What are herniated disc symptoms? This comprehensive guide delves into the various ways a herniated disc can manifest, from common pain to more complex complications. Understanding these symptoms is crucial for early diagnosis and effective management.
Herniated discs occur when the soft inner material of a spinal disc bulges or ruptures, putting pressure on surrounding nerves. This pressure can lead to a range of symptoms, and their severity can vary greatly depending on the location and extent of the herniation. This article explores the common signs, how symptoms differ depending on the affected area of the spine, and the potential complications of a herniated disc.
Introduction to Herniated Discs
A herniated disc, also known as a slipped disc, occurs when the soft, gel-like center of an intervertebral disc (the cushions between the vertebrae in your spine) bulges or ruptures through the tough outer layer. This can put pressure on nearby nerves, leading to pain, numbness, and other symptoms. Understanding the anatomy of the spine and the discs themselves is crucial to comprehending this condition.The intervertebral discs act as shock absorbers, allowing for flexibility and movement while protecting the spinal cord and nerves.
Each disc is composed of a tough outer layer called the annulus fibrosus and a softer, inner nucleus pulposus. A herniation happens when the nucleus pulposus protrudes or breaks through the annulus fibrosus, often due to injury or wear and tear.
Types of Herniated Discs and Potential Causes
Herniated discs can be categorized based on the direction of the herniation and the affected area of the spine. Common types include posterolateral herniations, which are the most frequent, and involve a bulge or rupture of the disc material posteriorly and laterally, pressing on the nerves. Other types include anterior, posterior, and lateral herniations, each potentially impacting different nerve roots.Causes of herniated discs are often multifactorial, encompassing both acute trauma and chronic degenerative processes.
Acute injuries, like a sudden twisting motion or a heavy lift, can directly cause a herniation. Chronic conditions, like osteoarthritis, can weaken the disc over time, increasing the risk of a herniation. Furthermore, factors such as poor posture, obesity, and repetitive strain injuries can contribute to the development of herniated discs.
Risk Factors for Herniated Discs
Several factors increase an individual’s susceptibility to herniated discs. Age is a significant factor, as discs naturally weaken and dehydrate with time. People in physically demanding occupations, such as construction workers or athletes, are at higher risk due to the repetitive stress and strain on the spine. Genetics also plays a role, as some individuals may inherit a predisposition to weaker discs.
A sedentary lifestyle, coupled with poor posture, can contribute to the development of herniated discs. Smoking, for instance, can reduce blood flow to the discs, potentially accelerating degeneration.
Structure and Function of the Spine, What are herniated disc symptoms
The spine is a complex structure composed of vertebrae, discs, and ligaments, working together to support the body and facilitate movement. Understanding the different parts of the spine and their roles is essential for comprehending herniated disc conditions.
| Spine Region | Vertebrae Count | Role in Body Support | Potential Herniation Impact |
|---|---|---|---|
| Cervical Spine (Neck) | 7 | Supports the head and neck; facilitates movement and flexibility | Can affect nerves controlling the arms and hands, leading to numbness and pain |
| Thoracic Spine (Upper Back) | 12 | Provides stability and support for the upper body; connects the neck to the lower back | Can affect nerves supplying the chest and upper abdomen |
| Lumbar Spine (Lower Back) | 5 | Supports the majority of the body weight; facilitates movement and flexibility, especially in the sagittal plane | Most commonly affected region; can cause pain radiating down the legs (sciatica) |
| Sacrum and Coccyx | 5 fused vertebrae (sacrum), 4 fused vertebrae (coccyx) | Forms the base of the spine, transferring weight to the pelvis; provides stability for sitting and standing | Herniations are less common in this area |
Common Symptoms
Herniated discs, a common spinal condition, manifest in a range of symptoms, often varying in intensity and location depending on the affected area and the severity of the herniation. Understanding these symptoms is crucial for early diagnosis and appropriate treatment. Accurate identification allows for targeted interventions, improving the quality of life for those affected.Herniated discs, a common spinal condition, often result in pain, numbness, or tingling in the affected area.
The precise nature of the symptoms depends on the location and size of the herniation. For example, a herniation in the lower back might primarily cause pain in the buttocks and legs, whereas a herniation in the neck might manifest as pain and numbness in the arms and hands. The severity of the symptoms can also vary greatly. Some individuals experience mild discomfort, while others may experience debilitating pain that significantly impacts their daily activities.
