Itchy hands and feet can be a frustrating and uncomfortable experience. This comprehensive guide delves into the various potential causes, symptoms, diagnosis, treatment options, and preventive measures for this common ailment. Understanding the nuances of itchy hands and feet is key to finding relief and restoring comfort. From skin conditions to allergies and underlying health…
Tag: medical-conditions
Why Do People Die in Their Sleep? Unveiling the Causes
Why do people die in their sleep? This question touches upon a deeply unsettling aspect of human life, prompting us to explore the various factors that can contribute to sudden death during slumber. From underlying medical conditions to sleep disorders, drug interactions, and environmental influences, the causes are multifaceted and often complex. Understanding these factors…
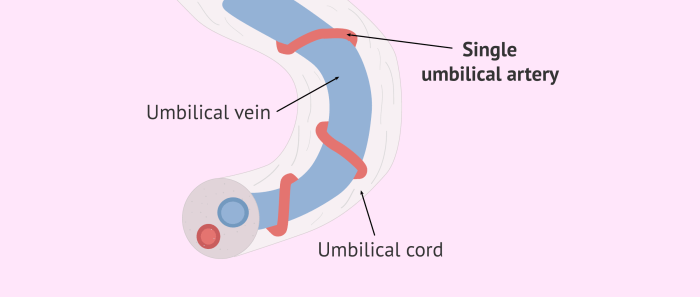
Belly Button Leaking Fluid Causes & Solutions
Belly button leaking fluid can be a concerning symptom, and understanding its possible causes is crucial for appropriate action. This comprehensive guide explores the various medical conditions, infections, and underlying issues that might lead to this discharge, from trauma to recent surgeries. We’ll delve into the potential causes, associated symptoms, when to seek medical attention,…
Why Am I So Tired and Have No Energy Female?
Why am I so tired and have no energy female? This pervasive feeling of exhaustion can stem from a multitude of factors, ranging from underlying medical conditions to lifestyle choices. Understanding the potential causes can be crucial in finding solutions and reclaiming your energy. This exploration delves into the complexities of female fatigue, examining everything…
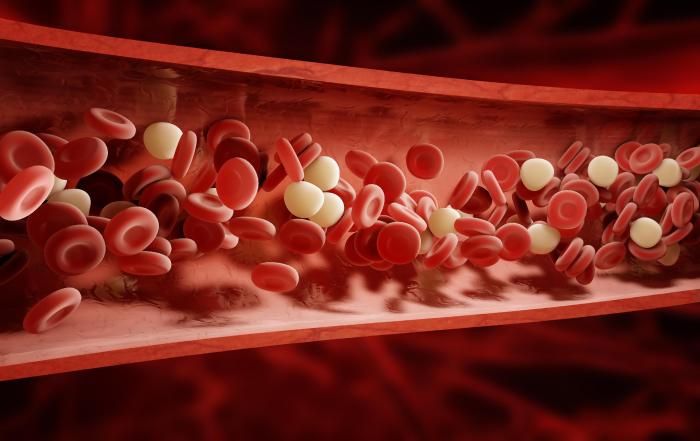
Blood Clots in Urine A Guide
Blood clots in urine can be a serious concern, and understanding the causes, symptoms, and potential treatments is crucial. These clots, while often alarming, can stem from various factors, ranging from relatively benign issues to more significant underlying medical conditions. This guide provides a comprehensive overview of blood clots in urine, covering everything from initial…