What is discogenic pain? This deep dive explores the complexities of this often-misunderstood back pain, examining its causes, symptoms, diagnosis, and treatment options. We’ll uncover the anatomical structures involved, the differences between types of discogenic pain, and the various approaches to managing this condition.
Discogenic pain, originating from the spinal discs, can manifest in a range of ways, impacting daily life. From the subtle ache to the debilitating flare-up, understanding its nuances is key to effective management. This comprehensive guide will equip you with the knowledge to navigate the complexities of discogenic pain.
Definition and Overview
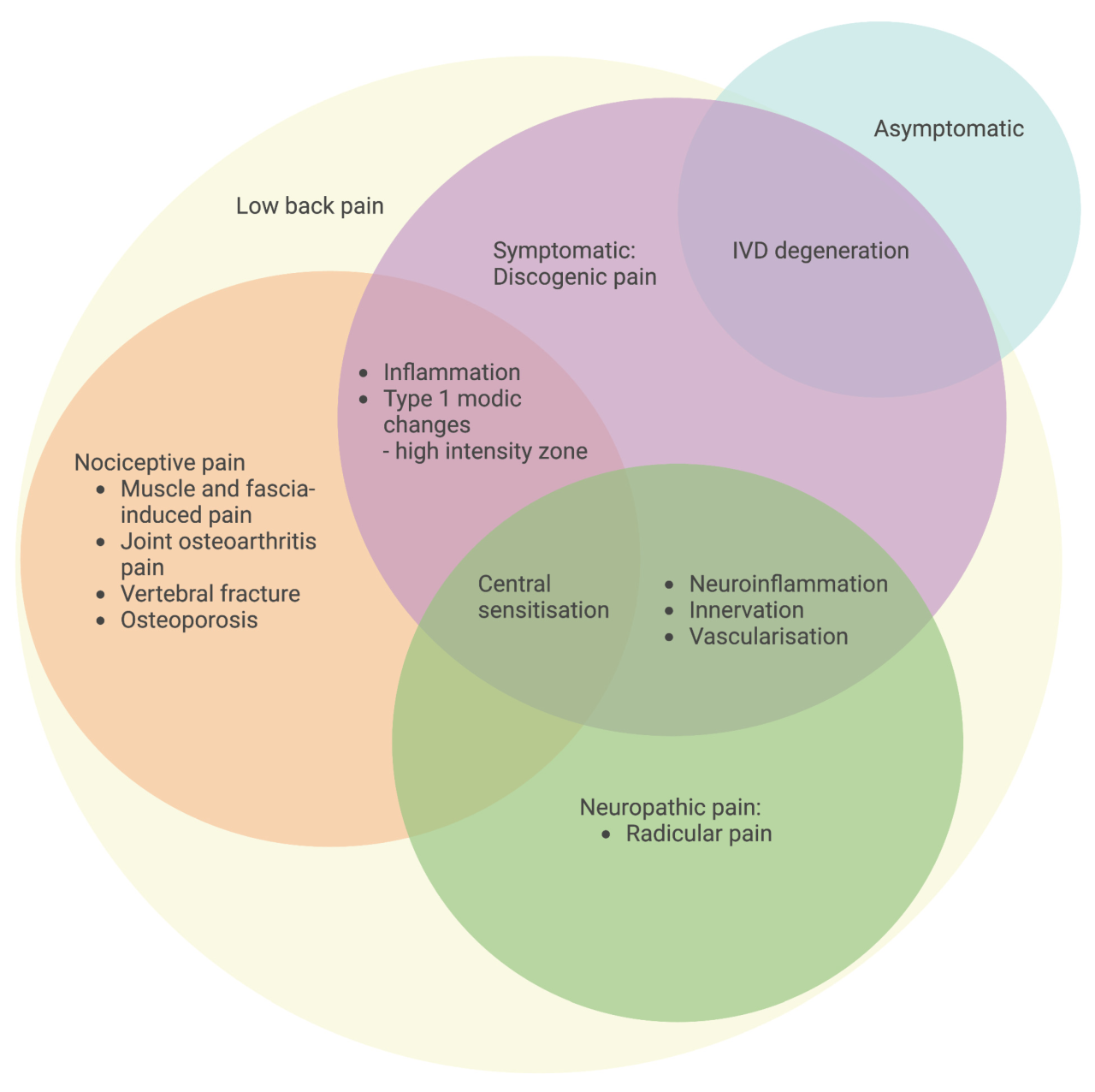
Discogenic pain, a common source of back and neck pain, originates from the intervertebral discs. These discs act as cushions between the vertebrae, enabling movement and absorbing shock. Understanding the structures involved and the various types of discogenic pain is crucial for effective diagnosis and treatment.The intervertebral discs, composed of an outer annulus fibrosus and an inner nucleus pulposus, are susceptible to degeneration and injury.
