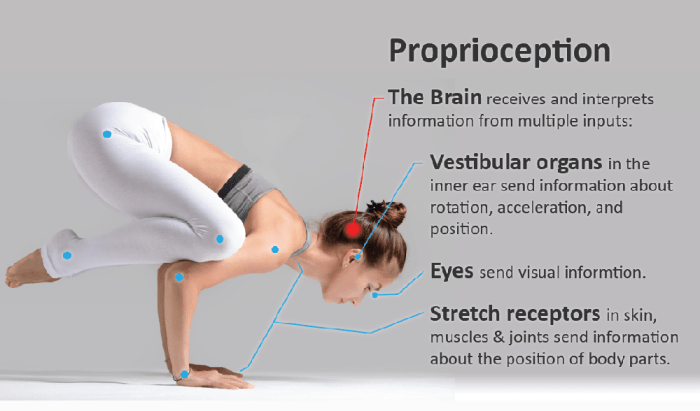
Proprioception in multiple sclerosis lays bare the intricate relationship between the nervous system and our sense of body awareness. This complex topic explores how multiple sclerosis impacts our ability to perceive our body’s position and movement, leading to a cascade of effects on daily activities. We’ll delve into the neurological underpinnings of proprioception, the specific…
Tag: neurological disorders
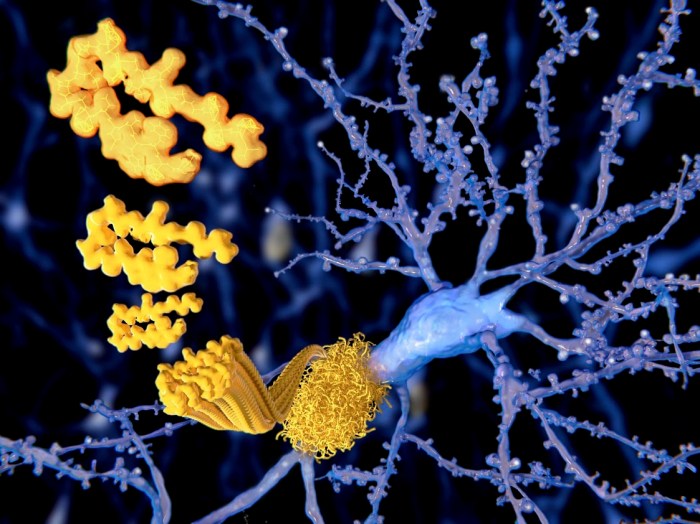
HATTR Amyloidosis with Polyneuropathy A Deep Dive
HATTR amyloidosis with polyneuropathy is a complex and often debilitating condition. This comprehensive look delves into the intricacies of this disease, exploring its underlying mechanisms, clinical presentation, diagnostic criteria, management strategies, prognosis, and the latest research. We’ll examine the challenges faced by patients and their families, and discuss the hope offered by current and future…
Can Macular Degeneration Cause Hallucinations?
Can macular degeneration cause hallucinations? This intriguing question delves into the complex relationship between the eyes, the brain, and vision. Macular degeneration, a leading cause of vision loss, affects the macula, the central part of the retina responsible for sharp central vision. Different types of macular degeneration, like dry and wet, have varying impacts on…
Papilledema Symptoms Causes, Diagnosis, and Treatment
Papilledema symptoms causes diagnosis treatment – Papilledema symptoms, causes, diagnosis, and treatment are crucial for understanding this potentially serious condition. This comprehensive guide delves into the various visual and non-visual symptoms, exploring the underlying causes from intracranial pressure to tumors. We’ll examine diagnostic methods, from ophthalmoscopy to imaging, and discuss the diverse treatment approaches, from…
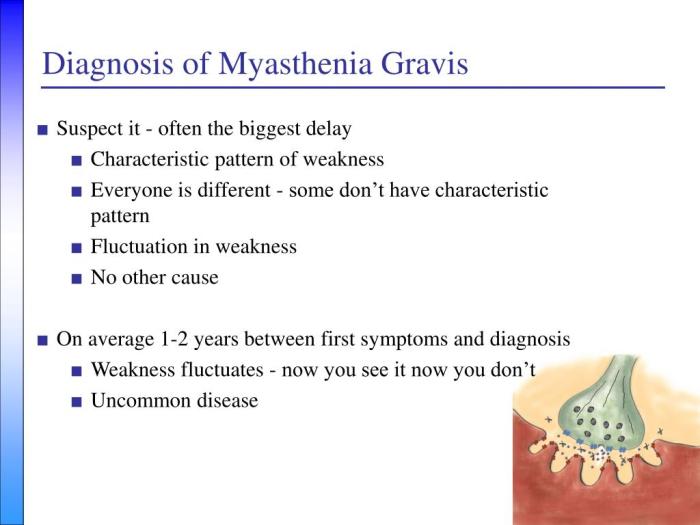
How Myasthenia Gravis Is Diagnosed A Comprehensive Guide
How myasthenia gravis is diagnosed is a crucial process, often involving a multifaceted approach. This journey begins with recognizing the subtle and sometimes overlooked initial symptoms, progressing through neurological examinations, and culminating in a series of diagnostic tests. Understanding the various methods used in the diagnostic process can help patients and their families navigate this…