Frequency and Variation of Symptoms
Symptoms of herniated discs are not uniform. They can range from mild discomfort to severe pain, and their location and nature often depend on the specific location of the herniated disc within the spine. A herniated disc in the lumbar region, for instance, typically leads to lower back pain radiating down the leg. This pain may be accompanied by numbness or tingling, and may worsen with activities like bending, lifting, or prolonged standing.
Conversely, a herniated disc in the cervical spine might cause neck pain that extends to the shoulder and arm, often accompanied by numbness or weakness in the hand.
Comparison with Other Spinal Conditions
Differentiating herniated disc symptoms from those of other spinal conditions can be challenging. While a herniated disc often presents with pain radiating to the extremities, other conditions like spinal stenosis or osteoarthritis can also cause similar symptoms. Careful examination, including a detailed medical history and physical assessment, is necessary to arrive at a precise diagnosis.
Herniated Disc vs. Sciatica
| Symptom | Herniated Disc | Sciatica | Comparison |
|---|---|---|---|
| Pain Location | Lower back, radiating to buttock and leg | Buttock and leg, typically following the sciatic nerve | Often overlapping, but sciatica specifically involves the sciatic nerve. |
| Numbness/Tingling | Possible, often in the same area as pain | Common, following the sciatic nerve’s path | Both conditions can cause numbness and tingling. |
| Muscle Weakness | Possible, in the affected leg or foot | Possible, in the affected leg or foot | Both can cause weakness, but this is less common than pain. |
| Aggravating Factors | Lifting, bending, prolonged standing | Certain movements, especially those affecting the sciatic nerve | Both conditions can be worsened by specific activities. |
Comparing the symptoms of a herniated disc with those of sciatica reveals notable overlaps. Sciatica, a common condition, is characterized by pain radiating along the sciatic nerve, often originating from the lower back. While the pain locations may overlap, sciatica is specifically linked to irritation of the sciatic nerve, which may or may not be caused by a herniated disc.
Common Pain Locations
Common pain locations associated with herniated discs include the lower back, radiating down one or both legs. The pain may be sharp, stabbing, or a dull ache. In the cervical spine, pain may radiate to the shoulder, arm, and hand. Numbness and tingling are frequently reported alongside the pain, and these sensations can follow the same pattern as the pain itself.
The location of the pain and its associated symptoms are crucial for diagnosis.
Symptoms by Location
Herniated discs aren’t a one-size-fits-all condition. The specific location of the herniation significantly impacts the type and intensity of symptoms experienced. Understanding where the disc is bulging or pressing on nerves provides crucial clues for diagnosis and treatment. Different nerves in the spine control various parts of the body, leading to location-specific pain patterns.The location of the herniated disc directly correlates with the area of the body that experiences pain and other symptoms.
This correlation is a key element in accurately diagnosing and treating the condition. Recognizing the specific nerve pathways affected by the herniation is critical for effective management and alleviation of discomfort.
Cervical Region Symptoms
Cervical herniations, occurring in the neck region, often manifest as pain radiating down the arm, potentially affecting the shoulder, elbow, forearm, and hand. Numbness or tingling (paresthesia) in these areas are also common. Weakness in the hand or arm muscles can occur, making everyday tasks challenging. Sometimes, symptoms might include headaches, dizziness, or vision problems. The pain can be sharp or dull, and often worsens with certain movements or activities.
Lumbar Region Symptoms
Lumbar herniations, located in the lower back, are frequently associated with lower back pain. This pain can range from a mild ache to a severe, stabbing sensation. The pain frequently radiates down one or both legs, following the sciatic nerve path. Symptoms such as numbness, tingling, or weakness in the legs, buttocks, or feet are common. Individuals may experience difficulty with walking, bending, or lifting.
Thoracic Region Symptoms
Herniations in the thoracic spine, located in the mid-back, are less common than those in the cervical or lumbar regions. However, when they do occur, they can still produce a variety of symptoms. Pain in the mid-back, radiating to the chest, abdomen, or even the groin, might be experienced. Numbness or tingling sensations in the upper body, including the chest, abdomen, and groin, can also accompany thoracic herniations.
These symptoms are generally less pronounced than those seen in cervical or lumbar herniations.