This damage can lead to inflammation and pain signals that radiate to surrounding tissues and nerves. The pain experienced is often described as deep, aching, or stabbing, and can vary in intensity and location depending on the affected disc and the individual.
Anatomical Structures Involved
The intervertebral discs are crucial components of the spine, providing cushioning and enabling movement. The annulus fibrosus, the outer layer, acts as a tough protective covering, while the nucleus pulposus, the inner gel-like substance, absorbs shock and maintains disc height. Damage or degeneration to these structures can disrupt the normal biomechanics of the spine and trigger pain signals.
Discogenic pain, often stemming from the spine, can be a real challenge. It’s important to find ways to manage the discomfort and improve your quality of life, like exploring resources for wet AMD coping support and living well. Wet AMD coping support and living well can offer valuable insights and strategies for navigating various health conditions.
Ultimately, understanding discogenic pain involves a holistic approach that considers physical and emotional well-being.
Types of Discogenic Pain
Discogenic pain can manifest in various regions of the spine. Lumbar discogenic pain, the most prevalent type, affects the lower back. Cervical discogenic pain, on the other hand, involves the neck region. Thoracic discogenic pain, though less common, can occur in the mid-back. Each type presents unique characteristics and symptoms, making accurate diagnosis essential.
Causes of Discogenic Pain
Several factors can contribute to discogenic pain. These include:
- Degenerative disc disease: A natural aging process that leads to disc breakdown and loss of cushioning properties.
- Disc herniation: A rupture or bulge in the disc, often pressing on nearby nerves.
- Disc prolapse: A more severe form of herniation where the nucleus pulposus protrudes from the annulus fibrosus.
- Disc tear: A tear in the annulus fibrosus, allowing the nucleus pulposus to bulge outward.
- Trauma: Injuries like falls or forceful impacts can cause disc damage.
- Repetitive stress: Activities involving repetitive movements or heavy lifting can strain the discs over time.
- Spinal stenosis: Narrowing of the spinal canal that can put pressure on the discs and nerves.
Diagnostic Tests and Treatment Options
Accurate diagnosis of discogenic pain is crucial for effective treatment. A range of diagnostic tests are employed to identify the source and extent of the problem. Treatment approaches are tailored to the specific cause and severity of the condition.
| Cause | Symptoms | Diagnostic Tests | Treatment Options |
|---|---|---|---|
| Degenerative Disc Disease | Persistent, dull back pain; stiffness; radiating pain; limited range of motion | X-rays, MRI scans, CT scans | Conservative measures (e.g., physical therapy, pain medication, lifestyle modifications); surgical intervention (e.g., spinal fusion) in severe cases. |
| Disc Herniation | Sharp, shooting pain; numbness; tingling; weakness in affected limbs; pain radiating down the leg (sciatica). | MRI scans, CT scans, nerve conduction studies | Conservative measures (e.g., physical therapy, pain medication, epidural injections); surgical intervention (e.g., discectomy) in severe cases. |
| Disc Prolapse | Severe, debilitating pain; loss of bowel or bladder function (rare, but critical); neurological deficits | MRI scans, CT myelograms, electromyography | Immediate medical attention; conservative measures; surgical intervention (e.g., discectomy, laminectomy) if severe nerve compression. |
| Disc Tear | Localized or radiating pain, varying intensity; pain often worsens with specific movements; muscle spasms | MRI scans, CT scans, discography | Conservative measures (e.g., physical therapy, pain medication, activity modification); injections; surgical intervention (e.g., discectomy, fusion) in rare cases. |
Symptoms and Presentation
Discogenic pain, originating from the intervertebral discs, can manifest in a variety of ways, making accurate diagnosis crucial. Understanding the specific symptoms and how they vary based on the affected area is key to effective treatment. This section will delve into the common symptoms, their potential differences, and how they compare to other back pain types.
