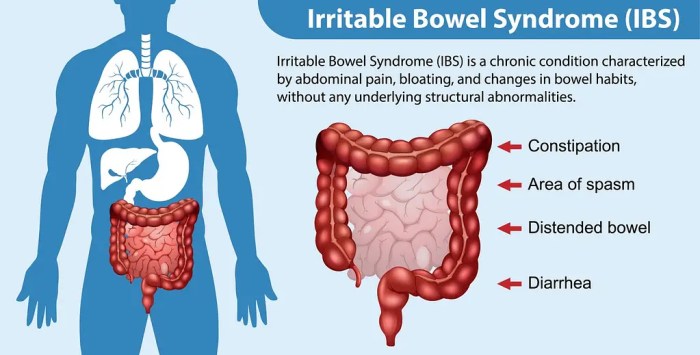
Facts about irritable bowel syndrome: Understanding this common digestive disorder is crucial for effective management. IBS affects millions worldwide, causing a range of uncomfortable symptoms. This guide delves into the complexities of IBS, exploring its types, potential causes, diagnostic methods, treatment options, and lifestyle modifications. We’ll also discuss coping strategies, potential complications, and the latest…
Tag: digestive health
When Should I Worry About Passing Too Much Gas?
When should I worry about passing too much gas? This common digestive issue can be frustrating, but understanding what’s normal and when to seek help is key. We’ll explore the science behind gas production, the signs that something might be amiss, potential underlying medical conditions, and lifestyle changes that can help manage it. From understanding…
6 Foods to Soothe IBS Naturally
6 foods to help soothe ibs symptoms naturally offer a natural approach to managing Irritable Bowel Syndrome (IBS). This guide explores specific foods, their potential benefits, and how they can help alleviate IBS symptoms. We’ll delve into the science behind these foods and provide practical dietary recommendations for incorporating them into your daily life. IBS…
Best Fruit for Constipation Relief
Best fruit for constipation? This deep dive explores the surprising power of fruits to tackle digestive woes. We’ll unpack everything from understanding different types of constipation to discovering the top fruits for relieving it, and even explore fruit-based supplements. Get ready to learn which fruits can be your secret weapon against sluggish bowels! Constipation can…
Best Time of Day for Kefir & Gut Health
Best time of day drink kefir gut health is a crucial aspect for maximizing its potential benefits. Understanding the ideal time to consume kefir, alongside the impact of meal timing and individual factors, is key to optimizing its effects on gut health. From its probiotic-rich nature to its role in digestion, kefir offers a compelling…
Beyond Sauerkraut Gut-Boosting Foods
Foods with more gut health benefits than sauerkraut are out there! Beyond the familiar tang of sauerkraut, a world of fermented and other foods holds powerful potential for a thriving gut microbiome. These foods offer a wealth of prebiotics and probiotics, impacting digestion, immunity, and even mood. We’ll delve into the specific ways these foods…
Facts About Ulcerative Colitis A Comprehensive Guide
Facts about ulcerative colitis delves into the complexities of this chronic inflammatory bowel disease. Understanding the causes, symptoms, and treatment options is crucial for those affected and those seeking to learn more. This comprehensive guide explores the various aspects of ulcerative colitis, from its definition and characteristics to the latest research and dietary considerations. We’ll…