Symptom Patterns by Spinal Location
| Spinal Region | Common Symptoms | Nerve Affected | Body Areas Affected |
|---|---|---|---|
| Cervical (Neck) | Neck pain, arm pain, numbness/tingling in arm/hand, weakness in arm/hand, headaches, dizziness | Cervical nerves | Neck, shoulder, arm, hand, potentially head |
| Lumbar (Lower Back) | Lower back pain, leg pain (sciatica), numbness/tingling in leg/foot, weakness in leg/foot, difficulty walking/bending | Sciatic nerve (and lumbar nerves) | Lower back, buttock, leg, foot |
| Thoracic (Mid-Back) | Mid-back pain, radiating pain to chest, abdomen, or groin, numbness/tingling in chest, abdomen, or groin | Thoracic nerves | Mid-back, chest, abdomen, groin |
Severity and Progression of Symptoms
Herniated discs, while often painful, don’t always follow a predictable course. The severity of symptoms can vary greatly from person to person, and even within the same individual over time. Understanding how symptoms progress is crucial for managing expectations and developing effective treatment strategies.The experience of a herniated disc is highly individualized. Some individuals might experience debilitating pain that significantly impacts their daily lives, while others might only have mild discomfort that resolves without intervention.
Factors such as the size and location of the herniated disc, the individual’s overall health, and their lifestyle all play a role in shaping the severity and progression of symptoms.
Factors Influencing Symptom Progression
The path of a herniated disc’s impact on a person’s well-being is influenced by several key elements. These factors include the degree of nerve compression, the presence of inflammation, the individual’s overall health, and lifestyle choices. Maintaining a healthy weight, engaging in regular exercise, and adopting good posture can all contribute to managing symptoms and preventing further complications.
Conversely, factors like prolonged periods of inactivity, poor posture, or lifting heavy objects can exacerbate symptoms and prolong the healing process.
Potential for Spontaneous Resolution
While medical intervention is often necessary for severe cases, it’s important to acknowledge the potential for herniated disc symptoms to resolve spontaneously, without any specific treatment. In some instances, the body’s natural healing processes can effectively reduce inflammation and alleviate pressure on the affected nerves. This is more likely in cases with milder herniations and where the individual maintains a healthy lifestyle.
So, you’re dealing with those nagging back pain symptoms? Herniated discs can cause a whole host of issues, from sharp shooting pains down your leg to a general feeling of stiffness. Sometimes, the pain can be easily mistaken for something else, like a stress fracture, which is a tiny crack in a bone, often caused by overuse. If you’re unsure about the cause, it’s always best to check in with a medical professional to pinpoint the exact problem.
Understanding the difference between these issues is key to getting the right treatment, so make sure to research what is a stress fracture as well. Ultimately, knowing the signs of a herniated disc is crucial for seeking timely and effective care.
However, this does not mean that proactive medical consultation is unnecessary. Consulting a healthcare professional is crucial to ensure an accurate diagnosis and to rule out any underlying conditions that might be contributing to the symptoms.
Herniated discs can cause a range of symptoms, from mild back pain to more debilitating nerve pain. Understanding how pain management strategies like adjuvant analgesics can help alleviate the discomfort is crucial. For example, learning more about what are adjuvant analgesics can provide insights into how these medications complement other pain relievers to manage the specific pain associated with herniated discs.
Ultimately, knowing the various symptom presentations and treatment options is key to navigating this condition effectively.
Severity Levels and Impact on Daily Activities
Understanding the different severity levels of herniated disc symptoms can help patients and healthcare providers anticipate potential impacts on daily activities. The following table provides a general overview, but individual experiences may vary.
| Severity Level | Description | Impact on Daily Activities | Potential for Spontaneous Resolution |
|---|---|---|---|
| Mild | Symptoms are infrequent and manageable, potentially resolving with over-the-counter pain relief. | Minimal to no disruption of daily activities. Slight discomfort during certain movements. | High |
| Moderate | Symptoms are more frequent and intense, requiring regular pain management. | Some limitations in daily activities, such as difficulty with lifting, prolonged sitting, or standing. Potential for reduced mobility. | Moderate |
| Severe | Symptoms are persistent and debilitating, significantly impacting daily life and requiring significant pain management. | Significant limitations in daily activities, including difficulty with basic movements and personal care. Potential for reduced work productivity and social interaction. | Low |
| Critical | Symptoms are severe and life-threatening, requiring immediate medical attention. | Complete inability to perform daily activities, including loss of bladder or bowel control. | None |
Associated Symptoms and Complications: What Are Herniated Disc Symptoms
A herniated disc isn’t just about pain; it can trigger a cascade of other symptoms and potential complications. Understanding these associated issues is crucial for effective management and seeking timely medical attention. Recognizing the range of symptoms and potential problems allows for a more holistic approach to recovery.
