Types of sleep apnea encompass a spectrum of breathing disorders that disrupt restful sleep. These conditions, ranging from the well-known obstructive sleep apnea to less common variations, can significantly impact overall health and well-being. Understanding the different types, their causes, symptoms, and treatment options is crucial for effective management and improved quality of life. This…
Tag: sleep disorders
Night Leg Cramps Understanding and Relief
Leg cramps at night can be incredibly disruptive, jolting you awake with sudden, sharp pain. This post dives deep into understanding these nocturnal muscle spasms, exploring the possible causes, risk factors, and effective home remedies. We’ll also look at when it’s time to seek medical attention for persistent or severe leg cramps. Night leg cramps…
Acting Out Dreams Dementia & Parkinsons Link
Acting out dreams predicts later dementia parkinsons – Acting out dreams predicts later dementia and Parkinson’s, a fascinating and potentially crucial link emerging from recent research. This phenomenon, where individuals physically act out their dreams during sleep, may serve as an early indicator of these neurodegenerative diseases. Understanding the types of dream enactment behaviors, their…
What Causes Sleep-Related Hallucinations? A Deep Dive
What causes sleep related hallucinations – What causes sleep-related hallucinations? This fascinating topic delves into the mysterious world of hypnagogic and hypnopompic experiences, exploring the neurological, psychological, and environmental factors that can trigger them. We’ll uncover the science behind these vivid dreamscapes, from the role of sleep deprivation to the influence of medications and underlying…
Study Links Sleep Pattern to Successful Aging
Study links this sleep pattern to successful aging, revealing a fascinating connection between slumber and healthy aging. This research delves into a specific sleep pattern, exploring its characteristics, correlations with successful aging, and potential mechanisms. Understanding this sleep pattern could lead to valuable interventions for promoting healthy aging and well-being in older adults. The study…
