The health benefits of bifobacterium – The health benefits of bifidobacterium are increasingly recognized for their positive impact on human well-being. This comprehensive exploration delves into the fascinating world of these beneficial bacteria, examining their role in digestive health, immune support, and potential impact on overall wellness. We’ll uncover how bifidobacteria work, their various species…
Tag: immune system
Can Allergies Cause Body Aches?
Can allergies cause body aches? This question delves into the fascinating connection between allergic reactions and the often-misunderstood discomfort of body aches. Understanding the intricate mechanisms behind this link is key to recognizing and managing these symptoms effectively. From the initial triggers to the physiological responses, this exploration unravels the mysteries surrounding allergic body aches,…
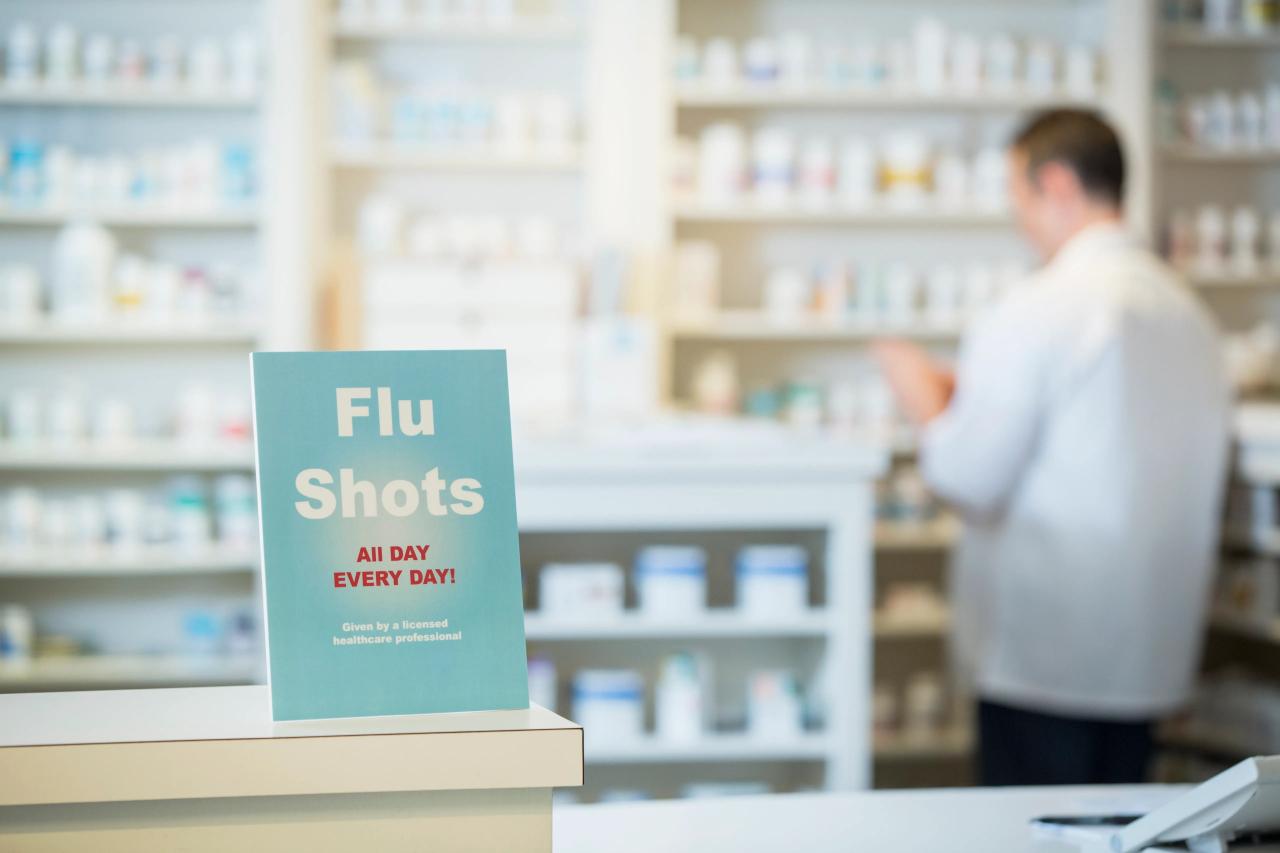
Why Did I Get Sick After a Flu Shot?
Why did I get sick after a flu shot? This question plagues many after receiving the annual vaccination. Understanding the flu shot process, potential underlying causes, and factors influencing post-shot illness is crucial. We’ll delve into the science behind the shot, examine common side effects, and explore how individual differences can affect the body’s response….
