Delirium
Delirium is characterized by a rapid onset of fluctuating mental status changes. Behavioral symptoms often include restlessness, agitation, and disorganized thinking. These symptoms can manifest as hallucinations, delusions, or disorientation. A person experiencing delirium might become easily startled or anxious, exhibit unpredictable mood swings, and have difficulty sleeping.
Cognitive Symptoms of Delirium
Cognitive symptoms in delirium often involve problems with attention and awareness. The individual may have difficulty focusing, maintaining attention, and responding to questions. Memory issues, such as difficulty recalling recent events, are also common. Disorientation to time, place, or person is a significant indicator. A person might also have impaired judgment and difficulty with problem-solving.
Cognitive Symptoms of Dementia
Dementia is a progressive decline in cognitive function. Cognitive symptoms typically include difficulties with memory, language, problem-solving, and judgment. These symptoms gradually worsen over time, affecting the individual’s ability to perform daily activities. A person with dementia may experience difficulty recognizing familiar faces or objects.
Fluctuating Attention and Awareness in Delirium
A hallmark of delirium is its fluctuating nature. Attention and awareness are not consistently impaired. Periods of lucidity can alternate with periods of confusion, disorientation, and agitation. This fluctuation is a critical diagnostic feature that sets delirium apart from dementia. For instance, a patient might be alert and responsive during one part of the day but become confused and agitated during another.
Impact on Daily Functioning
Delirium’s impact on daily functioning is often more acute and dramatic compared to dementia. While dementia gradually impairs daily activities, delirium can rapidly disrupt daily routines. Tasks like eating, bathing, and dressing might become difficult or impossible for the individual experiencing delirium. The fluctuating nature of delirium further complicates daily functioning, making it unpredictable.
Understanding the difference between delirium and dementia is crucial, but sometimes, we need to prioritize other aspects of health, like the risks of skin-to-skin contact, especially when considering STDs/STIs. For example, learning about the potential STIs associated with dry humping skin-to-skin contact is essential information to consider when prioritizing your health. stdsti risks of dry humpingskintoskin contact Ultimately, getting informed about these risks allows for better decisions about health choices, which can indirectly help with recognizing the subtle differences between delirium and dementia.
A deeper understanding of both topics can improve overall well-being.
Observable Differences in Behavior
Observing behavioral differences is important for distinguishing between delirium and dementia. Someone with delirium may exhibit sudden changes in mood, from calm to agitated, and vice versa. They might be more easily startled or show increased anxiety. In contrast, a person with dementia shows a gradual decline in cognitive abilities and behavioral patterns. Examples include forgetting appointments, repeating questions, or having difficulty with familiar tasks.
| Characteristic | Delirium | Dementia |
|---|---|---|
| Onset | Rapid (hours to days) | Gradual (months to years) |
| Attention | Fluctuating | Diminished |
| Awareness | Fluctuating | Relatively stable |
| Memory | Short-term, recent memory impairment | Short-term and long-term memory impairment |
| Mood | Rapid mood swings | Mood changes, but generally more stable |
Diagnostic Considerations
Differentiating delirium from dementia is crucial for appropriate treatment and management. Accurate diagnosis hinges on a thorough understanding of the presenting symptoms, medical history, and a systematic evaluation of cognitive function. This process involves careful consideration of the patient’s current state, past medical history, and any potential contributing factors. Effective diagnosis requires a multidisciplinary approach, combining clinical observations with objective assessments.
Diagnostic Criteria
Diagnostic criteria for delirium and dementia are established to provide standardized guidelines for clinicians. These criteria aid in the identification of distinguishing features and help rule out other potential causes of cognitive impairment. For delirium, the key is identifying an acute onset of fluctuating cognitive disturbance, often linked to a specific medical condition. Dementia, on the other hand, presents as a progressive decline in cognitive abilities over a longer period, typically not associated with an acute medical event.
These differences in the course of the cognitive impairment are essential in the diagnostic process.
Medical History and Physical Examination
A comprehensive medical history is paramount in the diagnostic process. This includes inquiring about the patient’s past medical conditions, medications, recent illnesses, and any recent life changes. A thorough physical examination is equally important, as it can reveal underlying medical conditions contributing to the cognitive symptoms. Physical examination can also detect vital signs abnormalities, physical indicators of illness, and other factors that may indicate delirium.
Figuring out the difference between delirium and dementia can be tricky, but understanding the symptoms is key. It’s important to recognize the subtle shifts in mental function. Learning how to tell if your ankle is broken, for example, requires a careful assessment of the injury how to tell if your ankle is broken , just like recognizing the specific changes in alertness and cognitive decline associated with delirium versus dementia.
