Things to know about your ovaries and ovulation: Dive deep into the fascinating world of female reproductive health. This comprehensive guide explores the intricate workings of your ovaries, the crucial ovulation process, and the overall menstrual cycle. From understanding ovarian anatomy to recognizing potential health concerns and fertility, you’ll gain valuable insights into your body’s amazing capabilities.
We’ll cover the structure and function of your ovaries, the steps involved in ovulation, and the hormonal interplay that governs the menstrual cycle. You’ll learn about common ovarian conditions, the impact of lifestyle choices, and the importance of early detection when it comes to ovarian health. We’ll also discuss fertility and how ovarian function plays a role in conception.
Ovarian Anatomy and Function
The ovaries, small almond-shaped organs nestled within the female pelvis, are crucial for reproductive health. They play a multifaceted role, producing eggs (ova) and the hormones that regulate the menstrual cycle and support pregnancy. Understanding ovarian anatomy and function is vital for comprehending the intricacies of female reproductive biology.
Ovarian Structure
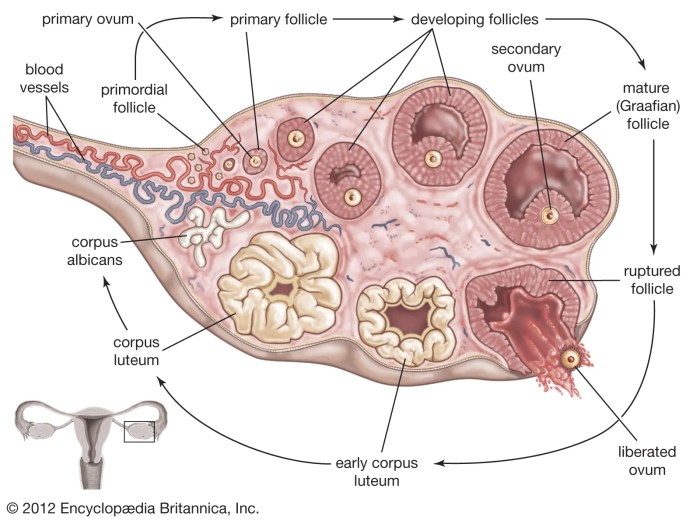
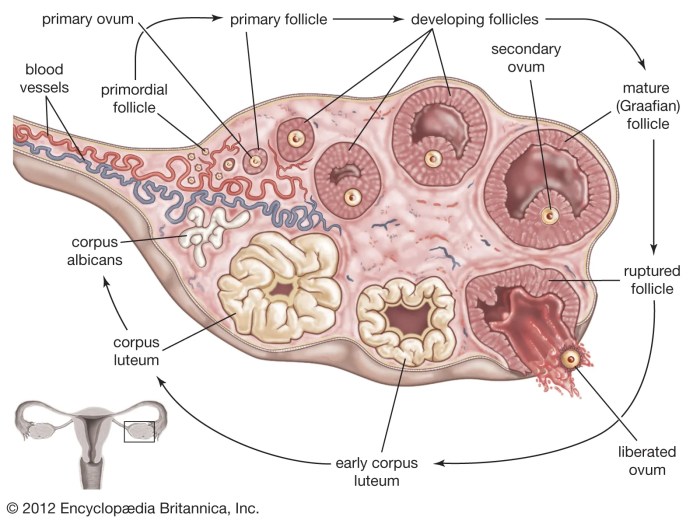
The ovary is composed of a cortex and a medulla. The cortex, the outer layer, houses the developing follicles containing the eggs. The medulla, the inner region, contains blood vessels, nerves, and connective tissue. These structures support the function of the follicles and the entire ovary.
Understanding your ovaries and ovulation cycle is key to overall health. Did you know that certain skin changes can sometimes be related to hormonal fluctuations? For instance, some women experience skin rashes or unusual blemishes during their cycle. If you’re concerned about skin changes, it’s essential to consult a doctor, especially if the changes are persistent or accompanied by other symptoms.