Common Symptoms of Discogenic Pain
Discogenic pain often presents with a deep, aching sensation that radiates from the affected area. This pain is frequently described as a dull ache or a sharp, stabbing sensation. The pain can be triggered or exacerbated by specific movements, postures, or activities. It’s important to note that the intensity and character of the pain can fluctuate over time, influenced by various factors.
Discogenic pain, essentially pain originating from the discs in your spine, can be a real pain in the neck. Sometimes, managing skin conditions like papulopustular rosacea, a type of facial redness and inflammation, can feel similarly frustrating. Learning how to manage these skin issues, such as how to deal with papulopustular rosacea , can offer a parallel approach to managing the discomfort and symptoms associated with discogenic pain, by focusing on stress reduction and healthy lifestyle choices.
Ultimately, understanding the root cause of discogenic pain, like spinal issues, is key to finding lasting relief.
Variations in Symptoms Based on the Affected Area
The specific location of the affected disc significantly impacts the presentation of symptoms. Pain originating from discs in the lumbar spine (lower back) often radiates into the buttocks and thighs, potentially mimicking sciatica. Cervical disc pain (neck) may lead to pain and numbness in the arms and hands. Thoracic disc pain (mid-back) is less common but can cause localized pain in the chest area, sometimes accompanied by referred pain to the shoulder blades.
Intensities and Durations of Discogenic Pain
The intensity of discogenic pain can range from mild discomfort to severe, debilitating pain. The duration also varies, from intermittent episodes to chronic pain lasting weeks or months. Factors like the severity of the disc injury, individual pain tolerance, and other coexisting conditions can all influence the experience. For example, a sudden, forceful injury may result in immediate and intense pain, while a gradual disc degeneration may cause a more persistent, dull ache over time.
Comparison with Other Back Pain Types
Differentiating discogenic pain from other back pain types is crucial for appropriate treatment. While muscle strains or ligament sprains may also cause localized pain, discogenic pain is often more deeply seated, radiating further from the affected area. Conditions like facet joint syndrome may cause similar pain patterns, requiring careful clinical assessment for proper diagnosis. Spinal stenosis, a narrowing of the spinal canal, might also present with pain that radiates, but it typically worsens with standing or walking.
Table: Symptoms, Descriptions, and Possible Locations of Discogenic Pain
| Symptom | Description | Possible Locations |
|---|---|---|
| Deep, Aching Pain | A persistent, dull ache felt deep within the affected area. | Lower back, neck, mid-back, buttocks, thighs, arms, hands, chest |
| Radiating Pain | Pain that spreads from the initial site to surrounding areas. | Lower back radiating to buttocks and thighs, neck radiating to arms and hands, mid-back radiating to shoulders |
| Numbness or Tingling | A loss of sensation or pins-and-needles feeling in the affected area. | Hands, feet, arms, legs, depending on the nerve root involved |
| Muscle Weakness | Difficulty moving or controlling certain muscles. | Legs, arms, depending on the nerve root involved |
| Limited Range of Motion | Difficulty bending, twisting, or straightening the affected area. | Lower back, neck, mid-back |
Diagnostic Methods
Pinpointing the source of discogenic pain requires a multifaceted approach. A thorough diagnostic evaluation combines patient history, physical examination findings, and appropriate imaging techniques. This process helps differentiate discogenic pain from other conditions with similar symptoms, ensuring accurate treatment and management strategies.
