What does mouth cancer look like? This introduction explores the often-overlooked visual characteristics of this serious condition. Understanding the early signs and symptoms is crucial for prompt detection and treatment. We’ll delve into the different types of oral cancer, their prevalence, and risk factors. Crucially, we’ll look at how to identify cancerous lesions, differentiating them…
Tag: oral health
HIV Mouth Sores Pictures Visual Guide
HIV mouth sores pictures offer a crucial visual aid for understanding the oral manifestations of HIV. Identifying these sores early is vital for proper diagnosis and treatment. This guide will visually illustrate various types of mouth sores associated with HIV, providing clear images and detailed descriptions. The goal is to empower patients and healthcare providers…
Facts About Fluoride Toothpaste A Comprehensive Guide
Facts about fluoride toothpaste are essential for understanding its role in oral health. This guide delves into the history, composition, benefits, and potential risks associated with fluoride toothpaste. We’ll explore different types, usage recommendations, and compare fluoride toothpastes with alternatives. From its historical context in dentistry to the chemical composition of common varieties, this in-depth…
Antibiotics Before Dental Work A Guide
Antibiotics before dental work are a common practice, but understanding the reasons behind it and the potential alternatives is crucial. This guide delves into the rationale for using antibiotics before dental procedures, considering various factors and risks involved. We’ll examine the different types of dental work, the impact of patient history, and alternatives to routine…
Canker Sore on Tongue A Comprehensive Guide
Canker sore on tongue, those pesky little ulcers that pop up in the mouth, can be incredibly frustrating. This guide dives deep into understanding these painful sores, from their causes and symptoms to effective home remedies and when to seek professional help. We’ll explore everything you need to know about identifying, treating, and preventing canker…
Paxlovid Mouth What to Do
Paxlovid mouth what to do? This guide explores the potential oral side effects of Paxlovid, offering practical strategies for managing discomfort, and highlighting the crucial role of professional interventions and patient self-care. Many users experience oral issues while taking Paxlovid, ranging from dry mouth and sores to more severe complications. Understanding the potential problems, along…
Why Do We Have Wisdom Teeth? A Deep Dive
Why do we have wisdom teeth? This question has puzzled scientists and dental professionals for generations. These seemingly vestigial molars, erupting often in our late teens or twenties, have a complex evolutionary history. They weren’t always a source of pain and crowding, but rather, played a crucial role in our ancestors’ survival. This blog post…
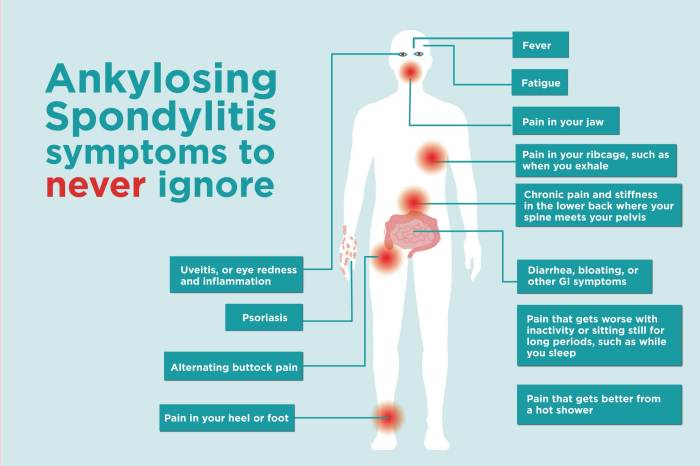
Ankylosing Spondylitis and Teeth Problems A Deep Dive
Ankylosing spondylitis and teeth problems are intricately linked, creating a complex interplay between spinal health and oral well-being. This exploration delves into the specifics of this connection, examining the common oral health concerns associated with AS, the underlying mechanisms, and effective management strategies. This comprehensive guide will cover various aspects of oral health in individuals…
How Long Do Fillings Last? A Deep Dive
How long do fillings last? This crucial question impacts every patient’s oral health journey. Understanding the factors influencing filling longevity, from material type to personal habits, is key to making informed decisions about your dental care. We’ll explore different filling types, common problems, and strategies for maintaining your fillings for years to come. From the…
How to Brush Your Teeth A Comprehensive Guide
How to brush your teeth effectively is crucial for maintaining good oral health. This guide dives deep into the essential steps, from selecting the right tools to mastering the perfect technique. Proper brushing prevents plaque buildup, gum disease, and cavities, leading to a healthier, more confident smile. We’ll explore various techniques for different needs, from…