Magnesium for constipation and ibsc – Magnesium for constipation and IBS-C: This comprehensive guide explores the vital role of magnesium in digestive health, delving into its potential benefits for managing constipation and irritable bowel syndrome with constipation (IBS-C). We’ll examine the science behind magnesium’s impact, discuss various forms and dosages, and provide actionable strategies for…
Tag: gut health
Does Iron Cause Constipation? A Deep Dive
Does iron cause constipation? This exploration delves into the complex relationship between iron intake and digestive health. Understanding the role of iron in the body, the various forms of iron, and their absorption processes is crucial to comprehending this connection. We’ll also examine how individual differences, diet, and medications might influence this relationship. Iron, an…
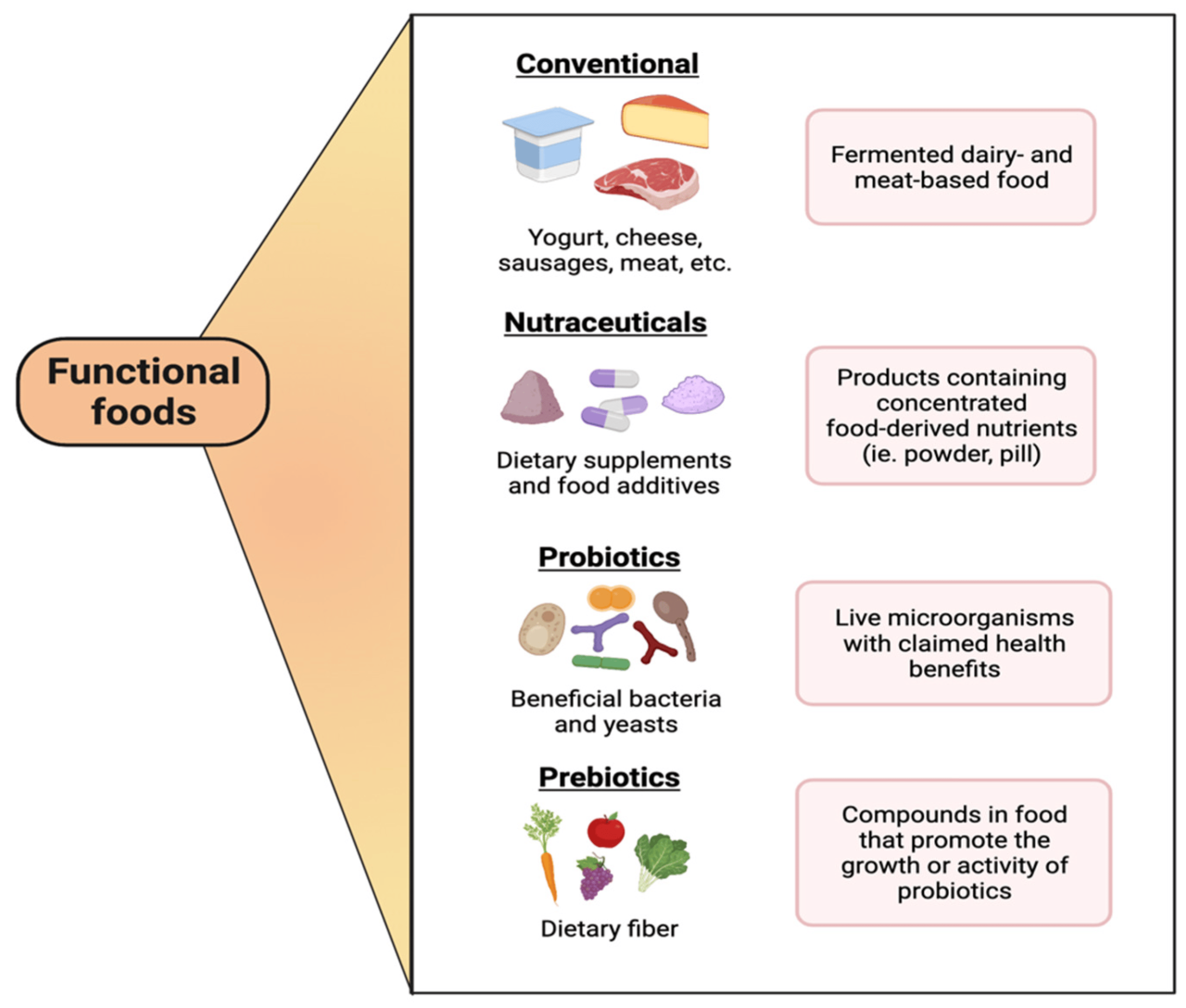
The Health Benefits of Bifidobacterium A Deep Dive
The health benefits of bifobacterium – The health benefits of bifidobacterium are increasingly recognized for their positive impact on human well-being. This comprehensive exploration delves into the fascinating world of these beneficial bacteria, examining their role in digestive health, immune support, and potential impact on overall wellness. We’ll uncover how bifidobacteria work, their various species…
Undigested Food in Stool A Deep Dive
Undigested food in stool sets the stage for this enthralling narrative, offering readers a glimpse into the complex world of digestive health. We’ll explore the various causes, symptoms, dietary factors, medical conditions, and even the diagnostic process related to this common issue. From the crucial role of enzymes to the impact of stress, this comprehensive…
How Long Does Constipation Last? A Deep Dive
How long does constipation last? This isn’t just an annoying question; understanding the duration is crucial for effective management. From mild discomfort to severe distress, the length of time constipation lingers varies significantly. This exploration delves into the factors influencing duration, from dietary changes to underlying health issues, providing insights into when to seek professional…
