Types of sleep apnea encompass a spectrum of breathing disorders that disrupt restful sleep. These conditions, ranging from the well-known obstructive sleep apnea to less common variations, can significantly impact overall health and well-being. Understanding the different types, their causes, symptoms, and treatment options is crucial for effective management and improved quality of life. This comprehensive guide will explore the various types of sleep apnea, highlighting the key differences and similarities between them.
This exploration delves into the underlying mechanisms behind each type, from the physical blockages of obstructive sleep apnea to the central nervous system irregularities in central sleep apnea. We’ll also examine the mixed form, a combination of both, and consider other less common types. A comparison table will be provided to illustrate the distinctions. This detailed look at the diverse types of sleep apnea will be beneficial for anyone seeking to understand this complex issue better.
Introduction to Sleep Apnea
Sleep apnea is a sleep disorder characterized by pauses in breathing during sleep. These pauses can last from a few seconds to minutes and occur repeatedly throughout the night. This disruption of breathing can lead to significant health consequences, affecting both physical and mental well-being. Understanding the different types of sleep apnea is crucial for effective diagnosis and treatment.Sleep apnea is a serious medical condition that impacts a person’s overall health.
The repeated interruptions of breathing during sleep deprive the body of adequate oxygen, leading to various physiological consequences. It’s important to note that recognizing the symptoms and seeking prompt medical attention are crucial for managing sleep apnea effectively.
Common Symptoms of Sleep Apnea
Recognizing the symptoms of sleep apnea is the first step towards effective management. These symptoms can vary in intensity and frequency. Common symptoms include loud snoring, gasping or choking sounds during sleep, daytime sleepiness, morning headaches, difficulty concentrating, and irritability. Individuals may also experience frequent awakenings during the night, leading to poor sleep quality. These symptoms can often be subtle, making it important to be aware of the possible signs and to consult a healthcare professional if concerned.
Physiological Mechanisms of Sleep Apnea
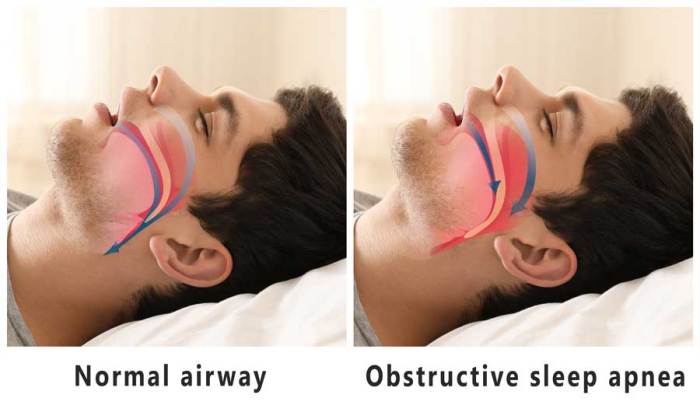
The physiological mechanisms underlying different types of sleep apnea are complex and involve interactions between various systems in the body. Obstructive sleep apnea (OSA) occurs when the airway passages narrow or collapse during sleep, preventing air from flowing into the lungs. Central sleep apnea (CSA) is characterized by the brain’s failure to send signals to the muscles that control breathing.
Mixed sleep apnea involves a combination of both obstructive and central events. The specific physiological mechanisms of each type differ, but the common outcome is the disruption of normal breathing patterns during sleep.
Types of Sleep Apnea: A Comparison
| Type | Cause | Symptoms | Impact |
|---|---|---|---|
| Obstructive Sleep Apnea (OSA) | Narrowing or collapse of the airway passages during sleep, often due to anatomical factors (e.g., enlarged tonsils, a deviated septum) or obesity. Increased throat tissue and soft palate are contributing factors. | Loud snoring, gasping or choking sounds during sleep, daytime sleepiness, morning headaches, difficulty concentrating, irritability, frequent awakenings during the night. | Increased risk of cardiovascular disease, stroke, hypertension, and type 2 diabetes. It can also contribute to cognitive impairment and mood disorders. |
| Central Sleep Apnea (CSA) | Failure of the brain to send signals to the muscles that control breathing. It can be caused by neurological conditions like stroke, certain medications, or heart failure. | Daytime sleepiness, frequent awakenings during the night, often without the presence of snoring. In some cases, gasping or choking may be observed. | Increased risk of cardiovascular complications, reduced quality of life due to poor sleep, and increased risk of accidents. |
| Mixed Sleep Apnea | Combination of obstructive and central sleep apnea events. A person might experience both airway blockage and the brain’s failure to signal breathing muscles. | A combination of symptoms from both OSA and CSA. | Potential for significant health consequences due to the cumulative impact of both obstructive and central events. |
Obstructive Sleep Apnea (OSA)
Obstructive sleep apnea (OSA) is a common sleep disorder characterized by pauses in breathing during sleep. These pauses, known as apneas, can last for several seconds or minutes and repeatedly disrupt sleep. This disruption leads to a lack of sufficient oxygen to the body, impacting various bodily functions and potentially causing significant health issues. Understanding the causes, diagnostics, risk factors, severity levels, and consequences of untreated OSA is crucial for effective management and prevention.