Checking out resources on skin cancer and rash, like this one skin cancer and rash , can help you understand potential connections and know when to seek professional medical advice. Ultimately, learning about your body and its signals is a crucial step in maintaining your well-being, and that includes understanding your ovaries and ovulation.
Oogenesis
Oogenesis is the process of egg development within the ovaries. It begins prenatally and continues throughout a woman’s reproductive years. Primordial follicles, containing immature oocytes, are present at birth. As a girl matures, these follicles undergo further development, eventually leading to ovulation. This process is tightly regulated by hormonal signals.
Follicle Development
Follicles are fluid-filled structures that nurture and protect the developing egg. Primordial follicles progress through various stages of growth, transforming into primary, secondary, and finally, Graafian follicles. This development is crucial for the maturation of the oocyte and its preparation for ovulation. Hormonal signals play a key role in determining which follicles progress to the next stage.
Hormonal Regulation
The hypothalamus, pituitary gland, and ovaries interact in a complex feedback loop to regulate ovarian function. The hypothalamus releases gonadotropin-releasing hormone (GnRH), which stimulates the pituitary gland to produce follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These hormones, in turn, influence follicle development and ovulation. Estrogen and progesterone are crucial ovarian hormones that influence the uterine lining and the entire menstrual cycle.
Role in the Menstrual Cycle
The ovaries are central to the menstrual cycle. During the follicular phase, FSH stimulates follicle growth and estrogen production. As the follicle matures, estrogen levels rise, triggering the thickening of the uterine lining. LH surge triggers ovulation, releasing the mature egg. After ovulation, the remaining follicle transforms into the corpus luteum, producing progesterone, which prepares the uterus for potential pregnancy.
If pregnancy does not occur, the corpus luteum degenerates, leading to menstruation.
| Structure | Function | Key Hormones |
|---|---|---|
| Cortex | Houses developing follicles | FSH, LH, Estrogen, Progesterone |
| Medulla | Contains blood vessels, nerves, and connective tissue | FSH, LH, Estrogen, Progesterone |
| Primordial follicle | Contains immature oocyte | FSH, LH, Estrogen, Progesterone |
| Primary follicle | Early stage of follicle development | FSH, LH, Estrogen, Progesterone |
| Secondary follicle | Further development of follicle | FSH, LH, Estrogen, Progesterone |
| Graafian follicle | Mature follicle, ready for ovulation | FSH, LH, Estrogen, Progesterone |
| Corpus luteum | Produces progesterone after ovulation | Progesterone |
Ovulation
Ovulation is the crucial phase in a woman’s reproductive cycle where a mature egg is released from the ovary. This event marks the potential for fertilization, leading to pregnancy if the egg is successfully met with sperm. Understanding the process and timing of ovulation is essential for fertility awareness, family planning, and diagnosing potential reproductive issues.
The Ovulation Process
Ovulation is a complex series of events orchestrated by the interplay of hormones. The process involves the follicle containing the egg maturing and rupturing, releasing the egg into the fallopian tube. This process is typically cyclical, occurring roughly every 28 days, though individual cycles can vary significantly. The precise timing of ovulation can influence the success of conception.
Factors Influencing Ovulation Timing
Several factors can impact the precise timing of ovulation. These include stress levels, changes in lifestyle, nutritional intake, and underlying health conditions. For example, significant stress can disrupt the hormonal balance, potentially affecting the regularity and timing of ovulation. Similarly, drastic changes in diet or intense physical activity can interfere with the normal hormonal signals. Moreover, certain medical conditions may cause irregular or absent ovulation.
Hormonal Changes Leading to Ovulation
The release of the egg is triggered by a surge in luteinizing hormone (LH). This surge, which occurs roughly 24-36 hours before ovulation, stimulates the follicle to release the mature egg. This is closely followed by a decrease in follicle-stimulating hormone (FSH), which helps regulate the development of the follicle. The interplay of these hormones ensures the precise timing and successful release of the egg.
