Why do I sweat so easily? This question plagues many, leading to discomfort and concern. Understanding the underlying reasons for excessive sweating is crucial for finding relief and improving overall well-being. This comprehensive guide explores the medical conditions, lifestyle factors, and physiological mechanisms that contribute to excessive perspiration, providing insights into diagnosis, treatment, and prevention…
Tag: medical-conditions
Secondary Headache Overview and More Understanding the Causes
Secondary headache overview and more delves into the complexities of headaches beyond the familiar. This exploration examines the crucial distinction between primary headaches, often idiopathic, and secondary headaches, where an underlying medical condition triggers the pain. Understanding the causes, symptoms, and diagnostic processes is key to effective management and treatment. Knowing how to differentiate these…
Back Pain A Lung Cancer Symptom
Back pain as a symptom of lung cancer is a complex and often overlooked possibility. While back pain is frequently associated with other conditions, its unusual manifestation in relation to lung cancer warrants careful consideration. This exploration delves into the potential link, highlighting the various ways back pain can manifest, its location, characteristics, and the…
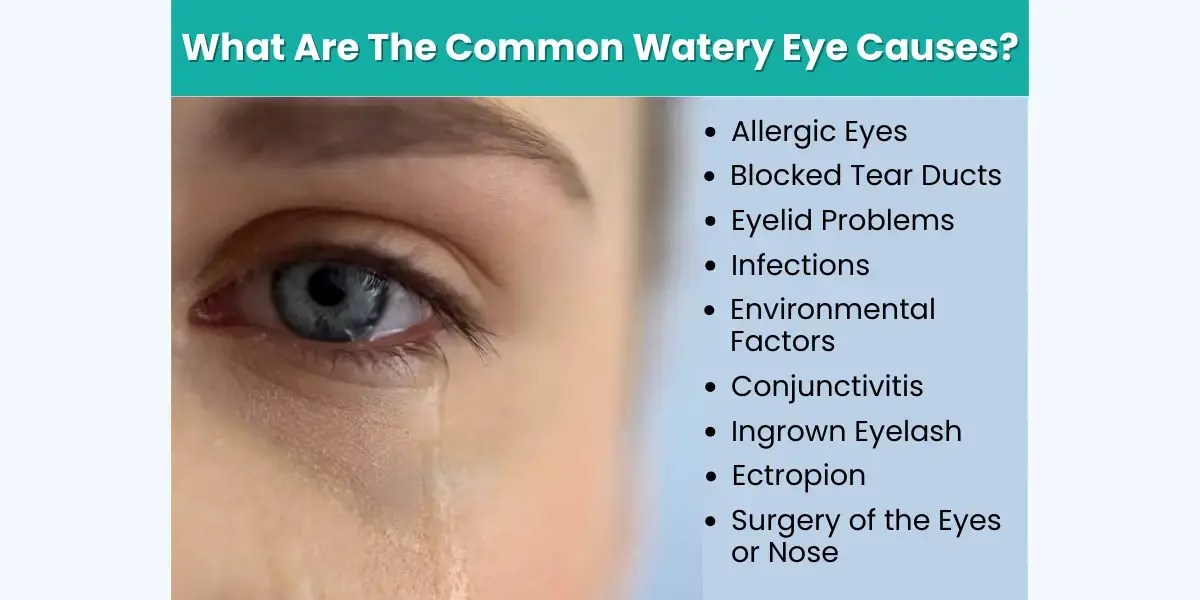
What Causes Watery Eyes? A Comprehensive Guide
What causes watery eyes? This insightful exploration delves into the myriad reasons behind those persistent, uncomfortable tears. From common allergies and infections to underlying medical conditions and environmental factors, we’ll uncover the root causes and provide a comprehensive understanding of this prevalent eye issue. This detailed guide will explore potential triggers, symptoms, diagnostic procedures, treatment…
Right Sided Chest Pain Symptoms & Causes
Right sided chest pain symptoms and possible causes can range from mild discomfort to serious medical concerns. Understanding the potential triggers and how to differentiate between various issues is crucial for appropriate action. This comprehensive guide delves into the common and less frequent causes of right-sided chest pain, considering age, specific populations, and when to…