Tardive Dyskinesia and COVID-19 A Look
Tardive dyskinesia and covid 19 – Tardive dyskinesia and COVID-19: A growing concern is emerging about the potential link between these two conditions. Tardive dyskinesia (TD) is a neurological disorder characterized by involuntary movements, often affecting the face and mouth. Understanding how COVID-19 might impact TD is crucial for healthcare professionals and patients alike. This…
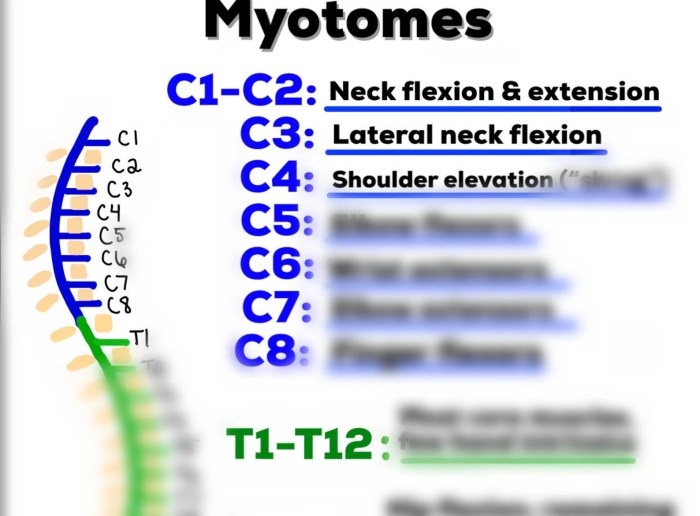
What is a Myotome A Deep Dive
What is a myotome? It’s a crucial concept in understanding how our muscles are controlled by the nervous system. Imagine a specific group of muscles, all working together, coordinated by a particular segment of the spinal cord. That’s essentially a myotome. This isn’t just an academic curiosity; myotome assessment plays a vital role in diagnosing…
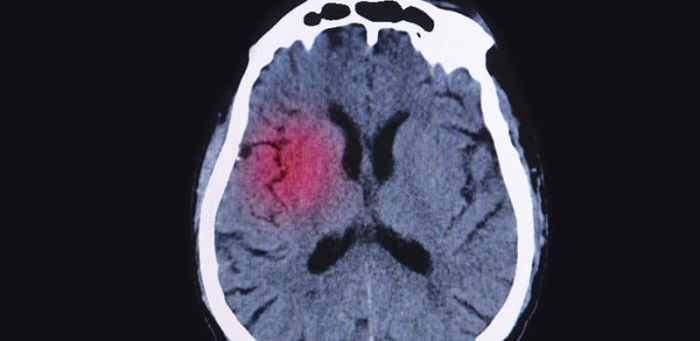
Understanding What is a Small Stroke
What is a small stroke? This in-depth exploration delves into the intricacies of this often-overlooked medical condition, highlighting its defining characteristics, potential causes, diagnostic procedures, and treatment options. We’ll examine the subtle signs and symptoms, distinguish it from a TIA, and explore the long-term effects and recovery strategies. From the initial definition and medical terminology…
Understanding Atonic Seizures What You Need to Know
What are atonic seizures? These are a type of seizure characterized by a sudden loss of muscle tone, leading to a brief period of falling or collapsing. Understanding their causes, symptoms, and treatment is crucial for those affected and their loved ones. This comprehensive guide delves into the intricacies of atonic seizures, providing valuable insights…
Migraine and Multiple Sclerosis Connection Unveiling the Link
Migraine and multiple sclerosis connection: This exploration delves into the intriguing relationship between these two neurological conditions. Migraines, characterized by debilitating headaches, and multiple sclerosis, a chronic autoimmune disease affecting the central nervous system, often share overlapping symptoms. Understanding this connection is crucial for accurate diagnosis and effective treatment strategies. The potential overlap in symptoms,…