Ovulation Prediction Methods
Various methods exist for predicting ovulation, each with its strengths and limitations. Accurate prediction is crucial for maximizing the chances of conception. One method involves tracking basal body temperature (BBT). Women record their body temperature each morning before any activity. A slight rise in temperature typically indicates ovulation.
Another method involves using ovulation prediction kits (OPKs). These kits detect the surge in LH in the urine, signaling the impending release of the egg. Both methods offer a degree of accuracy, but factors like individual variations in cycles can influence the reliability of these methods.
Comparison of Ovulation Prediction Methods
| Method | Mechanism | Accuracy | Advantages | Disadvantages |
|---|---|---|---|---|
| Basal Body Temperature Tracking | Monitoring body temperature changes | Moderate | Relatively inexpensive, provides insights into overall cycle health | Requires meticulous daily recording, less immediate prediction |
| Ovulation Prediction Kits | Detecting LH surge in urine | High | Provides a clear signal of impending ovulation | Can be expensive, may not always detect the surge accurately |
Ovulation Process Flowchart
The following flowchart Artikels the key steps in the ovulation process.
<svg width="400" height="200"> <rect x="50" y="50" width="100" height="30" style="fill:lightgray;" /> <text x="75" y="75" font-size="12">Follicle Maturation</text> <line x1="150" y1="80" x2="250" y2="80" style="stroke:black;stroke-width:2" /> <rect x="250" y="50" width="100" height="30" style="fill:lightgray;" /> <text x="275" y="75" font-size="12">LH Surge</text> <line x1="350" y1="80" x2="350" y2="150" style="stroke:black;stroke-width:2" /> <rect x="350" y="150" width="100" height="30" style="fill:lightgray;" /> <text x="375" y="175" font-size="12">Egg Release</text> </svg>
Understanding the Menstrual Cycle
The menstrual cycle is a complex series of hormonal and physiological changes that occur in a woman’s body each month, preparing it for potential pregnancy.
Understanding this cycle is crucial for comprehending women’s health and reproductive function. It involves a delicate interplay between the brain, ovaries, and uterus, all working together to orchestrate the monthly cycle.
The menstrual cycle isn’t just about getting your period; it’s a dynamic process with different phases, each playing a crucial role in the potential for conception. Hormonal shifts drive these phases, influencing the uterine lining and the ovarian follicles, ultimately determining whether or not fertilization occurs.
Phases of the Menstrual Cycle
The menstrual cycle is typically divided into four phases: menstruation, the follicular phase, ovulation, and the luteal phase. Each phase is characterized by specific hormonal changes and corresponding physiological events within the reproductive system.
- Menstruation: This is the shedding of the uterine lining, which occurs when a mature egg isn’t fertilized. The uterine lining, enriched with blood vessels and nutrients, is prepared for potential implantation. If no fertilization happens, the lining breaks down and is shed, leading to menstruation. This bleeding, usually lasting 3-7 days, is a natural part of the cycle.
- The Follicular Phase: This phase begins on the first day of menstruation and extends until ovulation. The pituitary gland releases follicle-stimulating hormone (FSH), stimulating the growth of several ovarian follicles, each containing an immature egg. As the follicles grow, they produce estrogen, which thickens the uterine lining, preparing it for potential implantation. This phase typically lasts 10-16 days.
- Ovulation: Ovulation is the release of a mature egg from the ovary. The surge in luteinizing hormone (LH) triggers the release of the egg into the fallopian tube, where it awaits fertilization. This process typically occurs around day 14 of a 28-day cycle.
- The Luteal Phase: Following ovulation, the ruptured follicle transforms into the corpus luteum, which produces progesterone. Progesterone further prepares the uterine lining for a potential pregnancy. If fertilization doesn’t occur, the corpus luteum eventually degenerates, causing a decrease in progesterone levels, triggering menstruation, and marking the beginning of a new cycle. This phase typically lasts 14 days.