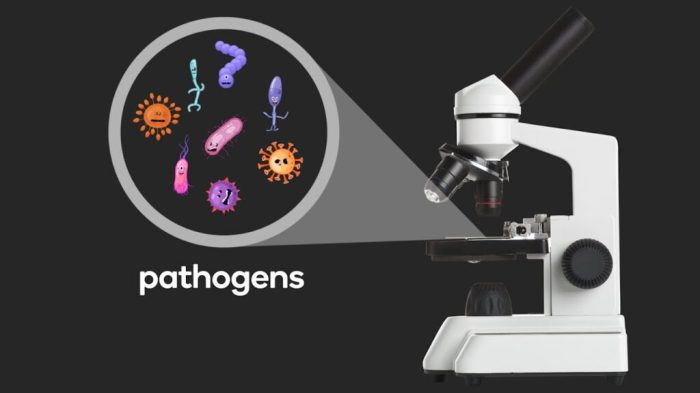
What is a Pathogen? A Deep Dive
What is a pathogen? This exploration delves into the fascinating world of disease-causing organisms, from the microscopic to the complex. We’ll unravel the mysteries behind these tiny invaders, examining their structures, functions, and the intricate ways they interact with their hosts. Understanding pathogens is crucial for comprehending human health and developing effective strategies to combat…
Can Allergies Cause Loss of Taste and Smell?
Can allergies cause loss of taste and smell? This intriguing question delves into the complex interplay between our immune system and sensory perception. Allergies, triggered by our bodies’ overreaction to harmless substances, can manifest in a wide range of symptoms, from the familiar runny nose to more subtle effects like changes in taste and smell….
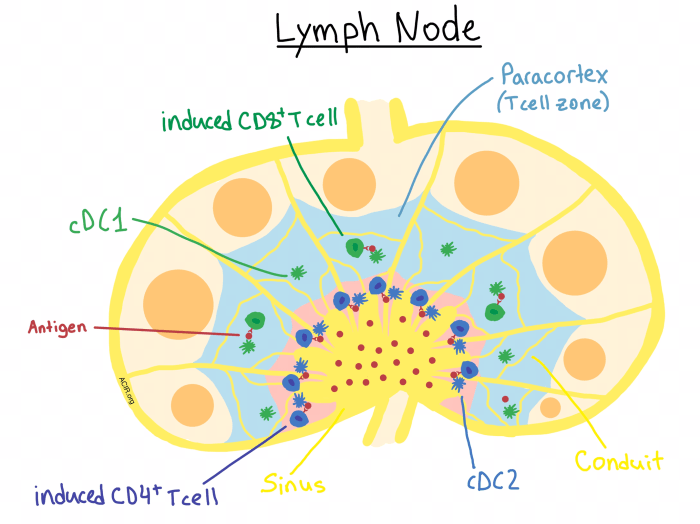
Understanding the Purpose of Lymph Nodes A Deep Dive
Understanding the purpose of lymph nodes sets the stage for this enthralling narrative, offering readers a glimpse into the intricate network of these vital structures within the human body. This exploration delves into the anatomical structure of lymph nodes, revealing their role in maintaining a healthy immune system. We’ll examine how these tiny filters work…
How Long Does a Flu Shot Last? Your Guide
How long does a flu shot last? This crucial question affects everyone’s decision to get vaccinated. Understanding the duration of protection offered by flu shots is key to making informed choices about your health. Different factors, like the specific flu strain, your immune system, and even underlying health conditions, all play a role in how…
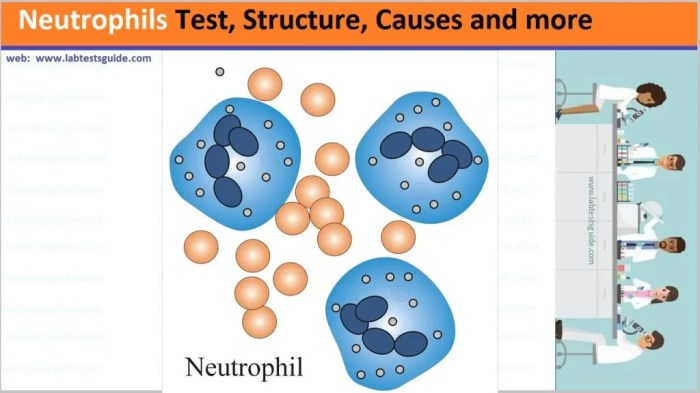
What are Neutrophils P2 A Deep Dive
What are neutrophils p2? This exploration delves into the crucial role of neutrophils, a type of white blood cell, within the context of P2. We’ll uncover their significance in the immune system, examining their structure, function, and behavior in a P2 environment. From the intricacies of their normal function to their response in P2 conditions,…
Do Fevers Cause Brain Damage? Exploring the Risks
Do fevers cause brain damage? This question is a crucial one for parents and healthcare professionals alike. While fevers are a natural part of the immune response, understanding the potential risks and protective factors is key to ensuring a healthy outcome. This blog post delves into the complex relationship between fever and brain damage, exploring…
Flu Shot While Sick What to Expect
What will happen if i get a flu shot while im sick – What will happen if I get a flu shot while I’m sick? This post dives into the potential effects of receiving a flu shot when you’re already experiencing flu-like symptoms. We’ll explore how your body’s immune response might be impacted, examine the…