Whats the difference between delirium and dementia? These two conditions, though both affecting cognitive function, have vastly different characteristics, onsets, and courses. Understanding these distinctions is crucial for accurate diagnosis and effective treatment. Delirium typically emerges suddenly, often triggered by an underlying medical issue, and involves fluctuating attention and awareness. Dementia, on the other hand,…
Tag: mental health
Signs of Depression in Men Hidden Struggles
Signs of depression in men often manifest differently than in women, leading to delayed recognition and treatment. Societal pressures and cultural norms frequently discourage men from seeking help, masking the underlying issue. This in-depth exploration delves into the various signs, from emotional and behavioral changes to subtle physical indicators. We’ll also discuss the challenges men…
Coping When Loved One Doesnt Recognize You
Coping when loved one doesnt recognize you – Coping when a loved one doesn’t recognize you is a deeply challenging experience, filled with a spectrum of emotions and complex situations. This journey explores the emotional toll of such a situation, from the initial shock and confusion to the potential long-term impact on the relationship. We’ll…
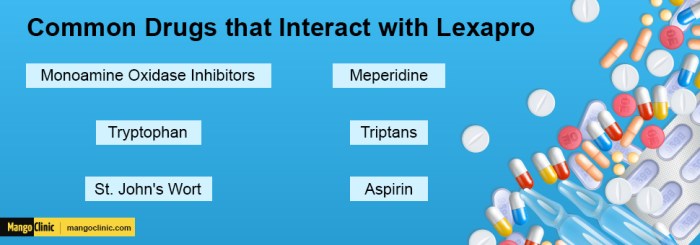
Prozac Fluoxetine vs Lexapro Escitalopram A Deep Dive
Prozac fluoxetine vs lexapro escitalopram: A comparison of these two popular antidepressants, both Selective Serotonin Reuptake Inhibitors (SSRIs), is crucial for individuals seeking effective treatment. This in-depth look examines their mechanisms of action, common side effects, dosage ranges, and potential interactions. Understanding the nuances between these drugs empowers informed decision-making with a healthcare professional. This…
Acute Trauma vs Chronic Trauma Understanding the Differences
Acute trauma vs chronic trauma: This exploration delves into the distinct impacts of sudden, intense experiences versus ongoing, pervasive stress. Understanding these differences is crucial for providing appropriate support and treatment. We’ll examine the physiological and psychological responses, the developmental effects, and the various treatment approaches. Acute trauma often stems from a single, shocking event…
Fear of People Anthropophobia Explained
Fear of people anthropophobia – Fear of people, anthropophobia, is a specific phobia characterized by an intense and persistent fear of other people. It’s different from general social anxiety, often focusing on a broad range of social situations rather than a specific fear of interaction. This fear can vary in severity, from mild discomfort to…
The Effects of Drug Addiction A Deep Dive
The effects of drug addiction are far-reaching and devastating, impacting individuals, families, and communities. This exploration delves into the complex web of consequences, from the initial biological triggers to the long-term societal implications. We’ll examine the immediate physiological and behavioral changes, the lasting damage to physical and mental health, and the profound social and economic…
Ask an Expert HIV Support Groups
Ask an expert HIV support groups sets the stage for a deep dive into the crucial world of support for those living with HIV. We’ll explore the different types of groups, from online forums to in-person meetings, and examine the vital role of members and facilitators. This journey delves into finding the right support, addressing…
Dysphoric Mood Warning Signs Coping Strategies
Dysphoric mood warning signs and how to cope is a crucial guide for understanding and managing emotional distress. This comprehensive resource delves into the nuances of dysphoric moods, from recognizing the initial signs to developing effective coping mechanisms and seeking professional help. We’ll explore various types of dysphoric moods, their triggers, and a range of…
Risks of Sitting Too Long A Health Hazard
Risks of sitting too long can lead to a multitude of health problems, impacting both physical and mental well-being. From musculoskeletal issues to cardiovascular risks, and even mental health concerns, understanding the dangers of prolonged sitting is crucial for maintaining a healthy lifestyle. This exploration delves into the various facets of this sedentary habit, highlighting…