Patient History
A detailed patient history is crucial in evaluating discogenic pain. This involves gathering information about the onset, location, and character of the pain, as well as any contributing factors. Symptoms like radiating pain, numbness, tingling, or muscle weakness are vital indicators. The patient’s medical history, including prior injuries, surgeries, or underlying conditions, should also be carefully documented.
Understanding the patient’s daily activities, posture, and lifestyle choices can provide valuable context to the pain experience. This information helps to narrow down the potential causes and focus diagnostic efforts.
Physical Examination
Physical examination plays a vital role in assessing discogenic pain. This involves a systematic evaluation of the spine and surrounding tissues. Neurological assessments, including sensory and motor function tests, are essential for identifying nerve root impingement. Range of motion (ROM) assessments, palpation, and specific provocative maneuvers help identify painful areas and specific movements that exacerbate the pain.
The physical exam provides objective data to support or refute the suspected diagnosis.
Imaging Techniques
Imaging plays a critical role in evaluating spinal structures and identifying potential sources of discogenic pain. Various imaging techniques are employed to visualize the spine and surrounding tissues.
- Magnetic Resonance Imaging (MRI): MRI is a powerful non-invasive imaging technique that provides detailed cross-sectional images of the spine. It is particularly valuable for assessing the soft tissues, including the intervertebral discs, spinal cord, and nerve roots. MRI can reveal herniated discs, degenerative changes, or other abnormalities that might be contributing to the pain. Examples include visualizing a herniated disc pressing on a nerve root, or identifying stenosis (narrowing) in the spinal canal.
These findings are crucial for guiding treatment decisions.
- Computed Tomography (CT) Scan: CT scans provide detailed anatomical images of the bony structures of the spine. While less sensitive to soft tissue changes compared to MRI, CT scans are helpful in identifying fractures, bony abnormalities, or tumors. They are also beneficial in cases where MRI is contraindicated (e.g., patients with metallic implants). A CT scan can help determine if there’s a bony spur or a fracture compressing the nerve root.
Diagnostic Table
| Diagnostic Method | Description | Advantages | Limitations |
|---|---|---|---|
| Patient History | Gathering information about pain onset, location, and contributing factors. | Identifies potential causes, provides context, and guides further investigation. | Subjective nature of information; reliance on patient recall. |
| Physical Examination | Systematic evaluation of the spine and surrounding tissues, including neurological assessments. | Provides objective data, identifies specific painful areas, and helps determine the affected nerve roots. | Reliance on examiner’s expertise; may not always identify subtle abnormalities. |
| MRI | Detailed cross-sectional images of soft tissues, including intervertebral discs. | Excellent visualization of soft tissues, identifies herniated discs, and detects degenerative changes. | May be contraindicated for patients with metallic implants; can be expensive. |
| CT Scan | Detailed images of bony structures of the spine. | Excellent visualization of bony structures, identifies fractures, and assesses bony abnormalities. | Less sensitive to soft tissue changes compared to MRI; potential for radiation exposure. |
Treatment Strategies
Discogenic pain, stemming from the spine’s intervertebral discs, can significantly impact daily life. Effective treatment often involves a multi-faceted approach, combining conservative strategies with, when necessary, surgical interventions. Understanding the various options available is crucial for managing this condition effectively.
Conservative Treatments, What is discogenic pain
Conservative treatments aim to alleviate pain and improve function without resorting to surgery. These approaches often form the initial line of defense and can be highly effective in many cases. Physical therapy plays a pivotal role in restoring spinal mobility and strengthening supporting muscles. Specific exercises, manual therapy techniques, and modalities like heat or ice can target the affected area, reducing pain and promoting healing.
Medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help manage pain and inflammation. In some cases, stronger pain relievers or muscle relaxants may be necessary, but only under the guidance of a healthcare professional. Careful attention to posture and ergonomics, along with lifestyle modifications, can further reduce stress on the spine.