Hormonal Regulation of the Menstrual Cycle
Hormones play a pivotal role in regulating the menstrual cycle. The interplay of follicle-stimulating hormone (FSH), luteinizing hormone (LH), estrogen, and progesterone is critical.
- Follicle-stimulating hormone (FSH): Stimulates the growth of ovarian follicles, promoting the development of immature eggs.
- Luteinizing hormone (LH): Triggers ovulation, the release of the mature egg from the ovary. A surge in LH is a key marker of ovulation.
- Estrogen: Plays a vital role in thickening the uterine lining, preparing it for potential implantation. It also regulates other bodily functions, influencing mood, energy levels, and bone health.
- Progesterone: Further prepares the uterine lining for pregnancy. It maintains the lining during the luteal phase. If pregnancy doesn’t occur, progesterone levels decline, leading to menstruation.
Typical Menstrual Cycle Length and Duration
A typical menstrual cycle lasts approximately 28 days, though this can vary considerably. The length of the menstrual cycle is measured from the first day of one period to the first day of the next. The duration of menstruation itself, typically lasting 3-7 days, is a separate consideration.
Understanding your ovaries and ovulation cycle is key to overall health. Sometimes, though, skin issues like an allergic reaction on your face allergic reaction on face can be confusing. But remember, knowing your body’s signals, including those from your reproductive system, is crucial for identifying potential problems and getting the right care. Keeping track of your menstrual cycle and any related symptoms is a good first step to better understanding your overall health.
Variations in Menstrual Cycles and Irregularities, Things to know about your ovaries and ovulation
Menstrual cycles can vary significantly in length and regularity, even within a single individual. Many factors can contribute to irregularities, including stress, changes in lifestyle, hormonal imbalances, underlying health conditions, and even certain medications.
| Phase | Hormonal Fluctuations |
|---|---|
| Menstruation | Estrogen and progesterone levels are low. |
| Follicular Phase | FSH stimulates follicle growth; estrogen levels rise. |
| Ovulation | LH surge triggers ovulation; estrogen levels peak. |
| Luteal Phase | Corpus luteum produces progesterone; estrogen levels fall if no fertilization occurs. |
Ovarian Health and Conditions
Understanding the intricacies of ovarian health is crucial for overall well-being. While ovulation and the menstrual cycle are vital functions, various conditions can impact the ovaries, sometimes requiring medical intervention. This section delves into common ovarian conditions, their symptoms, causes, diagnosis, and treatment options.
Polycystic Ovary Syndrome (PCOS)
PCOS is a hormonal disorder that affects women of reproductive age. It’s characterized by an imbalance in reproductive hormones, leading to a range of symptoms. Symptoms often manifest during puberty or after significant weight changes.
- Symptoms: Common symptoms include irregular periods, excess hair growth (hirsutism), acne, weight gain, and difficulty conceiving. Some women may experience symptoms like skin darkening in certain areas, or thinning hair.
- Causes: The exact cause of PCOS is unknown, but genetic predisposition, insulin resistance, and elevated androgen levels are believed to play a role.
- Diagnosis: Diagnosing PCOS involves a combination of physical examination, medical history review, and hormonal blood tests to assess hormone levels, including follicle-stimulating hormone (FSH), luteinizing hormone (LH), and testosterone. Ultrasound imaging can also help evaluate ovarian morphology.
- Treatment: Treatment options for PCOS focus on managing symptoms and improving overall health. Lifestyle modifications, such as weight loss and regular exercise, can be highly effective. Medications, including birth control pills, metformin, and other hormonal therapies, may also be prescribed.
Ovarian Cysts
Ovarian cysts are fluid-filled sacs that develop on or within the ovaries. They can vary in size and often resolve on their own without intervention.
- Symptoms: Symptoms of ovarian cysts can range from mild discomfort to severe pain, especially during menstruation or ovulation. Some cysts may cause no symptoms at all. Abdominal bloating and pelvic pain are also possible symptoms.
- Causes: Ovarian cysts can arise from various factors, including hormonal imbalances, ovulation irregularities, and certain medical procedures. In some cases, the exact cause is unknown.