Ultimately, both situations require a prompt and accurate diagnosis from a healthcare professional.
Laboratory Tests and Neuropsychological Assessments
Laboratory tests are often utilized to identify potential medical conditions that could be contributing to delirium or dementia. These tests may include blood tests, urine tests, and imaging studies. Neuropsychological assessments are essential to evaluate cognitive domains such as memory, attention, language, and executive function. These assessments help quantify cognitive deficits and assess the extent of the impairment.
Neuropsychological assessments can also provide insights into the specific cognitive domains affected, which can help differentiate between delirium and dementia.
Assessment Tools for Cognitive Function
Various assessment tools are employed to evaluate cognitive function and aid in the differentiation of delirium and dementia. These tools provide standardized methods to measure cognitive performance, enabling clinicians to quantify the extent of the impairment. Key tools include the Mini-Mental State Examination (MMSE) and the Confusion Assessment Method (CAM).
| Diagnostic Tool | Description | Application | Strengths |
|---|---|---|---|
| Mini-Mental State Examination (MMSE) | A brief questionnaire assessing orientation, registration, attention, recall, and language. | Useful for assessing global cognitive function, identifying deficits, and monitoring changes over time. Suitable for dementia, but less useful in delirium due to fluctuating nature. | Quick, easy to administer, and provides a general cognitive status score. Standardized, allowing for comparisons across patients and over time. |
| Confusion Assessment Method (CAM) | A structured clinical interview evaluating features of delirium. | Specifically designed to identify delirium by looking for acute onset, fluctuating course, inattention, and disorganized thinking. | Sensitive to the fluctuating nature of delirium and its specific characteristics, making it more appropriate for delirium diagnosis than MMSE. |
Treatment Approaches

Navigating the complexities of delirium and dementia necessitates a multifaceted approach that prioritizes the underlying causes and addresses the unique needs of each individual. Effective treatment hinges on a comprehensive understanding of these conditions, allowing for tailored interventions that promote well-being and quality of life.
Treating the Underlying Cause of Delirium, Whats the difference between delirium and dementia
Delirium, unlike dementia, is a temporary state. Identifying and addressing the underlying medical condition is paramount. This could include infections, medication side effects, dehydration, electrolyte imbalances, or even a recent surgery. Prompt diagnosis and treatment of the causative factor are crucial for reversing the symptoms and restoring the individual’s cognitive function. For example, if a patient is experiencing delirium due to a urinary tract infection, treating the infection with antibiotics will typically resolve the delirium.
Management Strategies for Delirium and Dementia
Managing both delirium and dementia necessitates a holistic strategy. For delirium, management involves supportive care to reduce agitation and promote safety. For dementia, strategies focus on maintaining cognitive function, enhancing communication, and fostering a supportive environment. This encompasses non-pharmacological interventions like cognitive stimulation therapy, reminiscence therapy, and creating a structured daily routine.
Supportive Care and Environmental Modifications
Creating a safe and supportive environment is critical for both delirium and dementia patients. Reducing environmental stimuli, such as noise and clutter, can significantly reduce agitation and anxiety in individuals with delirium. Similarly, dementia patients often benefit from a structured environment with clear cues and reminders. This could include labeled objects, calendars, and visual aids to help maintain orientation and reduce confusion.
For example, placing familiar objects or photos in the patient’s room can provide a sense of comfort and security.
Pharmacological Interventions
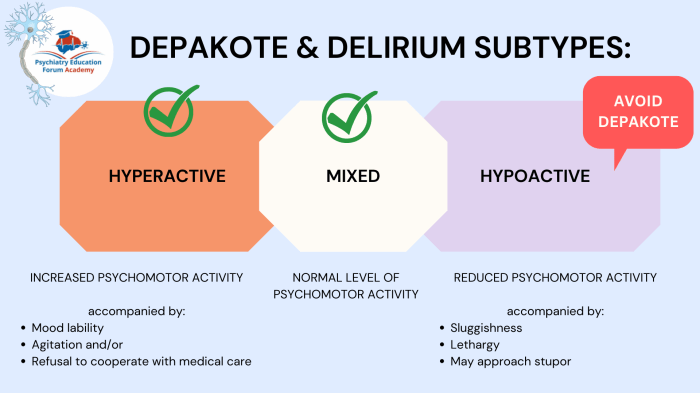
Pharmacological interventions play a role in managing both delirium and dementia, but their use should be carefully considered and tailored to the individual. In delirium, medications are primarily used to address symptoms like agitation and hallucinations, but only when other interventions have failed. In contrast, dementia medications aim to slow the progression of cognitive decline, but they do not cure the disease.