Causes of OSA
OSA occurs when the airway passages in the throat become blocked or narrowed during sleep. This blockage prevents sufficient airflow, leading to pauses in breathing. Several factors can contribute to this obstruction. Obesity is a significant contributor, as excess fat deposits in the throat area can narrow the airway. Anatomical factors, such as a small jaw or a large tongue, can also play a role.
Certain medical conditions, such as nasal congestion, enlarged tonsils or adenoids, and a deviated septum, can further constrict the airway. Furthermore, certain medications and some underlying medical conditions can contribute to the occurrence of OSA.
Diagnostic Criteria for OSA
Diagnosis of OSA typically involves a comprehensive evaluation of symptoms, medical history, and sleep study results. Polysomnography, or sleep studies, are used to monitor brain activity, breathing patterns, heart rate, and oxygen levels during sleep. These studies help to identify apneas and hypopneas, which are reductions in airflow. Diagnostic criteria often include an apnea-hypopnea index (AHI) value exceeding a specific threshold, typically 5 or more events per hour of sleep.
The AHI is a measure of the frequency of breathing pauses and reductions in airflow.
Risk Factors for OSA
Several factors increase the likelihood of developing OSA. Obesity is a significant risk factor, as excess weight often contributes to the narrowing of the airway. Age, particularly middle age and beyond, is associated with a higher risk. Male gender is also a recognized risk factor, though women can also be affected. Family history of OSA suggests a genetic predisposition.
Certain medical conditions, like nasal congestion or a deviated septum, can contribute to airway obstruction. Smoking and alcohol consumption can also worsen OSA symptoms.
Severity Levels of OSA, Types of sleep apnea
The severity of OSA is typically categorized based on the apnea-hypopnea index (AHI). A higher AHI indicates a more severe form of the disorder. Understanding the severity level is crucial for determining the most appropriate treatment plan.
| Severity Level | Apnea-Hypopnea Index (AHI) | Symptoms | Treatment Options |
|---|---|---|---|
| Mild | 5-15 events/hour | Snoring, occasional pauses in breathing | Lifestyle changes, CPAP therapy |
| Moderate | 15-30 events/hour | Frequent snoring, daytime sleepiness, morning headaches | CPAP therapy, lifestyle changes, oral appliances |
| Severe | >30 events/hour | Loud snoring, frequent pauses in breathing, severe daytime sleepiness, difficulty concentrating | CPAP therapy, surgery, oral appliances |
Impact of Untreated OSA on Overall Health
Untreated OSA can have significant adverse effects on overall health. It can lead to daytime sleepiness, fatigue, and difficulty concentrating. This can impact work performance, relationships, and overall quality of life. Furthermore, untreated OSA increases the risk of developing cardiovascular problems, such as high blood pressure, heart disease, and stroke. It can also contribute to type 2 diabetes and other metabolic disorders.
Understanding the different types of sleep apnea is crucial, as it can significantly impact overall health. One area of particular concern is the connection between sleep apnea and heart disease in women, a critical issue that warrants further investigation. Studies have shown a correlation between untreated sleep apnea and an increased risk of heart disease in women, highlighting the importance of early diagnosis and treatment.
Different types of sleep apnea, such as obstructive and central, require tailored approaches, and a proper understanding of these variations is vital for effective management. For more information on heart health in women, check out this resource on heart disease in women.
Additionally, untreated OSA may increase the risk of accidents due to impaired alertness. The impact of untreated OSA extends beyond the immediate symptoms, affecting various aspects of health and well-being.