- Diagnosis: Diagnosis typically involves a pelvic examination, ultrasound imaging to visualize the ovaries and identify any cysts, and possibly blood tests to evaluate hormone levels.
- Treatment: Treatment for ovarian cysts depends on their size, symptoms, and the underlying cause. Small, asymptomatic cysts may not require treatment and often resolve spontaneously. In cases of persistent pain or complications, surgical intervention may be necessary.
Endometriosis
Endometriosis is a condition in which tissue similar to the lining of the uterus (the endometrium) grows outside the uterus. This misplaced tissue can affect various pelvic organs, causing chronic pain and other complications.
- Symptoms: Common symptoms include pelvic pain, particularly during menstruation, painful intercourse, heavy bleeding, and infertility. Pain can vary in intensity and location, and some women may not experience any noticeable symptoms.
- Causes: The exact cause of endometriosis is not fully understood, but theories include retrograde menstruation, genetic factors, and immune system dysfunction.
- Diagnosis: Diagnosis often involves a combination of medical history, physical examination, ultrasound, and laparoscopy (a surgical procedure to visually inspect the pelvic organs).
- Treatment: Treatment options for endometriosis range from pain management strategies, hormonal therapies, and surgical procedures, such as laparoscopic surgery to remove the affected tissue.
Summary Table
| Condition | Symptoms | Causes | Treatment Options |
|---|---|---|---|
| PCOS | Irregular periods, hirsutism, acne, weight gain, difficulty conceiving | Hormonal imbalance, insulin resistance, genetics | Lifestyle modifications, medications (birth control, metformin) |
| Ovarian Cysts | Mild to severe pelvic pain, bloating, possible asymptomatic | Hormonal imbalances, ovulation irregularities, medical procedures | Observation, medication, surgery (if necessary) |
| Endometriosis | Pelvic pain (especially during menstruation), painful intercourse, heavy bleeding, infertility | Retrograde menstruation, genetic factors, immune system dysfunction | Pain management, hormonal therapies, surgical intervention |
Factors Affecting Ovarian Health
Your ovaries, those vital organs responsible for producing eggs and hormones, are susceptible to a multitude of influences. Understanding these factors is crucial for maintaining optimal ovarian health and recognizing potential risks. This section delves into the impact of lifestyle choices, environmental toxins, genetic predispositions, and potential risk factors for ovarian conditions.
Lifestyle factors play a significant role in ovarian health. A balanced approach to diet, exercise, stress management, and sleep can significantly impact the health and function of your ovaries. Conversely, neglecting these areas can increase the risk of developing ovarian problems. Environmental factors, too, can affect ovarian function, and recognizing potential risks is crucial for preventative measures.
Understanding the intricate interplay between these factors is essential for proactive health management.
Lifestyle Factors and Ovarian Health
Various lifestyle choices exert considerable influence on ovarian function. A balanced diet rich in fruits, vegetables, and whole grains, along with adequate protein intake, supports overall health and potentially promotes healthy ovarian function. Regular exercise not only benefits overall health but also helps regulate hormones, which are crucial for ovulation and menstrual cycles. Effective stress management techniques can minimize the impact of stress on hormonal balance and ovarian health.
Prioritizing sufficient sleep is essential for optimal hormone production and overall well-being.
- Diet: A nutritious diet rich in fruits, vegetables, and whole grains, along with adequate protein intake, supports overall health, potentially contributing to healthy ovarian function.
- Exercise: Regular physical activity benefits overall health and can help regulate hormones, impacting ovulation and menstrual cycles.
- Stress: Chronic stress can disrupt hormonal balance, potentially impacting ovarian function. Effective stress management techniques are important for mitigating this effect.
- Sleep: Sufficient sleep is crucial for optimal hormone production and overall well-being. Adequate sleep promotes healthy ovarian function.