Quality Sleep While Taking Cymbalta
Quality sleep while taking Cymbalta can be a challenge for many, but understanding the potential effects and strategies to manage them can make a significant difference. This comprehensive guide explores the relationship between Cymbalta and sleep, from its mechanism of action to individual experiences, and offers practical advice for navigating sleep issues effectively. This exploration…
Can Ambien Affect Your Memory?
Can ambien affect your memory? This exploration delves into the potential impact of Ambien on various types of memory, from the fleeting moments of short-term recall to the lasting imprints of long-term memories. We’ll examine how this sleep aid might affect cognitive functions, the severity and duration of any memory impairment, and the underlying mechanisms…
What is Light Box Therapy? A Comprehensive Guide
What is light box therapy? This therapy uses specialized lights to treat various conditions, primarily impacting mood and sleep patterns. Different types of light boxes emit varying wavelengths, each potentially affecting the body in distinct ways. Understanding the science behind light box therapy, along with the types of light boxes and their applications, is crucial…
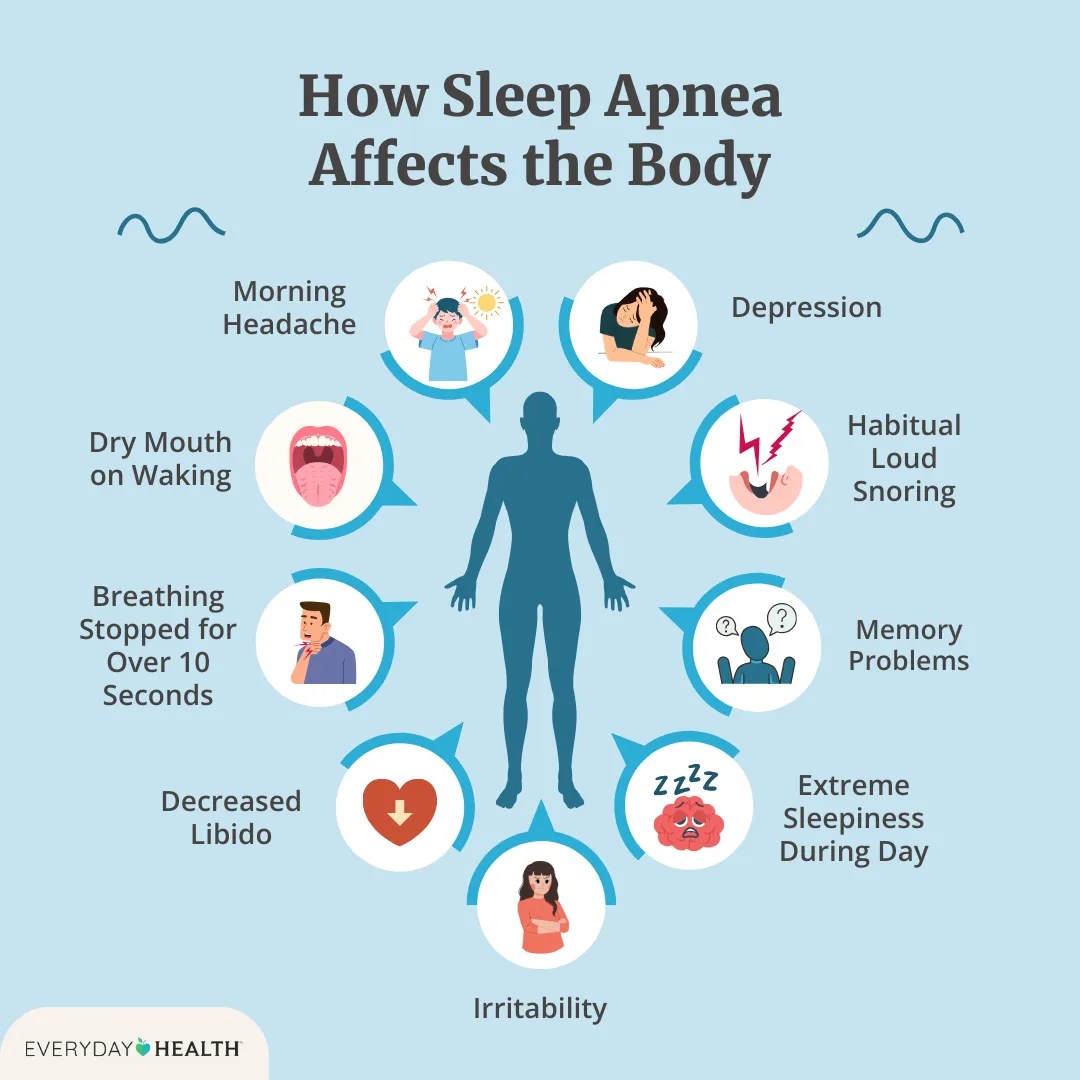
Effects of Sleep Apnea A Deep Dive
Effects of sleep apnea extend far beyond just feeling tired. This comprehensive exploration delves into the various ways sleep apnea impacts your overall health, from the cardiovascular system to cognitive function. We’ll uncover the different types, symptoms, and potential long-term consequences of this often-overlooked condition. Understanding these effects is crucial for early detection and effective…
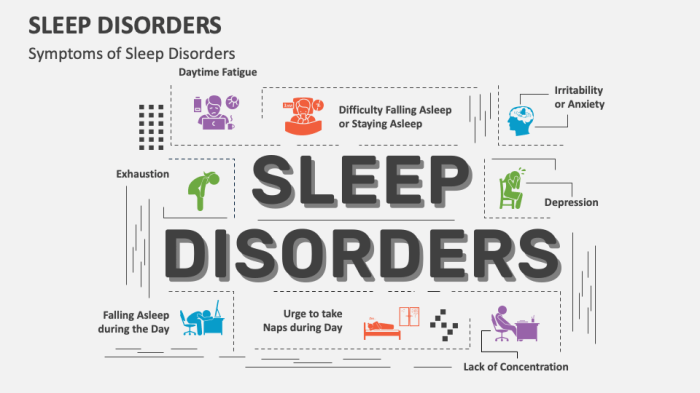
Types of Sleep Disorders A Deep Dive
Types of sleep disorders affect millions worldwide, disrupting not only individual well-being but also impacting society as a whole. From the common struggles of insomnia to the more complex conditions like sleep apnea, understanding the different types and their underlying causes is crucial for effective management and treatment. This exploration delves into the various sleep…