Other Accompanying Symptoms
Beyond the primary pain, a herniated disc can manifest with various accompanying symptoms. These often depend on the location of the herniation and the nerves affected. Numbness, tingling, and weakness are common sensations, often radiating along the nerve pathways. For instance, a herniated disc in the lower back might cause numbness and tingling in the leg or foot, while one in the neck could lead to similar symptoms in the arm or hand.
Potential Complications
Herniated discs can lead to more serious issues if left untreated or if the herniation is severe. Nerve damage, a significant complication, can result in permanent loss of function if not addressed promptly. This damage can manifest as persistent numbness, tingling, or weakness, making everyday tasks challenging. Muscle atrophy, or the shrinking of muscles, is another possible complication.
This occurs due to prolonged nerve compression, reducing muscle strength and potentially leading to functional limitations.
Chronic Pain
A herniated disc can contribute to the development of chronic pain. The initial pain may subside, but lingering discomfort can persist, affecting quality of life. The pain can cycle, becoming worse with certain activities or movements. Chronic pain can be a complex issue, often requiring a multidisciplinary approach to pain management.
Situations Requiring Medical Attention
There are specific situations where herniated disc symptoms warrant immediate medical attention. Sudden and severe pain, particularly if accompanied by weakness or numbness in a limb, requires prompt medical evaluation. Loss of bowel or bladder control is a critical sign of severe nerve compression and needs immediate medical intervention. Progressive worsening of symptoms, such as increasing numbness or weakness, necessitates a doctor’s visit to rule out more serious conditions.
Summary of Potential Complications
| Potential Complications | Symptoms | Examples | Importance |
|---|---|---|---|
| Nerve Damage | Persistent numbness, tingling, weakness, muscle atrophy | Inability to lift objects, reduced hand grip strength | Can lead to permanent functional limitations if untreated. |
| Muscle Atrophy | Progressive loss of muscle mass and strength | Difficulty walking, reduced arm strength | Often a result of prolonged nerve compression. |
| Chronic Pain | Lingering discomfort, pain cycles | Pain that persists after initial injury, exacerbating with certain movements | Can significantly impact quality of life, requiring comprehensive pain management. |
| Severe Nerve Compression | Loss of bowel or bladder control, sudden severe pain, accompanied by weakness or numbness in a limb. | Inability to control urination or bowel movements, sudden and severe back pain radiating down the leg | Requires immediate medical attention to prevent permanent nerve damage. |
Diagnosing Herniated Disc Symptoms
Identifying a herniated disc involves a multi-faceted approach, combining patient history, physical examination, and often, medical imaging. A thorough evaluation helps pinpoint the source of the pain and guide appropriate treatment strategies. The diagnostic process aims to distinguish a herniated disc from other potential causes of back pain, ensuring accurate and timely intervention.
Medical History and Physical Examination
A detailed medical history plays a crucial role in diagnosing a herniated disc. This includes inquiries about the onset, location, and character of the pain, as well as any associated symptoms. The history should also explore any pre-existing medical conditions, recent injuries, or lifestyle factors that might contribute to the problem. A physical examination is equally important.
This involves assessing range of motion, muscle strength, and neurological function, such as reflexes and sensation. The examination helps to pinpoint the specific area of the spine affected and identify any neurological deficits. A thorough physical exam helps to identify the patterns of pain, numbness, or weakness. A careful assessment of the patient’s posture, gait, and movements can also reveal subtle indicators.