Environmental Toxins and Ovarian Health
Environmental toxins, such as certain chemicals and pollutants, can potentially disrupt ovarian function. Exposure to these toxins may lead to hormonal imbalances and affect the production of eggs. Research into the specific effects of environmental toxins on ovarian health is ongoing, but understanding the potential risks is vital.
Potential Risk Factors for Ovarian Conditions
Several factors can increase the risk of developing ovarian conditions. Age, family history of ovarian cancer, and certain medical conditions, such as polycystic ovary syndrome (PCOS), are potential risk factors. Early detection and appropriate management of these conditions can significantly improve outcomes.
Understanding your ovaries and ovulation is key to overall health. Knowing the typical age range for these processes is important, but it’s also crucial to consider how factors like age of onset for certain conditions, like ALS, might influence these processes. Research into the potential links between conditions like ALS age of onset and reproductive health is ongoing.
Ultimately, a deeper understanding of your body’s processes, including those related to your ovaries and ovulation, is vital for making informed decisions about your health.
Genetics and Ovarian Health
Genetic factors play a role in ovarian health and the risk of developing certain conditions. A family history of ovarian cancer or other reproductive disorders can increase an individual’s susceptibility. Understanding genetic predispositions can help individuals make informed decisions about their health and seek appropriate screening and preventative measures.
Ovarian Cancer Awareness
Knowing your body is crucial for overall well-being, and that includes understanding potential health concerns like ovarian cancer. While it’s a relatively rare cancer, early detection significantly improves outcomes. This section will explore the signs, symptoms, risk factors, and resources available for those affected.
Signs and Symptoms of Ovarian Cancer
Ovarian cancer often presents with subtle symptoms that can be easily mistaken for other conditions. Recognizing these signs is key to seeking timely medical attention. These symptoms can vary significantly, and some people may not experience any noticeable changes.
- Abdominal bloating or swelling:
- Pelvic or abdominal pain:
- Changes in bowel or bladder habits:
- Fatigue:
- Unexplained weight loss:
This persistent bloating can often be a symptom of ovarian cancer, particularly as it progresses.
Pain in the lower abdomen or pelvis can be a symptom of ovarian cancer, often accompanied by bloating or fullness.
Unexplained changes in bowel or bladder function, like increased frequency, urgency, or difficulty emptying, could be indicative of ovarian cancer.
Persistent tiredness or fatigue that doesn’t improve with rest could be a sign of an underlying health condition, including ovarian cancer.
An unexpected loss of weight, particularly if accompanied by other symptoms, may warrant a visit to a healthcare provider for evaluation.
Risk Factors for Ovarian Cancer
Several factors can increase a person’s risk of developing ovarian cancer. Understanding these factors can help individuals make informed decisions about their health and potential preventative measures.
- Age:
- Family history:
- Inherited genetic mutations:
- Previous history of certain cancers:
- Infertility treatments:
- Obesity:
The risk of ovarian cancer increases with age, particularly after menopause. For example, the average age of diagnosis is around 63 years old.
A strong family history of ovarian or breast cancer significantly increases a person’s risk. If close relatives have had these cancers, it’s important to discuss this with a healthcare professional.
Mutations in certain genes, like BRCA1 and BRCA2, significantly increase the risk of ovarian and other cancers. Genetic testing can help identify individuals at high risk.
A history of breast or colon cancer can increase the risk of ovarian cancer.
Some fertility treatments may increase the risk of ovarian cancer.
Obesity is a significant risk factor for several cancers, including ovarian cancer. Maintaining a healthy weight is essential for overall health and cancer prevention.
Importance of Early Detection and Screening
Early detection is crucial for improving the chances of successful treatment and recovery from ovarian cancer. Regular check-ups and awareness of potential symptoms can help identify the disease in its early stages.
- Regular check-ups:
- Screening tests:
- Self-awareness:
Routine check-ups with a healthcare provider are essential for monitoring overall health and detecting potential problems early.
While no definitive screening tests exist for ovarian cancer, discussions with a doctor about potential risks and symptoms are crucial.