Surgical Interventions
Surgical interventions for discogenic pain are typically reserved for cases where conservative treatments have failed to provide adequate relief. Discectomy, a common surgical procedure, involves the removal of the damaged portion of the disc. This procedure aims to alleviate pressure on the spinal nerves, thereby reducing pain. Spinal fusion, another surgical option, involves joining two or more vertebrae together.
This procedure stabilizes the spine, potentially eliminating pain and restoring spinal integrity. The choice between discectomy and fusion depends on the specific nature of the injury and the patient’s overall condition. Careful consideration and discussion with a qualified spine surgeon are essential in determining the most appropriate course of action.
Lifestyle Modifications
Lifestyle modifications can significantly impact the management of discogenic pain. Maintaining a healthy weight can reduce the strain on the spine. Regular exercise, particularly low-impact activities like swimming or walking, can strengthen core muscles and improve spinal stability. Proper posture, both during work and leisure activities, is paramount. Ergonomic adjustments in the workplace or at home can significantly reduce stress on the spine.
Smoking cessation and stress reduction techniques, such as meditation or yoga, can also play a crucial role in promoting overall well-being and minimizing the risk of further spinal problems.
Treatment Options Table
| Treatment Type | Description | Effectiveness |
|---|---|---|
| Physical Therapy | Includes exercises, manual therapy, and modalities to improve spinal mobility, strengthen supporting muscles, and reduce pain. | Generally effective in reducing pain and improving function, especially in combination with other treatments. |
| Medications (NSAIDs, etc.) | Nonsteroidal anti-inflammatory drugs (NSAIDs) and other pain relievers help manage pain and inflammation. | Effective in reducing pain and inflammation for many patients. Effectiveness varies depending on the individual and the severity of the condition. |
| Discectomy | Surgical removal of the damaged portion of the intervertebral disc to relieve pressure on spinal nerves. | Potentially highly effective in relieving pain for patients with specific types of disc herniations or bulges causing significant nerve impingement. Success rates can vary depending on factors like the patient’s overall health and the specific nature of the injury. |
| Spinal Fusion | Surgical joining of two or more vertebrae to stabilize the spine and potentially eliminate pain. | Effective in stabilizing the spine and reducing pain for patients with significant instability or degeneration. Recovery time can be longer compared to discectomy. |
| Lifestyle Modifications | Maintaining a healthy weight, regular exercise, good posture, and stress management can significantly reduce the stress on the spine and improve overall well-being. | While not a direct treatment for the pain itself, lifestyle modifications are crucial for long-term management and prevention of future problems. |
Risk Factors and Prevention: What Is Discogenic Pain
Discogenic pain, stemming from issues with the spinal discs, can significantly impact daily life. Understanding the risk factors associated with this condition is crucial for proactive prevention. By recognizing potential triggers and adopting preventive measures, individuals can minimize their likelihood of experiencing this debilitating pain.
Identifying Risk Factors
Several factors can increase the risk of developing discogenic pain. These factors are often interconnected, highlighting the importance of a holistic approach to preventing this condition. A combination of lifestyle choices and inherent predispositions can contribute to the development of discogenic pain.
- Age: The risk of disc degeneration increases with age, as the discs naturally lose water content and become less resilient. This age-related deterioration is a common factor in the development of discogenic pain, particularly in individuals over 40.
- Genetics: A family history of back problems or disc degeneration can increase an individual’s susceptibility to discogenic pain. Inherited traits can influence the structure and function of the spine, making some people more prone to disc-related issues.
- Repetitive Stress: Jobs or activities involving repetitive movements, especially those that strain the back, can put significant stress on the spinal discs. Examples include manual labor, prolonged sitting, and certain sports.
- Obesity: Excess weight puts added pressure on the spine, potentially leading to disc degeneration and pain. Maintaining a healthy weight is crucial in protecting the spinal discs from excessive strain.
- Poor Posture: Slouching or maintaining poor posture throughout the day can lead to misalignment of the spine and increased pressure on the discs. This poor posture is a major risk factor, particularly in individuals who spend prolonged periods sitting or standing in awkward positions.
- Improper Lifting Techniques: Lifting heavy objects without using proper techniques can cause significant strain on the spinal discs. This can lead to herniations or other disc-related problems.