Role of Medical Imaging
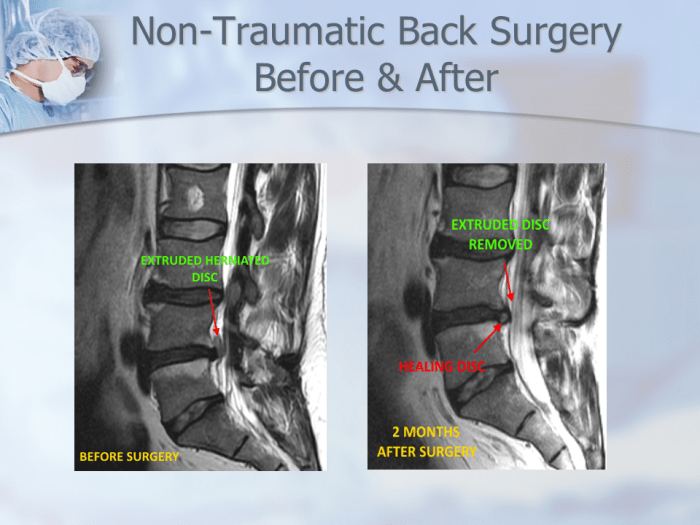
Medical imaging, particularly Magnetic Resonance Imaging (MRI), is essential in diagnosing herniated discs. MRI scans provide detailed cross-sectional views of the spine, allowing visualization of the spinal cord, nerve roots, and surrounding tissues. This helps to pinpoint the location and extent of any disc herniation. While X-rays can reveal bone structure abnormalities, they aren’t as effective in visualizing soft tissues like the intervertebral discs.
MRI is superior for this purpose. CT scans, while also showing bony structures, are less helpful in identifying soft tissue herniations.
Diagnostic Tests
A range of diagnostic tests may be employed to further investigate the condition. These tests aim to confirm the presence of a herniated disc and rule out other potential causes of back pain. Electromyography (EMG) and nerve conduction studies can evaluate the function of the nerves, which is crucial to determine if nerve compression is present. These studies can identify potential nerve root impingement, a key indicator of herniated disc.
Table of Diagnostic Tests
| Diagnostic Test | Procedure | Purpose | Implications |
|---|---|---|---|
| Magnetic Resonance Imaging (MRI) | A non-invasive scan using powerful magnets and radio waves to create detailed images of the spine. | Identifies the location, size, and extent of the herniation, and any associated spinal cord or nerve root compression. | Provides detailed anatomical information, allowing for precise diagnosis and guiding treatment decisions. |
| Computed Tomography (CT) Scan | Uses X-rays to create detailed cross-sectional images of the spine. | Evaluates bone structure and bony abnormalities, and can help in detecting fractures or other bony issues. | Less effective in visualizing soft tissues like discs compared to MRI. |
| Electromyography (EMG) | A test that measures the electrical activity in muscles. | Evaluates nerve function and detects nerve damage or compression. | Provides important information about nerve root impingement, which can indicate a herniated disc. |
| Nerve Conduction Studies | Measures the speed at which electrical signals travel along nerves. | Assesses nerve function and identifies any abnormalities in nerve conduction velocity. | Helps in identifying nerve root compression, a key feature of herniated discs. |
Differentiating from Other Conditions
Pinpointing the precise cause of back pain is crucial for effective treatment. Many conditions can mimic the symptoms of a herniated disc, making accurate diagnosis essential. Understanding these similarities and differences allows for a more targeted approach to care.Accurate diagnosis is paramount to avoid misdiagnosis and inappropriate treatment. Ignoring or misinterpreting symptoms can delay appropriate intervention and hinder recovery.
A comprehensive evaluation, considering various factors beyond just pain, is critical to differentiating between a herniated disc and other possible causes of back pain.
Herniated disc symptoms can range from mild aches to debilitating pain, often radiating down the arm or leg. Understanding these symptoms is crucial for proper diagnosis, and sometimes, the color of your inhaler can be equally important! For instance, knowing what the different inhaler colors mean can help you manage your breathing conditions effectively. Refer to this informative guide on inhaler colors what do they mean to learn more about the various colors and their corresponding medications.
Ultimately, recognizing these symptoms early and seeking professional medical advice is key to managing any herniated disc issues.
Conditions Sharing Similar Symptoms
Several spinal conditions, alongside other non-spinal issues, can produce symptoms that overlap with those of a herniated disc. Careful consideration of the patient’s medical history, physical examination findings, and diagnostic tests is necessary to distinguish between these conditions.
Differentiating Factors
Distinguishing between a herniated disc and other spinal issues often involves analyzing the specific characteristics of the pain, such as its location, radiation pattern, and associated symptoms. For instance, pain radiating down the leg (sciatica) is a hallmark of a herniated disc, but similar pain can also arise from other conditions.
