Solu Medrol for MS provides a potent anti-inflammatory approach to managing multiple sclerosis (MS). This guide delves into the intricacies of its use, from acute exacerbations to long-term management. Understanding the mechanisms of action, potential side effects, and patient considerations is crucial for effective treatment strategies. The article explores the role of inflammation in MS…
Tag: treatment
Fatigue Symptoms Causes, Diagnosis, and Treatment
Fatigue symptoms causes diagnosis and treatment is a complex issue affecting many people. This in-depth exploration dives into the various facets of fatigue, from its different forms and potential causes to effective diagnostic methods and treatment strategies. Understanding the nuances of fatigue, including its physiological and psychological roots, is crucial. This article will explore the…
Sotatercept Pulmonary Arterial Hypertension A Deep Dive
Sotatercept pulmonary arterial hypertension is a significant advancement in the fight against this often-deadly disease. This exploration delves into the specifics of this treatment, examining its mechanism of action, clinical trial data, and the impact it has on patient outcomes. We’ll also look at potential side effects and the exciting future of PAH treatment. Understanding…
CLL When to Treat A Comprehensive Guide
CLL when to treat is a crucial question for patients and healthcare providers alike. This in-depth exploration delves into the complexities of chronic lymphocytic leukemia (CLL), examining the factors that influence treatment decisions, from patient characteristics to genetic mutations. We’ll explore the various treatment options available, their effectiveness, and potential side effects, ultimately providing a…
Nicotine Patches Long COVID Treatment A Deep Dive
Nicotine patches long COVID treatment is a burgeoning area of research, exploring a potential link between nicotine and alleviating the symptoms of Long COVID. This complex topic delves into the mechanisms of nicotine’s effects on the body, compares them to the symptoms of Long COVID, and examines the potential benefits, risks, and existing research. The…
The Effects of Drug Addiction A Deep Dive
The effects of drug addiction are far-reaching and devastating, impacting individuals, families, and communities. This exploration delves into the complex web of consequences, from the initial biological triggers to the long-term societal implications. We’ll examine the immediate physiological and behavioral changes, the lasting damage to physical and mental health, and the profound social and economic…
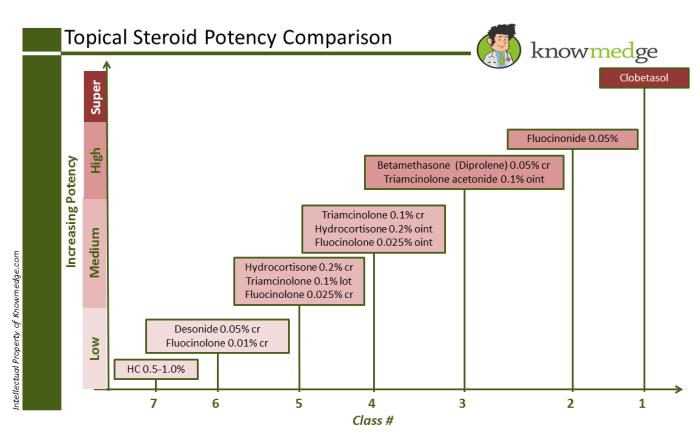
Steroids Topical Steroid Strengths A Deep Dive
Steroids topical steroid strengths are crucial for treating various skin conditions. This guide delves into the different potencies, their applications, and potential side effects. Understanding the strengths and appropriate usage is vital for effective treatment and minimizing adverse reactions. We’ll explore the diverse range of skin conditions treatable with topical steroids, examining the factors determining…
RSV and Rash Symptoms Link and Treatment
RSV and rash symptoms link and treatment is a crucial topic for parents and caregivers. Understanding the connection between Respiratory Syncytial Virus (RSV) and skin rashes can help in early diagnosis and appropriate management. This comprehensive guide explores the various types of rashes associated with RSV, their symptoms, potential causes, diagnostic methods, treatment strategies, and…
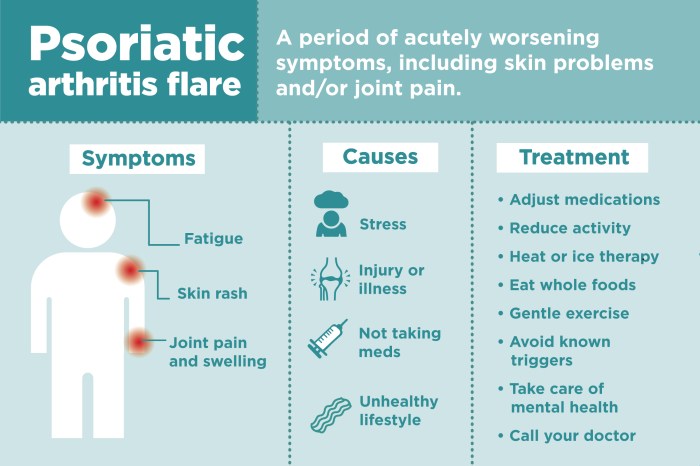
What Medications Treat Psoriatic Arthritis? A Comprehensive Guide
What medications treat psoriatic arthritis? This comprehensive guide delves into the various treatments available for this complex condition. Psoriatic arthritis, a chronic inflammatory disease, affects not only the joints but also the skin, causing pain, stiffness, and inflammation. Understanding the different medication options and their mechanisms of action is crucial for effective management. We’ll explore…
Hand and Wrist Lumps and Bumps A Comprehensive Guide
Hand and wrist lumps and bumps can be a source of worry, but understanding the various causes, symptoms, and treatment options can ease anxieties. This comprehensive guide explores the diverse possibilities, from benign conditions to more serious concerns, equipping you with knowledge to navigate this potentially perplexing health issue. We’ll delve into the different types…