- Smoking: Smoking is associated with reduced blood flow to the spinal discs, potentially contributing to their degeneration and increasing the risk of discogenic pain. This effect has been observed in various studies and can affect the health of the entire body.
Maintaining Good Posture and Lifting Techniques
Maintaining good posture is essential for protecting the spinal discs. Slouching and poor posture put undue pressure on the discs, increasing the risk of injury and pain. Proper lifting techniques are equally important. These techniques ensure the load is distributed evenly across the body’s core, reducing stress on the spine and minimizing the risk of injury.
- Posture Awareness: Regularly reminding oneself to maintain good posture throughout the day is crucial. This can be achieved through conscious effort and periodic checks, ensuring proper spinal alignment.
- Ergonomic Workspace: Adjusting the workspace to support good posture is important. Using appropriate chairs, desks, and monitor positions are critical components of a healthy workspace.
- Lifting Techniques: When lifting, use your legs, not your back. Keep the load close to your body and maintain a straight back. Avoid twisting while lifting.
Regular Exercise and Healthy Weight
Regular exercise strengthens the muscles supporting the spine, improving stability and reducing the risk of injury. Maintaining a healthy weight helps to reduce the strain on the spinal discs. This is an important preventative measure for individuals at risk.
- Strengthening Exercises: Exercises targeting core muscles, back muscles, and other supportive muscles can significantly improve spinal stability.
- Cardiovascular Activity: Cardiovascular exercise contributes to overall health and can help maintain a healthy weight.
- Weight Management: Maintaining a healthy weight reduces the load on the spine and helps prevent disc degeneration.
Illustrative Case Studies
Understanding discogenic pain requires delving into real-world examples. These case studies highlight the diverse presentations, diagnostic challenges, and treatment outcomes associated with this condition. By examining individual experiences, we can gain a deeper appreciation for the complexities of discogenic pain and the importance of a tailored approach to diagnosis and management.
Discogenic pain, often stemming from the spine, can be a real pain in the neck. Sometimes, hormonal imbalances, like those related to androgens and PCOS excess levels, androgens and pcos excess levels what it means , can indirectly affect the spine, contributing to the overall discomfort. Understanding the underlying causes is crucial for effective management of discogenic pain.
Case Study Examples
These case examples demonstrate the spectrum of discogenic pain, emphasizing the variability in symptom presentation, diagnostic difficulty, and treatment response. Each case illustrates a different facet of the condition, from the relatively straightforward to the more intricate scenarios.
| Case ID | Patient Profile | Symptoms | Diagnosis | Treatment |
|---|---|---|---|---|
| 1 | A 45-year-old female, sedentary office worker. Reports a history of back pain for 6 months, gradually worsening. | Low back pain, radiating to the left buttock and thigh, worsened by prolonged standing or sitting, and relieved by lying down. Associated with occasional numbness and tingling in the left leg. | Discogenic pain, likely from a herniated disc in the lumbar spine. MRI confirmed a small posterior disc herniation at L4-L5. | Conservative management including physical therapy focused on core strengthening and posture correction, anti-inflammatory medication, and epidural steroid injections. The patient reported significant improvement within 8 weeks. |
| 2 | A 28-year-old male, construction worker, experiencing acute back pain after lifting a heavy object. | Severe, localized low back pain, sharp and stabbing, with immediate onset. Limited range of motion, inability to stand upright. | Discogenic pain likely caused by a facet joint strain, aggravated by the forceful movement. No obvious disc herniation on initial imaging. | Initial pain management with rest, ice, and over-the-counter analgesics. Followed by physical therapy to restore spinal mobility and strength. The patient recovered within 6 weeks, returning to work without limitations. |
| 3 | A 62-year-old female, experiencing persistent back pain for 12 months. Reports worsening pain over time, accompanied by stiffness and limited mobility. | Chronic, dull aching low back pain, worse in the morning. Progressive loss of mobility, with pain extending to the hips. Associated with a feeling of weakness in the lower extremities. | Discogenic pain secondary to degenerative disc disease. MRI revealed significant disc degeneration and facet joint osteoarthritis at L3-L4. | Multimodal approach including physical therapy, medication for pain and inflammation, and spinal injections for pain relief. Patient experienced some improvement in pain and mobility but not a complete resolution. |
Diagnostic Challenges in Discogenic Pain
Diagnosing discogenic pain can be challenging due to the overlapping symptoms with other musculoskeletal conditions. Precise identification often requires a careful history, physical examination, and various imaging techniques. Radiographic findings may not always correlate directly with the patient’s symptoms, requiring further evaluation and potentially more advanced diagnostic tools like discography.