Comparing Herniated Discs to Other Potential Causes of Back Pain
| Condition | Symptoms | Location | Other Characteristics |
|---|---|---|---|
| Herniated Disc | Sharp, shooting pain radiating down the leg (sciatica), numbness, tingling, weakness in the leg, pain worsened by movement, bending, or lifting. | Typically localized in the lower back, but pain can radiate to the buttock, thigh, and leg. | May exhibit pain that increases with prolonged standing or sitting, and decreased with bending forward. Often associated with a specific trigger, like lifting a heavy object. |
| Spinal Stenosis | Pain, numbness, and weakness in the legs, typically worsened by walking and relieved by sitting. | Can affect the entire spine, but commonly presents in the lower back or neck. | Pain often described as cramping or a burning sensation in the legs. Neurological symptoms may be more prominent. Symptoms often worsen with activity and improve with rest. |
| Spondylosis | Stiffness, aching pain in the back, especially in the morning, and reduced range of motion. | Can occur throughout the spine, with lower back involvement being common. | Usually progressive, and symptoms tend to worsen over time. Often associated with age-related degeneration. Pain is typically more persistent and less acutely related to specific movements. |
| Muscle Strain | Localized muscle pain, stiffness, and tenderness in the back. | Localized to the specific strained muscle groups. Pain often worsens with activity. | Often results from overuse, poor posture, or improper lifting techniques. Pain is typically not accompanied by radiating symptoms like numbness or tingling. |
| Facet Joint Syndrome | Deep, aching pain localized to the lower back, often exacerbated by movement. | Pain often centered around the affected facet joints in the spine. | Pain may be worse when twisting or bending the spine, or in certain positions. The pain may be accompanied by stiffness. |
Importance of Accurate Diagnosis
A precise diagnosis is crucial for effective treatment. Incorrect identification of the cause of back pain can lead to ineffective interventions and prolonged discomfort. A multifaceted approach that combines patient history, physical examination, and diagnostic imaging is vital. This ensures that the appropriate treatment plan is implemented for the specific underlying condition.
Managing Herniated Disc Symptoms
Dealing with a herniated disc can be a challenging experience, often impacting daily activities and quality of life. Effective management hinges on understanding the available options, ranging from conservative treatments to surgical interventions. This section will explore various methods for managing herniated disc symptoms, from physical therapy to surgical procedures and recovery.Conservative management strategies, often the first line of defense, aim to alleviate pain and improve function without resorting to surgery.
These methods frequently involve a combination of approaches, tailored to the individual’s specific needs and the severity of the herniation.
Non-Surgical Management Methods
Conservative treatments are typically employed to reduce pain, inflammation, and promote healing. These methods aim to strengthen the supporting muscles around the spine, improve posture, and minimize stress on the affected area. This often involves a combination of approaches.
- Physical Therapy: A crucial aspect of non-surgical management, physical therapy involves exercises, stretches, and manual techniques to improve spinal mobility, reduce pain, and strengthen core muscles. A skilled physical therapist can create a customized program to address specific needs and limitations.
- Medications: Pain relievers, such as over-the-counter ibuprofen or stronger prescription medications, can help manage pain and inflammation. These may be accompanied by muscle relaxants to reduce spasms. However, it is essential to consult with a doctor before taking any medication, especially if there are pre-existing conditions or concerns about potential side effects.
- Lifestyle Modifications: Maintaining a healthy weight, practicing good posture, and avoiding activities that exacerbate pain are crucial for managing herniated disc symptoms. This includes ergonomic adjustments in the workplace and at home to reduce strain on the spine. For instance, using a supportive chair and proper lifting techniques can significantly decrease the risk of further injury.
- Heat and Cold Therapy: Applying heat or ice packs can help reduce pain and inflammation. Heat can relax muscles, while ice can numb the area and reduce swelling. These are often used in conjunction with other treatments.
Surgical Intervention
Surgical intervention is considered when conservative methods fail to provide adequate relief or when the herniated disc is causing significant neurological issues, such as weakness or numbness in the limbs. The decision for surgery is made on a case-by-case basis.
- Types of Surgical Procedures: Common surgical procedures include discectomy, laminectomy, and fusion. A discectomy involves removing the herniated portion of the disc. A laminectomy removes part of the lamina, the bony arch of the vertebra, to create more space for the spinal cord or nerve roots. Fusion involves fusing two or more vertebrae together to stabilize the spine.
Recovery Following Surgery
Post-operative recovery can vary depending on the specific procedure and individual factors. A structured rehabilitation program, including physical therapy and gradual return to activity, is essential. Patients need to follow their physician’s instructions carefully to facilitate a safe and effective recovery.