Understanding the signs and symptoms of ovarian cancer can empower individuals to recognize potential issues and seek prompt medical attention.
Support Resources for Individuals Affected by Ovarian Cancer
Facing a diagnosis of ovarian cancer can be challenging, but support resources can provide valuable assistance and guidance. Many organizations offer information, emotional support, and practical help for individuals and their families.
- Support groups:
- Online communities:
- Cancer organizations:
- Healthcare professionals:
Support groups provide a safe space for individuals affected by ovarian cancer to share experiences, offer encouragement, and learn from others.
Online forums and communities provide virtual support and connect individuals with others facing similar challenges.
Numerous cancer organizations offer resources, information, and support services for individuals affected by ovarian cancer.
Healthcare professionals, such as oncologists and nurses, can provide medical guidance and emotional support during treatment and recovery.
Ovarian cancer risk factors include age, family history, inherited genetic mutations, previous cancers, infertility treatments, and obesity. Common symptoms include abdominal bloating, pelvic pain, changes in bowel or bladder habits, fatigue, and unexplained weight loss.
Fertility and Ovarian Function
Understanding the intricate dance of ovarian function is key to comprehending fertility. Ovarian health directly impacts a woman’s ability to conceive, and this connection is deeply influenced by various factors, including age, ovulation patterns, and overall well-being. This section delves into the vital role the ovaries play in the journey to parenthood.
Ovarian function is intricately linked to fertility. The ovaries are responsible for producing eggs (ova) and the hormones that regulate the menstrual cycle. A healthy ovarian reserve, which refers to the number of eggs remaining in the ovaries, is essential for successful ovulation and subsequent conception. Factors like age, lifestyle, and underlying health conditions can significantly affect this reserve.
The Impact of Age on Ovarian Reserve and Fertility
Age is a crucial factor in ovarian reserve and, consequently, fertility. Ovarian reserve naturally declines with age. As women age, the number of eggs available for ovulation diminishes, and the quality of those eggs can also change. This decline in ovarian reserve leads to a reduced likelihood of successful conception. For instance, a woman in her late 30s or early 40s may experience a decreased frequency of ovulation or have eggs that are less likely to fertilize.
This explains why fertility treatments are often more complex and less successful in older women. A woman’s individual experience will vary depending on several factors.
The Role of Ovulation in Conception
Ovulation is the process of releasing a mature egg from the ovary. This egg then travels through the fallopian tube, where it awaits fertilization by a sperm. For conception to occur, ovulation must take place, and the egg must be viable for fertilization. If ovulation does not happen regularly or if the egg is not released, conception is impossible.
Understanding the timing of ovulation is critical for couples trying to conceive.
Different Fertility Treatments Involving Ovarian Stimulation
Several fertility treatments involve ovarian stimulation to enhance egg production. These treatments use medications to encourage the ovaries to develop and release multiple eggs, increasing the chances of fertilization. Common methods include controlled ovarian hyperstimulation (COH). This process carefully monitors the ovarian response to medication to ensure that the stimulation is appropriate and avoids potential complications. Different types of fertility drugs have varying degrees of efficacy, and the optimal approach is determined by factors such as age, ovarian reserve, and individual response.
Tracking Ovulation to Improve Conception Chances
Tracking ovulation can significantly improve the chances of conception. Methods like basal body temperature monitoring, ovulation predictor kits, and tracking cervical mucus can help identify the fertile window. This awareness allows couples to time intercourse strategically to coincide with ovulation, maximizing the chances of fertilization. By understanding the signs and symptoms of ovulation, couples can make informed decisions about when to engage in sexual activity, thereby increasing their chances of conception.
Outcome Summary: Things To Know About Your Ovaries And Ovulation
In conclusion, understanding your ovaries and ovulation is key to comprehending your overall well-being. This exploration has highlighted the complex interplay of hormones, structures, and processes that shape your reproductive health. By gaining knowledge about your body, you can make informed decisions about your health and well-being. Remember, knowledge is power, and empowering yourself with information is the first step toward a healthier future.