Central Sleep Apnea (CSA)
Central sleep apnea (CSA) is a type of sleep apnea where the brain fails to send the proper signals to the muscles that control breathing. Unlike obstructive sleep apnea (OSA), where a physical blockage prevents airflow, CSA arises from a problem within the central nervous system. This difference in underlying mechanisms leads to distinct symptoms and treatment approaches.Central sleep apnea is characterized by pauses in breathing during sleep, resulting from a lack of signals from the brain to the respiratory muscles.
Understanding the different types of sleep apnea is crucial for effective treatment. While researching various sleep apnea forms, I stumbled upon the importance of proper post-surgery care, like learning how to take a sitz bath, how to take a sitz bath. Knowing the best techniques for a sitz bath can really help with recovery, which is a key element in managing certain sleep apnea conditions.
Different types of sleep apnea, like obstructive, central, and mixed, all have varying causes and treatments, so it’s important to consult a healthcare professional for proper diagnosis and management.
These pauses can be brief or extended, and they can occur frequently throughout the night, disrupting sleep quality and potentially impacting overall health.
Underlying Mechanisms of CSA
Central sleep apnea occurs when the brain fails to send the proper signals to the respiratory muscles. This can stem from various neurological or medical conditions that affect the brain’s control over breathing. The brain may not initiate breathing signals, or it may signal incorrectly. This can result in brief or prolonged pauses in breathing during sleep.
Medical Conditions Linked to CSA
Several medical conditions are linked to central sleep apnea. These include stroke, heart failure, and certain neurological disorders such as multiple sclerosis. Furthermore, medications such as opioids and some sedatives can also contribute to the development of CSA. These conditions can affect the brain’s ability to regulate breathing, thus increasing the risk of central sleep apnea.
Diagnostic Methods for Identifying CSA
Diagnosing central sleep apnea typically involves a comprehensive sleep study, also known as a polysomnography (PSG). This test monitors various physiological functions during sleep, including brain activity, airflow, oxygen levels, and heart rate. A PSG can accurately identify patterns of central apnea events, helping differentiate it from other sleep disorders. It also helps identify the underlying medical conditions that might be contributing to the central sleep apnea.
Differences in Symptoms Between CSA and OSA
While both CSA and OSA involve pauses in breathing during sleep, the symptoms can differ. Individuals with central sleep apnea might experience excessive daytime sleepiness, but they might not experience the loud snoring associated with OSA. The symptoms can also vary based on the underlying cause. Some people may experience a headache or other symptoms related to their underlying condition.
A sleep study can help differentiate between these two types of sleep apnea.
Ever wondered about the different types of sleep apnea? Well, it turns out there’s more to understanding your body than just your sleep patterns. Did you know that your digestive system, like your colon, plays a significant role in overall health? Learning about facts about your colon might actually shed light on some sleep-related issues.
From obstructive to central sleep apnea, understanding these different types can be crucial for diagnosis and treatment.
Long-Term Effects of Untreated CSA
Untreated central sleep apnea can have significant long-term health consequences. It can lead to an increased risk of hypertension, heart disease, and stroke. The chronic sleep deprivation can also negatively impact cognitive function, leading to reduced alertness, impaired memory, and difficulty concentrating. It’s crucial to diagnose and treat central sleep apnea to prevent these potentially serious health complications.
Effectiveness of Treatments for CSA
Treatments for central sleep apnea vary depending on the underlying cause. In cases where a specific medical condition is responsible, addressing that condition can often improve or resolve CSA. For instance, treating heart failure can alleviate central sleep apnea symptoms. CPAP therapy is often not effective for CSA, as it is primarily used to treat the physical obstruction in OSA.
Other treatments might include medications to regulate breathing or other therapies focused on improving underlying medical conditions. The effectiveness of different treatments should be evaluated individually based on the patient’s specific circumstances.
Mixed Sleep Apnea: Types Of Sleep Apnea
Mixed sleep apnea, a complex sleep disorder, represents a blend of both obstructive and central sleep apnea. Understanding its unique characteristics, causes, and treatment challenges is crucial for accurate diagnosis and effective management. This form of sleep apnea presents a diagnostic and therapeutic conundrum, often requiring a comprehensive approach.Mixed sleep apnea arises from a simultaneous occurrence of both obstructive and central apnea events during sleep.
This means that breathing pauses are caused by a combination of airway obstruction and a lack of proper signals from the brain to the respiratory muscles. This dual nature significantly impacts the severity and presentation of the disorder.
