Rapid and extreme mood swings can be incredibly disruptive, impacting daily life and relationships. This exploration delves into the complexities of these intense emotional shifts, examining their causes, triggers, and potential consequences. We’ll uncover the difference between normal mood fluctuations and clinically significant swings, providing valuable insights into understanding and managing these experiences. The article…
Tag: mental health
Borderline Personality Disorder Diagnosis A Deep Dive
Borderline personality disorder diagnosis is a complex process, requiring careful consideration of various factors. This exploration delves into the intricacies of identifying and understanding BPD, from defining the disorder itself to examining the diagnostic process, influencing factors, and even treatment implications. We’ll uncover the nuances of the DSM-5 criteria, explore diagnostic challenges, and analyze the…
What is Self-Care? Your Guide to Well-being
What is self care – What is self-care? It’s more than just a trend; it’s a vital component of a healthy and fulfilling life. This guide delves into the multifaceted world of self-care, exploring its definition, benefits, and practical strategies for incorporating it into your daily routine. We’ll uncover the difference between self-care and selfishness,…
Borderline Personality BPD Triggers Examples & Coping
Borderline personality BPD triggers examples and coping mechanisms are crucial for navigating the challenges of this condition. Understanding the various types of triggers, from interpersonal conflicts to internal thoughts, is the first step in developing effective coping strategies. This guide provides a comprehensive overview of common triggers and offers practical techniques for managing intense emotions…
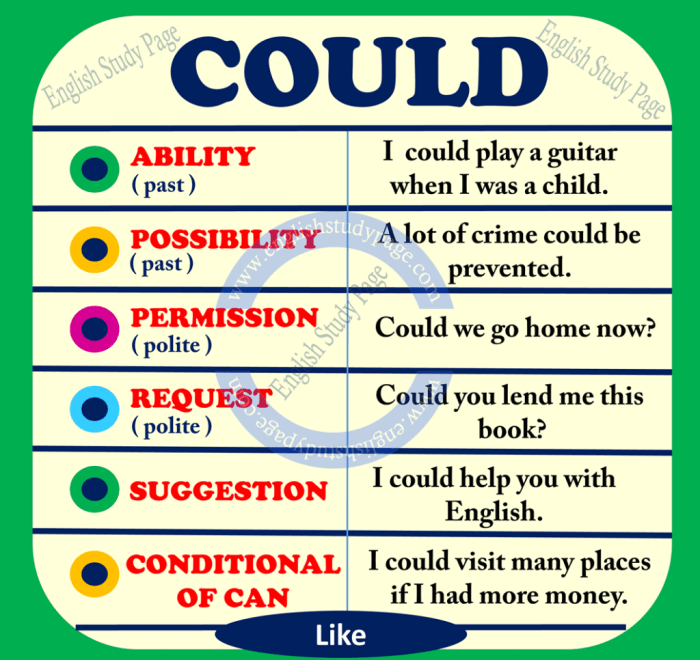
Could Prednisone Cause Mood Swings?
Could prednisone cause mood swings? This question delves into the potential link between the powerful corticosteroid prednisone and fluctuations in mood. Understanding how this medication impacts the body’s neurochemistry is crucial for patients and healthcare providers alike. This exploration investigates the mechanisms behind prednisone’s effect on various neurotransmitters, leading to potential mood changes. Prednisone, often…
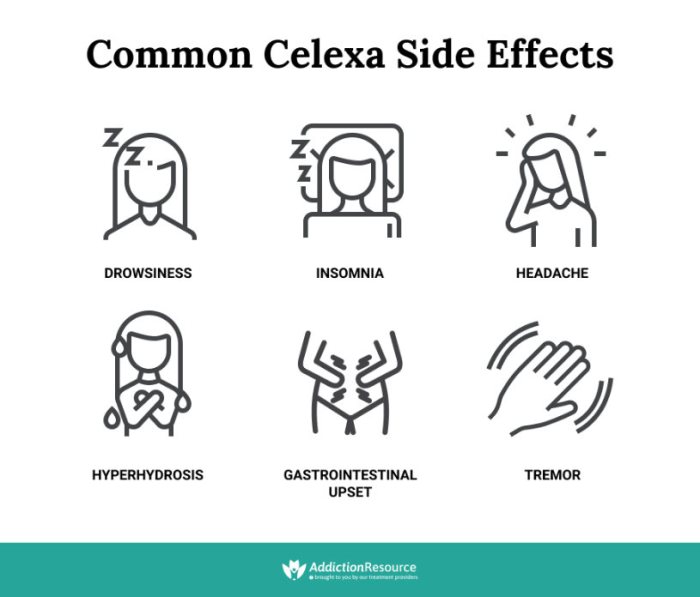
Celexa vs Zoloft Similarities and Differences
Celexa vs Zoloft similarities and differences is a crucial topic for those considering these medications for mental health conditions. Both are selective serotonin reuptake inhibitors (SSRIs), commonly prescribed to alleviate symptoms of depression, anxiety, and other related disorders. Understanding their similarities and differences is essential for informed decision-making alongside a healthcare professional. This comprehensive comparison…
Post SSRI Erectile Dysfunction A Deep Dive
Post SSRI erectile dysfunction is a complex issue affecting many individuals taking selective serotonin reuptake inhibitors (SSRIs). This in-depth exploration delves into the potential link between SSRIs and sexual dysfunction, examining the various mechanisms involved, the symptoms experienced, and available treatment options. We’ll also discuss underlying factors and preventative strategies. Understanding the potential for SSRIs…
How Depression Is Diagnosed A Comprehensive Guide
How depression is diagnosed is a multifaceted process, requiring careful consideration of various factors. From understanding the core symptoms and diagnostic criteria to the crucial role of the clinician and cultural sensitivities, this exploration delves into the complexities of accurately identifying depression. We’ll examine the historical evolution of diagnostic methods, exploring the strengths and weaknesses…
Different Types of OCD A Deep Dive
Different types of OCD sets the stage for this enthralling narrative, offering readers a glimpse into the complexities of this condition. We’ll explore the various obsessions and compulsions that define different OCD experiences, delving into the underlying anxieties and fears that fuel them. Understanding the diverse manifestations of OCD is crucial for comprehending its impact…
How Long Does Postpartum Depression Last? Understanding the Journey
How long does postpartum depression last? This question weighs heavily on the minds of new mothers and their loved ones. It’s a complex journey, marked by a spectrum of experiences, and understanding the timeframe is crucial for navigating this challenging period. This article delves into the duration of postpartum depression (PPD), exploring the factors that…