Examples include cholinesterase inhibitors for mild to moderate Alzheimer’s disease, which may improve cognitive function, and memantine, which can slow the progression of symptoms in moderate to severe Alzheimer’s. It is crucial to note that the choice of medication and dosage must be individualized, and close monitoring of the patient is essential to ensure safety and effectiveness.
Comparison of Pharmacological Interventions
| Feature | Delirium | Dementia ||——————-|——————————————-|——————————————–|| Primary Goal | Manage symptoms, treat underlying cause | Slow disease progression, manage symptoms || Medication Type| Primarily to address symptoms (antipsychotics, benzodiazepines, etc.) | Often cholinesterase inhibitors, memantine, etc.|| Duration of Use| Usually short-term, until underlying cause is resolved | Often long-term, as dementia is progressive || Monitoring | Frequent, especially for side effects | Ongoing, to monitor efficacy and side effects |
Flowchart for Managing Delirium and Dementia
Initial Assessment | V Identify Underlying Cause (Delirium) | V Treat Underlying Cause | V Non-Pharmacological Interventions (Both) | V Pharmacological Intervention (as needed, Delirium) | V Monitor and Adjust Treatment (Both) | V Support and Environmental Modifications (Both) | V Ongoing Assessment and Management (Both)
Prognosis and Long-Term Implications
Understanding the potential outcomes and long-term effects of delirium and dementia is crucial for both individuals and their caregivers.
This section explores the varied prognoses, the lasting impacts on quality of life, and the support systems available. It also emphasizes the importance of effective communication strategies in managing these conditions.
Potential Outcomes for Delirium
Delirium, often a temporary state, typically resolves within days or weeks. However, the recovery process can vary significantly depending on the underlying cause. Some individuals experience a full recovery without any lasting cognitive impairment. Others may experience lingering cognitive difficulties or a slower return to baseline functioning. Factors like the severity of the underlying illness, the presence of other medical conditions, and the promptness of treatment all play a role in determining the specific outcome.
In some cases, delirium can be a harbinger of more serious health issues.
Long-Term Effects of Dementia
Dementia, in contrast to delirium, is a progressive and irreversible decline in cognitive function. The long-term effects can be devastating, impacting memory, language, problem-solving, and daily functioning. The progression of dementia varies greatly from person to person, impacting individuals differently, and leading to varying degrees of dependency on others. Individuals with dementia may experience increasing difficulties with activities of daily living, eventually needing significant assistance with personal care and daily tasks.
The specific long-term implications also depend on the type of dementia.
Impact on Quality of Life
Both delirium and dementia significantly impact an individual’s quality of life. Delirium can disrupt sleep, increase anxiety, and cause confusion, leading to significant distress for the affected individual and their loved ones. Dementia, due to its progressive nature, can cause isolation, frustration, and fear as cognitive abilities decline. It can also lead to social withdrawal, impacting relationships and social interaction.
The resulting dependence on others can also impact the emotional well-being of the individual and their caregivers.
Support Systems Available
Comprehensive support systems are essential for individuals with delirium and dementia. These systems include medical professionals, family members, caregivers, support groups, and community resources. Early intervention and access to appropriate medical care are crucial for managing delirium. For dementia, support groups, home care services, and specialized memory care facilities can provide vital assistance. These systems are critical in helping individuals maintain a degree of independence and dignity.
Effective Communication Strategies
Effective communication is paramount when interacting with individuals experiencing delirium or dementia. Clear, concise language, a calm and reassuring tone, and visual aids can be highly beneficial. Patience and understanding are crucial. Addressing the individual’s emotional needs, validating their feelings, and avoiding complex or demanding conversations are vital for maintaining positive interactions. Active listening, and focusing on non-verbal cues, can also significantly improve communication.
Examples of Effective Communication Strategies
- Using simple, direct language and avoiding jargon or technical terms.
- Breaking down complex instructions into smaller, manageable steps.
- Using visual aids, such as pictures or diagrams, to enhance understanding.
- Maintaining a calm and reassuring tone of voice.
- Allowing sufficient time for the individual to process information and respond.
- Acknowledging and validating the individual’s feelings and concerns.
Final Wrap-Up

In conclusion, recognizing the distinct features of delirium and dementia is vital for timely intervention. While both can significantly impact daily life, their underlying causes, symptom profiles, and progression vary considerably. This discussion has highlighted the importance of a comprehensive approach to diagnosis, emphasizing the need for a thorough medical history, physical examination, and appropriate diagnostic tools like the Mini-Mental State Examination (MMSE) and Confusion Assessment Method (CAM).
Ultimately, understanding the differences between delirium and dementia empowers healthcare professionals and caregivers to provide the best possible support and treatment.