Type 2 diabetes in black and brown people is a critical health issue demanding attention. This exploration delves into the significant prevalence rates and the unique risk factors impacting these communities. We’ll examine the challenges in diagnosis, the need for culturally appropriate management strategies, and the role of social determinants of health in shaping these…
Tag: Type 2 Diabetes
Diabetes Nutrition and Weight Loss Your Guide
Diabetes nutrition and weight loss is a crucial aspect of managing this condition effectively. Understanding the connection between food choices, portion sizes, and activity levels is key to achieving and maintaining a healthy weight while controlling blood sugar. This guide delves into balanced nutrition plans, effective weight loss strategies, and considerations for diverse populations, all…
Anthony Wilsons Type 2 Diabetes Journey
Anthony wilson my journey with type 2 diabetes – Anthony Wilson’s journey with type 2 diabetes sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality. He chronicles his experience from initial diagnosis to lifestyle adjustments, medical treatments, and the emotional and…
Hyvelle Fergusons Type 2 Diabetes Journey
Hyvelle ferguson my journey with type 2 diabetes – Hyvelle Ferguson’s journey with type 2 diabetes offers a compelling personal account of navigating a chronic condition. This in-depth exploration dives into the challenges and triumphs of managing type 2 diabetes, sharing insights into her experiences and strategies. From understanding the fundamental mechanisms of type 2…
Christina Herreras Diabetes Journey
Christina herrera my journey with type 2 diabetes – Christina Herrera’s journey with type 2 diabetes sets the stage for this enthralling narrative, offering readers a glimpse into a story rich in personal detail and insightful reflections. She shares her experiences, challenges, and triumphs in managing this condition, providing valuable insights and inspiration for others…
Zepbound Tirzepatide Diabetes Risk A Deep Dive
Zepbound tirzepatide diabetes risk is a critical area of concern for those managing diabetes. This in-depth look examines the potential risks associated with tirzepatide, a medication increasingly used to control blood sugar. We’ll explore its mechanism of action, potential side effects, risk factors, and the latest research. Understanding these risks is crucial for informed decision-making…
Type 2 Diabetes Nutrition and Weight Loss Your Guide
Type 2 diabetes nutrition and weight loss is a crucial aspect of managing this condition effectively. This comprehensive guide explores various dietary approaches, from the Mediterranean diet to low-carb strategies, to help you understand how nutrition plays a vital role in achieving and maintaining a healthy weight. We’ll delve into portion control, caloric intake, and…
Type 2 Diabetes Diet Your Guide to Healthy Eating
Type 2 diabetes diet is crucial for managing this condition effectively. This guide provides a comprehensive overview of the dietary principles and strategies necessary for a healthy lifestyle. It explores the fundamental aspects of a balanced diet, emphasizing portion control and the importance of specific food choices. We’ll delve into macronutrient balance, food recommendations, practical…
Type 2 Diabetes Meal Planning Your Guide
Type 2 diabetes meal planning is crucial for managing blood sugar levels and overall health. This comprehensive guide delves into the essential principles, practical strategies, and resources to create a personalized meal plan that fits your needs and lifestyle. We’ll explore everything from macronutrient distribution to carbohydrate counting, healthy food choices, and even meal planning…
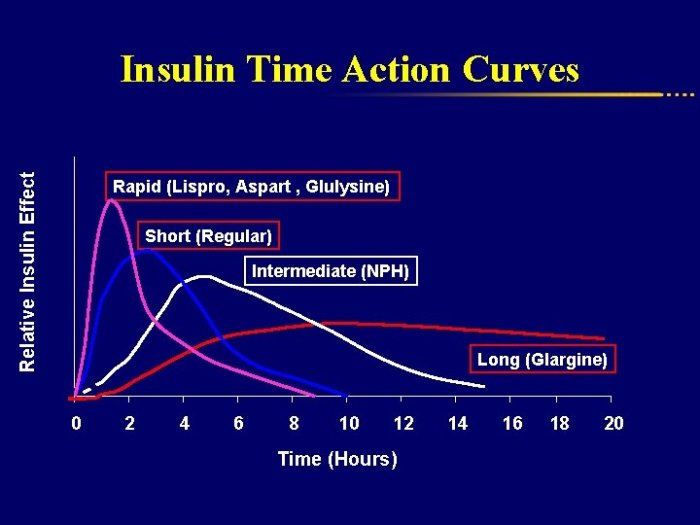
Metformin Not Working? Signs and Solutions
Signs metformin not working can be subtle, but they can significantly impact your health. This in-depth exploration dives into the potential reasons why metformin isn’t effectively managing your blood sugar. We’ll uncover possible medical issues, lifestyle factors, and medication interactions that could be hindering its effectiveness. Prepare to learn practical strategies for monitoring your progress,…