Combination of OSA and CSA
The coexistence of obstructive and central apnea events in mixed sleep apnea creates a complex interplay of physiological factors. Obstructive apnea episodes result from the physical blockage of the airway, often due to soft tissue collapse. Central apnea episodes, on the other hand, arise from the brain’s failure to properly signal the respiratory muscles to initiate breathing. This combination can fluctuate in severity and frequency throughout the night, making diagnosis and treatment challenging.
Causes of Mixed Sleep Apnea
The causes of mixed sleep apnea are often multifactorial, reflecting the convergence of obstructive and central apnea mechanisms. While the exact causes remain multifaceted, some contributing factors include:
- Underlying medical conditions:
- Heart failure can lead to fluid buildup in the body, impacting the airway and potentially causing obstructive events. Furthermore, heart failure can also affect the brain’s respiratory control centers, increasing the likelihood of central events.
- Neurological disorders, such as stroke or multiple sclerosis, can disrupt the signals between the brain and the respiratory muscles, leading to both obstructive and central events.
- Certain medications, such as opioids or sedatives, can depress respiratory function, potentially triggering both obstructive and central apneas.
- Obesity and physical factors:
- Obesity is a major risk factor for both obstructive and central sleep apnea. The extra weight and fat deposition in the neck region can narrow the airway, leading to obstructive events. Simultaneously, the altered physiology associated with obesity can impact the brain’s respiratory control, potentially resulting in central events.
- Other factors:
- Chronic lung conditions, such as asthma or chronic obstructive pulmonary disease (COPD), can contribute to a combination of obstructive and central apnea events.
Symptoms Specific to Mixed Sleep Apnea
Symptoms of mixed sleep apnea often mirror those of both obstructive and central sleep apnea. Patients may experience daytime sleepiness, fatigue, and difficulty concentrating, along with the common symptoms of snoring, gasping, and pauses in breathing during sleep. The combination of these symptoms can create a unique presentation, requiring careful evaluation by healthcare professionals.
Diagnostic Challenges of Mixed Sleep Apnea
Diagnosing mixed sleep apnea presents a challenge due to the overlapping nature of obstructive and central apnea events. Standard polysomnography (sleep study) may not always definitively identify the mixed nature of the disorder. Interpreting the results often requires careful consideration of the patterns of both obstructive and central apnea events throughout the sleep cycle. Advanced analysis and interpretation by trained sleep specialists are crucial.
Challenges in Treating Mixed Sleep Apnea
Treatment for mixed sleep apnea requires a tailored approach that addresses both the obstructive and central components. Treating only one component may not effectively resolve the overall sleep apnea problem. The presence of underlying medical conditions or the complexity of central apnea can significantly impact the effectiveness of treatment strategies. Careful assessment of the patient’s overall health and the interplay of factors contributing to mixed apnea is vital.
Potential Treatment Options for Mixed Sleep Apnea
Treating mixed sleep apnea requires a multi-faceted approach, often involving a combination of therapies. Treatment options may include:
- CPAP therapy:
- Continuous Positive Airway Pressure (CPAP) therapy, while effective for obstructive sleep apnea, may not adequately address the central apnea component in mixed sleep apnea.
- Other therapies:
- Weight management, lifestyle changes, and addressing underlying medical conditions can positively impact both obstructive and central components of mixed sleep apnea.
- Supplemental oxygen therapy may be beneficial in some cases, particularly when central apnea is a significant component.
- Positive airway pressure devices other than CPAP (e.g., BiPAP) might be considered, depending on the specific interplay of obstructive and central events.
Other Types (if applicable)
While obstructive, central, and mixed sleep apnea are the most prevalent types, several other less common forms of sleep apnea exist. These variations often present unique diagnostic and management challenges due to their distinct underlying mechanisms. Understanding these nuances is crucial for healthcare professionals to provide tailored care to patients.The diagnostic process for these less common types frequently involves specialized testing and a thorough evaluation of the patient’s medical history, symptoms, and sleep patterns.
This comprehensive approach ensures an accurate diagnosis and appropriate management plan.
Idiopathic Sleep Apnea
Idiopathic sleep apnea is a form of sleep-disordered breathing characterized by recurrent episodes of apnea (cessation of breathing) during sleep, with no identifiable cause. This distinguishes it from other types of sleep apnea, which usually have a clear underlying medical condition. The exact pathophysiology of idiopathic sleep apnea remains unclear, making its management somewhat challenging. It’s important to rule out other potential causes before reaching this diagnosis.