Can Antibiotics Cause Yeast Infections? Intor
Can antibiotics cause yeast infections intor? This is a common concern for people taking antibiotics, as these powerful drugs can disrupt the delicate balance of bacteria in the body. Understanding how antibiotics work and their potential impact on the gut microbiome is crucial in navigating this issue. This post will delve into the mechanisms by…
Candida Diet Foods to Avoid A Comprehensive Guide
Candida diet foods to avoid are crucial for managing or preventing Candida overgrowth. This guide delves into a comprehensive list of problematic foods, categorized by food group. We’ll explore the science behind why certain foods fuel Candida yeast and offer practical tips for identifying and avoiding them, even when eating out. Discover hidden sources of…
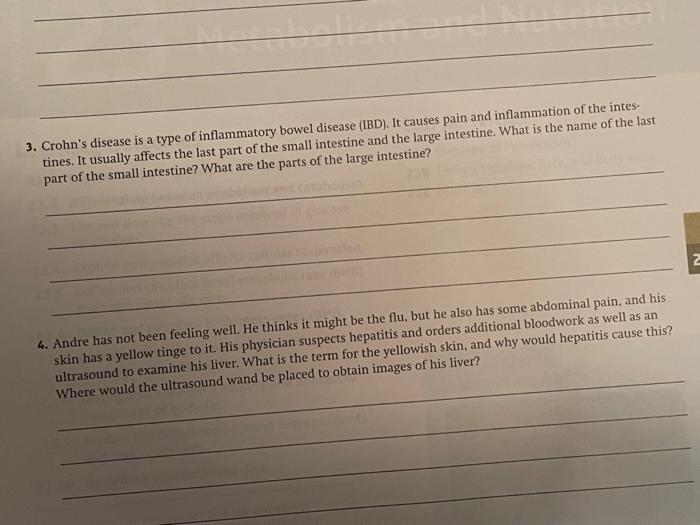
What is Crohns Colitis? A Deep Dive
What is crohns colitis – What is Crohn’s Colitis? This chronic inflammatory condition affects the digestive tract, causing a range of symptoms and impacting daily life. Understanding the nuances of this complex disease, from its causes and stages to potential complications and treatment options, is crucial for those affected and those seeking to learn more….
Anxiety Stress and Diarrhea Understanding the Link
Anxiety stress and diarrhea are often intertwined, with the connection running deeper than many realize. This blog post delves into the physiological mechanisms linking anxiety and stress to digestive issues like diarrhea. We’ll explore the role of the autonomic nervous system, the impact on the gut microbiome, and common symptoms. Understanding this complex interplay is…
Can Probiotics Help Acid Reflux?
Can probiotics help with acid reflux? This question sparks curiosity and debate among those seeking natural remedies for this common digestive ailment. Acid reflux, characterized by the burning sensation in the chest, often arises from stomach acid backing up into the esophagus. While conventional treatments exist, many people explore alternative approaches, including probiotics. This exploration…