Foods to avoid with macular degeneration are crucial for managing this condition. This guide dives into the specific dietary choices that can either support or hinder your eye health. Understanding which foods contribute to macular degeneration’s progression and which ones offer protective antioxidants is key to preserving vision. Macular degeneration, a common age-related eye disease,…
Tag: diet
Protein Weight Gain or Loss Your Ultimate Guide
Protein weight gain or loss is a complex topic, but understanding the role of protein in your body is key to achieving your fitness goals. This comprehensive guide delves into the science behind protein’s impact on weight management, from building muscle to shedding fat. We’ll explore different protein sources, optimal intake strategies, and potential health…
Does Watermelon Trigger Migraines? A Deep Dive
Does watermelon trigger migraines? This intriguing question delves into the potential connection between this refreshing summer fruit and the debilitating headaches of migraines. We’ll explore the nutritional profile of watermelon, the characteristics of migraines, and the scientific understanding of food-related triggers, examining potential mechanisms and individual sensitivities. The discussion will also touch upon how watermelon…
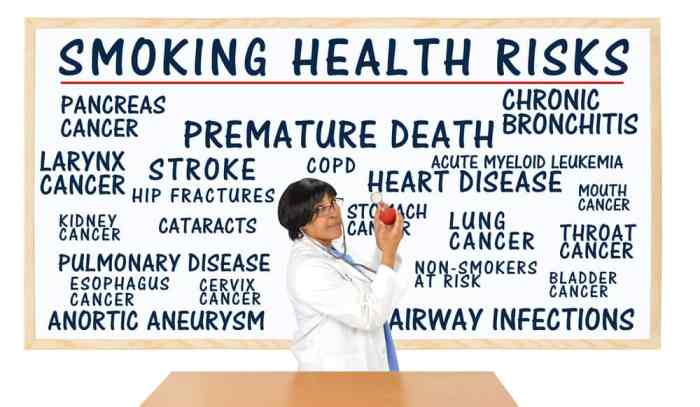
Things to Stop for a Longer Life
Things to stop if you want to live longer: This post delves into crucial lifestyle choices that can significantly impact your lifespan. We’ll explore the negative effects of unhealthy habits and offer actionable strategies to cultivate healthier practices. From diet and exercise to stress management and sleep hygiene, we’ll cover a comprehensive approach to a…
Anti-Inflammatory Diet for Psoriasis A Guide
Anti inflammatory diet for psoriasis – Anti-inflammatory diet for psoriasis is a powerful approach to managing this chronic skin condition. It’s not just about avoiding certain foods, but about understanding how your diet directly impacts inflammation and your psoriasis symptoms. This comprehensive guide explores the principles, food choices, and practical strategies to create a personalized…
Why Is It So Hard to Cut Back on Sodium?
Why is it so hard to cut back on sodium? This isn’t just about willpower; it’s a complex interplay of physiological cravings, ingrained habits, and the pervasive presence of sodium in processed foods. We’ll delve into the science behind salt cravings, explore the sneaky ways food manufacturers add sodium, and uncover the psychological factors that…
Does Drinking Water Help You Lose Weight?
Does drinking water help you lose weight? This intriguing question delves into the surprising ways hydration can influence your body’s metabolism, appetite, and overall calorie intake. We’ll explore the science behind how water impacts your body’s functions and whether it can truly be a key player in your weight loss journey. From boosting metabolism to…
Foods to Avoid with UTI A Dietary Guide
Foods to avoid with UTI can significantly impact your recovery. Understanding which foods might worsen your symptoms is key to managing this common infection effectively. This guide explores the relationship between diet and UTIs, providing insights into specific foods to limit or avoid, along with strategies for hydration and balanced meal plans. We’ll delve into…
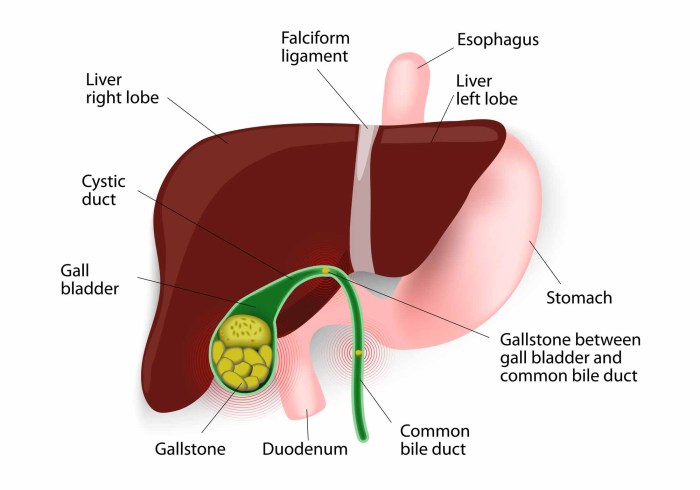
Gallbladder Disease Causes and Risk Factors
Gallbladder disease causes and risk factors are multifaceted, encompassing lifestyle choices, genetics, and underlying medical conditions. Understanding these elements is crucial for proactive health management. This exploration delves into the interplay of diet, obesity, family history, and other influences that contribute to gallbladder issues. We’ll examine the role of various factors in increasing your risk…
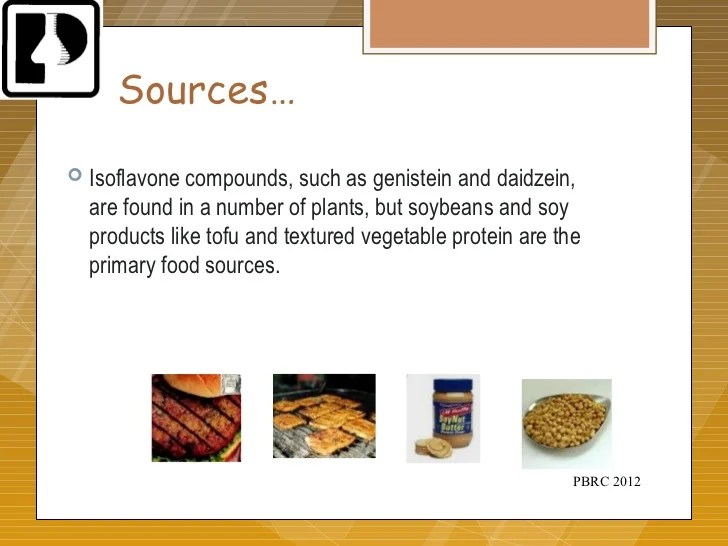
Isoflavones Benefits Side Effects, Dosage, and Interactions
Isoflavones benefits side effects dosage and interactions are a complex topic, but understanding the nuances can be key to harnessing their potential. These plant compounds, found in various foods, are gaining attention for their potential health benefits. However, it’s crucial to consider the potential side effects, appropriate dosage, and possible interactions with other substances. This…