Treatment Outcomes
Treatment outcomes for discogenic pain vary depending on the severity, underlying cause, and the individual patient’s response. Conservative management, including physical therapy, medication, and injections, often yields positive results for milder cases. Surgical intervention might be considered for more severe or persistent cases unresponsive to conservative measures.
Prognosis and Long-Term Management

Discogenic pain, while often manageable, can significantly impact a person’s quality of life. Understanding the expected trajectory of the condition and implementing effective long-term strategies are crucial for achieving optimal outcomes. This section delves into the prognosis, the importance of ongoing management, and the vital role of patient education and support.The prognosis for discogenic pain varies considerably depending on several factors, including the severity of the underlying condition, the individual’s response to treatment, and their commitment to long-term management strategies.
In many cases, pain can be significantly reduced or even eliminated, leading to improved function and a better overall quality of life. However, some individuals may experience persistent pain, necessitating ongoing management and adjustments to lifestyle.
Expected Prognosis
The expected prognosis for discogenic pain depends on several key factors, including the severity of the disc degeneration, the presence of other underlying conditions, and the effectiveness of treatment. Early intervention and adherence to a comprehensive treatment plan can lead to significant improvement, often with pain reduction and restoration of function. However, some individuals may experience persistent pain, requiring ongoing management and lifestyle modifications.
Individual responses to treatment vary, making it challenging to predict the exact course of the condition.
Importance of Long-Term Management
Long-term management of discogenic pain is essential to prevent recurrence and maintain a high quality of life. This approach involves a multifaceted strategy that addresses the underlying causes of pain, promotes healing, and educates the patient on self-management techniques. Regular monitoring and adjustments to treatment plans are necessary to adapt to the individual’s evolving needs and response to interventions.
A proactive approach can significantly reduce the likelihood of future flare-ups and improve long-term outcomes.
Role of Patient Education and Support Groups
Patient education plays a critical role in the long-term management of discogenic pain. Understanding the condition, its triggers, and effective coping mechanisms empowers patients to actively participate in their recovery. Support groups provide a platform for individuals to share experiences, exchange information, and offer mutual support. These networks can be invaluable resources for fostering a sense of community and encouraging adherence to treatment plans.
Strategies to Prevent Recurrence
Preventing recurrence of discogenic pain necessitates a proactive approach that addresses lifestyle factors, maintains a healthy weight, and promotes good posture. Regular exercise, particularly activities that strengthen core muscles, is essential for spinal stability and reducing the risk of further injury. Maintaining a healthy diet and managing stress levels are also critical components of a comprehensive preventative strategy.
Addressing potential triggers and developing coping mechanisms are also essential for preventing recurrence.
Successful Long-Term Management Strategies for Specific Patient Groups
Successful long-term management strategies vary based on individual needs and circumstances. For example, patients with sedentary lifestyles may benefit from specific exercises and ergonomic adjustments at work or home. Those with pre-existing medical conditions may require personalized strategies that take into account their specific needs. Individuals with a history of back injuries may require a more cautious approach to physical activity and a focus on maintaining core strength.
Final Conclusion
In conclusion, discogenic pain, while challenging, is manageable. A thorough understanding of its causes, symptoms, diagnostic methods, and treatment options empowers individuals to take an active role in their recovery. By combining medical guidance with lifestyle adjustments, effective strategies can be implemented to alleviate pain and improve long-term well-being.