Research is ongoing to better understand the mechanisms involved and develop more effective treatment strategies.
Congenital Central Sleep Apnea (CCSA)
Congenital central sleep apnea (CCSA) is a rare form of central sleep apnea that presents in infancy. It is characterized by a disruption in the brain’s signals responsible for breathing during sleep. Infants with CCSA may exhibit symptoms such as rapid breathing, difficulty feeding, and decreased alertness. The exact cause of CCSA is often unknown. It’s crucial to distinguish CCSA from other causes of respiratory distress in infants, like infections or other congenital conditions.
Upper Airway Resistance Syndrome (UARS)
Upper airway resistance syndrome (UARS) is characterized by repeated episodes of significant upper airway narrowing during sleep, resulting in decreased airflow. Unlike obstructive sleep apnea, where complete cessation of breathing occurs, UARS involves a reduction in airflow. Symptoms may include snoring, daytime sleepiness, and fatigue, but often lack the severe respiratory distress seen in other types of sleep apnea.
The diagnosis often relies on polysomnography to differentiate it from other sleep disorders. Treatment approaches for UARS may focus on improving upper airway patency, such as with positional therapy or oral appliances.
Treatment Approaches Comparison
Management approaches for these less common types of sleep apnea often involve a combination of strategies, similar to those used for OSA, but with considerations for the unique underlying mechanisms. Lifestyle modifications, such as weight loss, avoiding alcohol and sedatives, and maintaining a regular sleep schedule, are commonly recommended. Positive airway pressure (PAP) therapy, particularly CPAP, is frequently employed for symptomatic relief.
However, the specific type of PAP device and pressure settings may vary based on the individual’s needs and the type of sleep apnea.
| Type of Sleep Apnea | Diagnostic Challenges | Treatment Challenges |
|---|---|---|
| Idiopathic | Identifying the root cause is challenging. | Treatment strategies may vary due to the unknown cause. |
| Congenital Central | Differentiating from other neonatal respiratory issues. | Management strategies need to be tailored for infants. |
| Upper Airway Resistance | Differentiating from other sleep disorders with similar symptoms. | Treatment response can vary based on the individual’s specific anatomy and contributing factors. |
Impact of Sleep Apnea
Sleep apnea, a condition characterized by pauses in breathing during sleep, significantly impacts various aspects of daily life. These disruptions not only affect the quality of sleep but also have cascading effects on physical and mental well-being, interpersonal relationships, and overall quality of life. Understanding the multifaceted consequences of sleep apnea is crucial for effective diagnosis, treatment, and management.
Cognitive Function
Sleep apnea directly affects cognitive function, impacting alertness, concentration, and memory. Chronic sleep deprivation caused by repeated awakenings due to breathing interruptions leads to impaired cognitive performance. Individuals with sleep apnea often experience daytime sleepiness, difficulty concentrating, and reduced alertness, which can negatively affect their ability to perform tasks at work, school, or home. This can manifest in decreased productivity, increased errors, and difficulty with complex tasks.
Studies have shown a correlation between sleep apnea and an increased risk of cognitive decline and dementia.
Cardiovascular Health
Sleep apnea is strongly linked to cardiovascular problems. The repeated drops in oxygen levels and increases in carbon dioxide during sleep apnea episodes place a strain on the cardiovascular system. This strain can lead to high blood pressure, irregular heartbeats (arrhythmias), and an increased risk of heart attack and stroke. Furthermore, the chronic inflammation associated with sleep apnea contributes to atherosclerosis, the buildup of plaque in the arteries, further increasing the risk of cardiovascular diseases.
Individuals with sleep apnea often exhibit elevated levels of inflammatory markers in their blood, a crucial indicator of cardiovascular risk.
Mental Health
The impact of sleep apnea extends to mental health, potentially contributing to mood disorders and other mental health issues. Chronic sleep deprivation, a hallmark of sleep apnea, can lead to irritability, anxiety, and depression. The constant stress on the body and brain due to repeated oxygen deprivation and sleep disruption can trigger or exacerbate mental health conditions. The vicious cycle of poor sleep and mental distress can significantly impair daily functioning and quality of life.
Studies have shown a correlation between sleep apnea and increased risk of depression and anxiety.
Interpersonal Relationships
Sleep apnea can negatively affect interpersonal relationships due to its impact on mood, behavior, and energy levels. Daytime sleepiness, irritability, and difficulty concentrating can lead to strained relationships with family members, partners, and colleagues. Individuals with sleep apnea may experience emotional outbursts, reduced patience, and difficulties in communication. This can result in conflicts and misunderstandings, impacting the quality of social interactions.