- Physical Therapy: Post-surgery, physical therapy is crucial to restore strength, mobility, and range of motion. This often involves exercises, stretches, and manual techniques tailored to the specific surgical intervention and the patient’s progress.
- Pain Management: Pain management strategies may include medication and alternative therapies like acupuncture. It is vital to discuss pain management options with a physician to develop a personalized approach.
- Gradual Return to Activity: Returning to daily activities is a gradual process. Patients need to listen to their bodies and avoid activities that cause pain or discomfort.
Conservative Treatments Summary
- Physical Therapy: Addresses specific needs to improve spinal mobility and core strength.
- Medications: Used to manage pain and inflammation, consult with a physician before use.
- Lifestyle Modifications: Healthy weight, good posture, ergonomic adjustments to reduce strain.
- Heat and Cold Therapy: Help reduce pain and inflammation.
Illustrative Case Studies
Understanding herniated disc symptoms through real-life examples can significantly improve comprehension and empathy. These hypothetical case studies highlight the diverse ways herniated discs manifest and the various treatment approaches. Each case provides a glimpse into the patient journey, from initial symptoms to long-term outcomes.
Case Study 1: The Young Athlete
This case involves a 25-year-old professional basketball player experiencing persistent lower back pain. The pain intensified after a particularly strenuous game, radiating down his left leg. He also reported numbness and tingling in his toes. Physical examination revealed limited range of motion in his lower back and muscle weakness in his left leg. Initial diagnostic tests, including an MRI, confirmed a herniated disc at L4-L5.
Conservative treatment, including physical therapy focusing on core strengthening and pain management, was initially attempted. However, the pain persisted. Subsequently, a minimally invasive surgical procedure was performed to decompress the affected nerve root. The patient showed significant improvement post-surgery and returned to competitive play within six months. His recovery demonstrated a positive correlation between surgical intervention and a rapid return to normal activity.
Case Study 2: The Middle-Aged Office Worker
A 48-year-old office worker presented with gradual onset lower back pain. The pain was described as a dull ache, worsening throughout the day and often accompanied by stiffness. The pain was not significantly aggravated by movement but did radiate into the buttocks and thighs. The patient reported no numbness or tingling. Diagnostic imaging revealed a herniated disc at L5-S1.
The patient responded well to a combination of medication, including pain relievers and anti-inflammatory drugs, and physical therapy emphasizing posture correction and stretching. Regular exercise and lifestyle modifications, such as ergonomic adjustments at work, played a crucial role in long-term pain management. The patient experienced sustained relief and a return to normal activities without requiring surgical intervention.
Case Study 3: The Elderly Gardener
A 72-year-old gardener experienced progressively worsening lower back pain, accompanied by weakness in both legs. The pain was described as sharp and shooting, exacerbated by prolonged standing or walking. The patient reported difficulty with daily activities, such as walking and gardening. Diagnostic imaging showed a herniated disc at L3-L4. Given the patient’s age and overall health, conservative treatment, including pain management, physical therapy, and lifestyle modifications, was prioritized.
The patient demonstrated a slow but steady recovery, regaining mobility and independence over several months. The patient experienced noticeable pain reduction, but complete symptom resolution was not achieved. This case underscores the importance of individualized treatment plans based on patient-specific factors.
Case Study Summary Table
| Case Study | Symptoms | Diagnosis | Treatment |
|---|---|---|---|
| Young Athlete | Lower back pain, radiating leg pain, numbness/tingling | L4-L5 herniated disc | Physical therapy, minimally invasive surgery |
| Middle-Aged Office Worker | Gradual onset lower back pain, radiating to buttocks/thighs | L5-S1 herniated disc | Medication, physical therapy, lifestyle modifications |
| Elderly Gardener | Progressive lower back pain, leg weakness, difficulty with mobility | L3-L4 herniated disc | Pain management, physical therapy, lifestyle modifications |
Final Wrap-Up

In conclusion, recognizing the symptoms of a herniated disc is essential for prompt medical attention. The variety of symptoms, from localized pain to radiating numbness and weakness, can vary significantly depending on the location and severity of the herniation. While some cases resolve with conservative treatments, others may require more intervention. This article provides a valuable overview of herniated disc symptoms, empowering readers with knowledge to better understand and manage this condition.

