What happens if you stop breathing in your sleep? This is a crucial question for understanding sleep apnea, a common yet often overlooked sleep disorder. It’s a condition where breathing repeatedly stops and starts during sleep, affecting everything from your physical health to your daily life. This exploration will delve into the physiological processes behind…
Tag: sleep disorders
How Does Sleep Inertia Make It Hard to Wake Up?
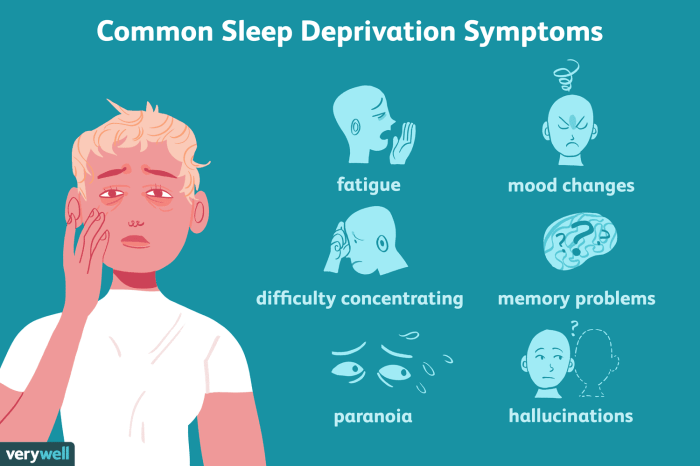
How does sleep inertia make it hard to wake up? This deep dive explores the physiological processes behind that sluggish feeling after waking. We’ll uncover the stages of sleep, neurochemical shifts, and how sleep deprivation amplifies this inertia. The result? A frustrating struggle to get going in the morning, impacting everything from concentration to mood….
Why We Drool in Our Sleep A Deep Dive
Why we drool in our sleep sets the stage for this enthralling narrative, offering readers a glimpse into the fascinating world of nocturnal physiology. This exploration delves into the intricate mechanisms behind this seemingly mundane phenomenon, examining everything from the activity of our salivary glands to the potential correlation between sleep stages and drooling episodes….
Why Does Coffee Make Me Sleepy? The Truth Unveiled
Why does coffee make me sleepy? This seemingly paradoxical question plagues many coffee lovers. It’s a common experience, and the answer isn’t always straightforward. This blog post dives deep into the complex relationship between coffee and sleep, exploring individual differences, consumption habits, underlying health conditions, and alternative options to help you understand why your morning…