The impact on relationships can further contribute to stress and worsen the sleep apnea symptoms themselves, creating a complex feedback loop.
Diagnosis and Treatment
Understanding sleep apnea goes beyond simply recognizing its symptoms. Accurate diagnosis is crucial for tailoring effective treatment strategies. The journey to managing sleep apnea often involves a combination of medical evaluations, lifestyle adjustments, and, in some cases, therapeutic interventions. This process aims to identify the specific type of apnea and develop a personalized treatment plan.The diagnostic process for sleep apnea begins with a thorough evaluation of symptoms and medical history.
This includes a review of sleep habits, overall health conditions, and any potential risk factors. The evaluation also aims to understand the patient’s lifestyle, work patterns, and potential stressors.
Diagnostic Process
The diagnosis of sleep apnea typically involves a polysomnography (PSG) test. This overnight sleep study monitors various physiological parameters during sleep, including brain waves, heart rate, breathing patterns, and oxygen levels. The PSG provides crucial data for identifying apnea events and their characteristics, which helps distinguish between the different types of sleep apnea. Additional tests may be conducted, such as blood tests or chest X-rays, to rule out other potential underlying conditions.
This comprehensive approach ensures an accurate diagnosis and allows for a tailored treatment plan.
Treatment Options
Effective treatment for sleep apnea often involves a multi-pronged approach. This might include lifestyle modifications, medical interventions, or, in some cases, surgical procedures. The choice of treatment depends on the type and severity of sleep apnea, as well as the individual patient’s health status.
Lifestyle Modifications
Lifestyle modifications play a significant role in managing sleep apnea. These modifications can include weight loss, if applicable, as obesity is a significant risk factor for sleep apnea. Avoiding alcohol and sedatives before bedtime can also improve sleep quality. Regular exercise and a balanced diet contribute to overall health and can help mitigate some of the underlying factors associated with sleep apnea.
Consistency in these lifestyle changes is essential for long-term improvement.
CPAP Therapy
Continuous Positive Airway Pressure (CPAP) therapy is a widely used treatment for obstructive sleep apnea (OSA). A CPAP machine delivers a continuous flow of air pressure through a mask worn during sleep. This pressure helps keep the airway open, preventing the pauses in breathing that characterize OSA. CPAP therapy is often the first-line treatment for moderate to severe OSA.
Patient adherence to CPAP therapy is crucial for its effectiveness.
Surgery
In some cases, surgery may be an option for treating sleep apnea. Surgical procedures aim to address anatomical issues that contribute to airway obstruction. These procedures vary in complexity and invasiveness. For example, uvulopalatopharyngoplasty (UPPP) is a surgical procedure that reduces tissue in the back of the throat to create more space for the airway. Surgery is typically considered for patients who have not responded well to other treatments or for those with severe anatomical obstructions.
Treatment Summary
| Treatment | Mechanism | Effectiveness | Side Effects |
|---|---|---|---|
| Lifestyle Modifications | Improve overall health and reduce risk factors | Variable, depends on individual response | Minimal, if any |
| CPAP Therapy | Maintain continuous airflow through the airway | Generally effective for OSA | Mask discomfort, nasal dryness, and psychological issues in some cases |
| Surgery | Address anatomical obstructions | Effective for specific cases with anatomical issues | Potential for complications like bleeding, infection, or nerve damage |
Diagnostic and Treatment Pathway Flow Chart
[A flow chart illustrating the diagnostic and treatment pathway would be included here. This would visually depict the steps involved in diagnosing and treating sleep apnea, from initial evaluation to treatment selection. The flow chart would show the options at each step, such as further testing, lifestyle modifications, CPAP, and surgery. The flow chart would be visually clear and informative.]
Ending Remarks
In conclusion, the variety of sleep apnea types underscores the complexity of this sleep disorder. From obstructive sleep apnea, the most prevalent form, to central sleep apnea and mixed sleep apnea, each type presents unique challenges in diagnosis and treatment. Understanding the distinctions between these types is essential for proper diagnosis and effective management. The impact on daily life, cognitive function, cardiovascular health, and mental well-being is significant.
Effective treatment options, including lifestyle modifications, CPAP therapy, and surgical interventions, are available for each type. The journey to better sleep begins with understanding the nuances of sleep apnea.