Muscle Stiffness Symptoms, Causes & Treatment
Muscle stiffness symptoms causes and treatment – Muscle stiffness symptoms, causes, and treatment: Understanding this complex issue is crucial for managing discomfort and restoring mobility. From everyday aches to more serious conditions, muscle stiffness can stem from various factors, ranging from minor injuries to underlying medical problems. This comprehensive guide delves into the intricacies of…
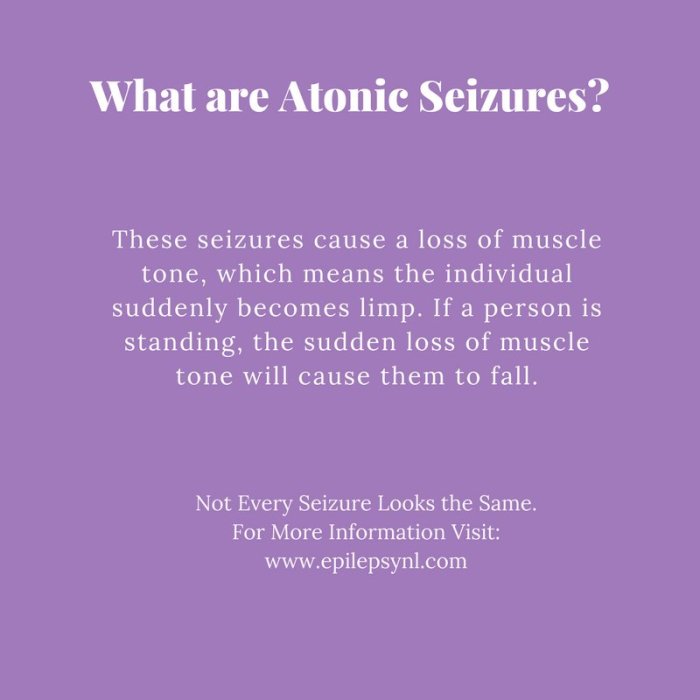
Understanding Atonic Seizures What You Need to Know
What are atonic seizures? These are a type of seizure characterized by a sudden loss of muscle tone, leading to a brief period of falling or collapsing. Understanding their causes, symptoms, and treatment is crucial for those affected and their loved ones. This comprehensive guide delves into the intricacies of atonic seizures, providing valuable insights…
Nkem Osians Uterine Fibroid Story A Personal Account
Nkem osian uterine fibroid story – Nkem Osian’s uterine fibroid story is a powerful account of navigating a health challenge with resilience and grace. This journey delves into the personal experiences, medical treatments, and societal factors surrounding uterine fibroids. From understanding the condition itself to exploring the emotional and practical impacts, this narrative offers a…
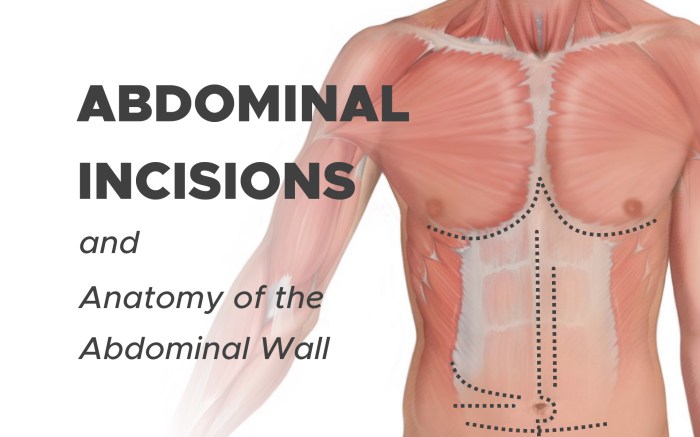
Abdominal Swelling and Bloating Understanding the Causes
Abdominal swelling and bloating can be uncomfortable and frustrating. This comprehensive guide explores the various aspects of this common issue, from defining the symptoms to understanding potential causes, diagnostic procedures, and effective treatment options. We’ll delve into the physiological mechanisms behind the distention, differentiate between types of swelling, and discuss the role of different organs…
Feeling of Something Stuck in Throat Causes & Solutions
Feeling of something stuck in throat can be incredibly uncomfortable and worrisome. This blog post dives deep into the possible causes, from everyday irritants to more serious medical conditions. We’ll explore potential triggers, diagnostic considerations, management strategies, and preventive measures to help you understand this common issue. From anxiety to specific foods, a variety of…