Exercises for arthritic knees are crucial for managing pain and improving mobility. This guide provides a comprehensive overview of various exercises, tailored to different levels of knee arthritis severity. We’ll explore different types of exercises, safety precautions, and how to design a personalized program to help you stay active and comfortable. From strengthening to flexibility,…
Tag: physical therapy
Neck Arthritis Exercises to Avoid A Guide
Neck arthritis exercises to avoid are crucial for preventing further pain and discomfort. Understanding which movements could exacerbate your condition is key to maintaining a healthy neck. This guide explores common exercises that should be modified or avoided altogether, offering practical advice for individuals with neck arthritis. This comprehensive guide will cover various aspects, including…
Physical Therapy for Pectus Excavatum A Deep Dive
Physical therapy for pectus excavatum provides a vital pathway to managing this condition, offering a blend of exercises and techniques to address both the physical and emotional aspects of the condition. It’s a crucial component in the overall treatment plan, helping individuals regain strength, improve posture, and enhance breathing capacity. This comprehensive guide delves into…
What to Wear to Physical Therapy Your Guide
What to wear to physical therapy is more important than you might think. Choosing the right clothes can significantly impact your comfort, performance, and even your mindset during your sessions. This guide will equip you with the knowledge to select clothing that optimizes your therapy experience, from comfortable fabrics to temperature regulation and specific exercise…
Physical Therapy After Ankle Fracture Your Recovery Guide
Physical therapy after ankle fracture is crucial for a successful recovery. This comprehensive guide provides a detailed overview of the entire process, from initial rehabilitation to advanced exercises and returning to pre-injury activities. We’ll explore the different phases, common exercises, and important considerations for managing pain and potential complications. Understanding the specific exercises, the progression…
Exercises for Ankylosing Spondylitis A Guide
Exercises for ankylosing spondylitis are crucial for managing this chronic inflammatory condition. This guide delves into the types of exercises, routines, and considerations needed to effectively incorporate movement into your life with AS. We’ll explore everything from personalized programs to lifestyle integration and how exercise impacts your overall well-being. Understanding the specific needs of those…
Muscle Stiffness Symptoms, Causes & Treatment
Muscle stiffness symptoms causes and treatment – Muscle stiffness symptoms, causes, and treatment: Understanding this complex issue is crucial for managing discomfort and restoring mobility. From everyday aches to more serious conditions, muscle stiffness can stem from various factors, ranging from minor injuries to underlying medical problems. This comprehensive guide delves into the intricacies of…
Physical Therapy After Proximal Humeral Fracture A Guide
Physical therapy after a proximal humeral fracture is crucial for regaining strength, mobility, and function in the shoulder. This comprehensive guide delves into the evaluation, rehabilitation phases, and considerations for various patient populations, ensuring a smooth recovery journey. We’ll cover everything from initial assessments to advanced exercises, addressing common complications and outlining successful return-to-activity strategies….
Physical Therapy After Fracture Hardware Removal Your Recovery Guide
Physical therapy after fracture hardware removal is crucial for a successful recovery. This comprehensive guide provides a detailed overview of the process, from initial assessments to returning to daily activities. We’ll explore the different types of fractures requiring hardware removal, common exercises, pain management strategies, and the importance of gradual mobility restoration. We’ll also discuss…
Functional Reach Test in Physical Therapy A Comprehensive Guide
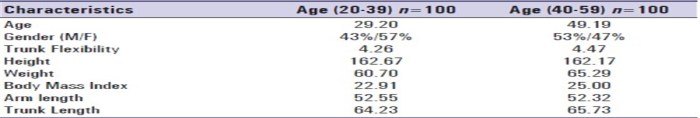
The functional reach test in physical therapy sets the stage for understanding a crucial assessment tool for evaluating functional mobility. This test is used to measure the distance a person can reach forward from a standing position, providing valuable insights into balance and potential risks of falls. Understanding the test’s purpose, administration, interpretation, and limitations…