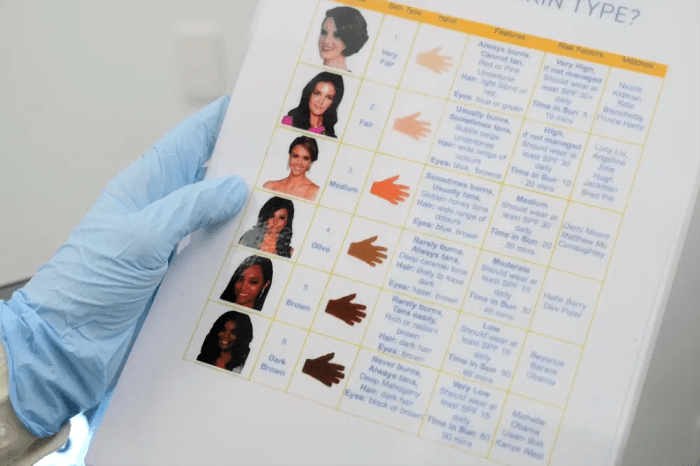
Foods to avoid with macular degeneration are crucial for managing this condition. This guide dives into the specific dietary choices that can either support or hinder your eye health. Understanding which foods contribute to macular degeneration’s progression and which ones offer protective antioxidants is key to preserving vision. Macular degeneration, a common age-related eye disease,…
Tag: eye health
Can Macular Degeneration Cause Hallucinations?
Can macular degeneration cause hallucinations? This intriguing question delves into the complex relationship between the eyes, the brain, and vision. Macular degeneration, a leading cause of vision loss, affects the macula, the central part of the retina responsible for sharp central vision. Different types of macular degeneration, like dry and wet, have varying impacts on…
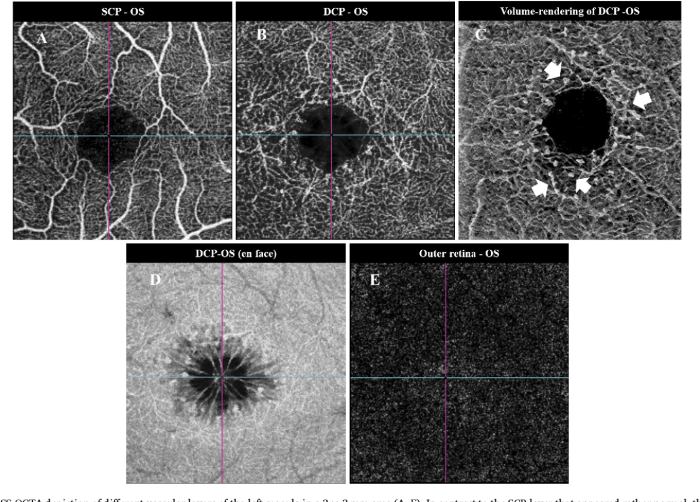
Macular Telangiectasia Type Two A Comprehensive Guide
Macular telangiectasia type two (MT2) is a chronic eye condition that affects the macula, the central part of the retina responsible for sharp, central vision. This guide delves into the intricacies of MT2, exploring its characteristics, causes, diagnosis, management strategies, and the impact it has on patients’ lives. We’ll cover everything from the early stages…
Dry Eyes After Cataract Surgery A Guide
Dry eyes after cataract surgery is a common issue, and understanding the reasons behind it, the symptoms, and effective treatments is crucial for a smooth recovery. This guide delves into the various aspects of dry eye syndrome following cataract surgery, from the initial onset to long-term management. Cataract surgery, while improving vision, can disrupt the…
Dry Eyes in Kids A Comprehensive Guide
Dry eyes in kids sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset. This condition, while sometimes overlooked, can significantly impact a child’s well-being and vision. Understanding the nuances of dry eye syndrome in children, from its symptoms…
Maximize Dry Eye Treatment A Comprehensive Guide
Maximize dry eye treatment is crucial for achieving optimal comfort and vision. This comprehensive guide explores the multifaceted aspects of dry eye, from understanding its causes and symptoms to maximizing treatment outcomes and embracing emerging therapies. We’ll delve into the science behind dry eye, compare current treatments, and discuss personalized approaches to management. The article…
How to Cure Dry Eyes A Comprehensive Guide
How to cure dry eyes? This comprehensive guide dives deep into understanding, diagnosing, and treating dry eye syndrome. We’ll explore the various causes, symptoms, and stages of this common condition, and equip you with effective treatment options, from over-the-counter remedies to lifestyle changes. From understanding the intricate tear production process to exploring preventative measures and…
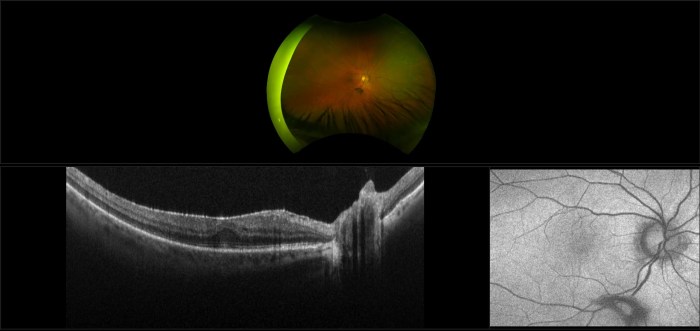
Epiretinal Membrane Retinal Scar Tissue A Deep Dive
Epiretinal membrane retinal scar tissue forms a delicate yet significant threat to vision. This intricate web of scar tissue, often developing on the retina, can lead to a range of visual disturbances. Understanding its formation, diagnosis, and treatment options is crucial for effective management and preserving sight. This post will explore the specifics of this…
Dry Eye Syndrome Facts A Comprehensive Guide
Dry eye syndrome facts are crucial for understanding this common condition. It affects millions, causing discomfort and impacting daily life. This guide delves into the various types, causes, symptoms, diagnoses, and treatments available. We’ll explore how age, lifestyle, and medical conditions play a role, as well as the effectiveness of different management strategies. Get the…
Bulls Eye Maculopathy Overview and More
Bull s eye maculopathy overview and more – Bull’s eye maculopathy overview and more delves into the intricacies of this eye condition. It explores the defining characteristics, underlying mechanisms, and visual field impact. We’ll also examine different types, diagnostic methods, risk factors, management strategies, prognosis, visual rehabilitation, and case studies. Get a comprehensive understanding of…