How hyperkalemia is diagnosed involves a multifaceted approach, starting with a thorough patient history and physical examination. This comprehensive guide details the key steps, from initial assessment to advanced laboratory testing and imaging techniques. Understanding the nuances of each stage is crucial for accurate diagnosis and effective treatment. The diagnostic process for hyperkalemia begins with…
Tag: diagnosis
Visual Clues to Dementia Diagnosis Early Detection
Visual clues to dementia diagnosis are subtle yet significant indicators that can aid in early detection. This blog post explores the various visual cues potentially associated with dementia, ranging from subtle changes in facial expressions to alterations in posture and eye contact. Understanding these visual indicators can be crucial for early intervention and support for…
How Depression Is Diagnosed A Comprehensive Guide
How depression is diagnosed is a multifaceted process, requiring careful consideration of various factors. From understanding the core symptoms and diagnostic criteria to the crucial role of the clinician and cultural sensitivities, this exploration delves into the complexities of accurately identifying depression. We’ll examine the historical evolution of diagnostic methods, exploring the strengths and weaknesses…
Fatigue Symptoms Causes, Diagnosis, and Treatment
Fatigue symptoms causes diagnosis and treatment is a complex issue affecting many people. This in-depth exploration dives into the various facets of fatigue, from its different forms and potential causes to effective diagnostic methods and treatment strategies. Understanding the nuances of fatigue, including its physiological and psychological roots, is crucial. This article will explore the…
Asymptomatic Definition Importance and Controversy
Asymptomatic definition importance and controversy is a complex and crucial aspect of public health. Understanding how we define the absence of symptoms is essential for effective disease prevention and control strategies. This multifaceted issue involves diverse perspectives, ranging from medical definitions to public health implications, ethical considerations, and practical challenges in identification. Different medical and…
Secondary Headache Overview and More Understanding the Causes
Secondary headache overview and more delves into the complexities of headaches beyond the familiar. This exploration examines the crucial distinction between primary headaches, often idiopathic, and secondary headaches, where an underlying medical condition triggers the pain. Understanding the causes, symptoms, and diagnostic processes is key to effective management and treatment. Knowing how to differentiate these…
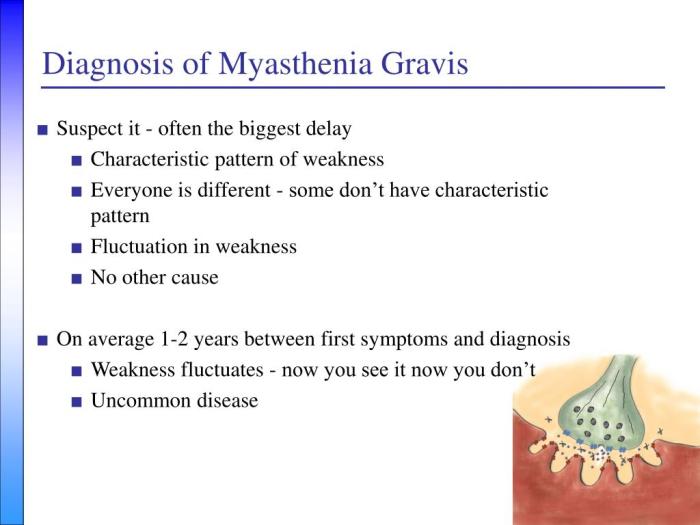
How Myasthenia Gravis Is Diagnosed A Comprehensive Guide
How myasthenia gravis is diagnosed is a crucial process, often involving a multifaceted approach. This journey begins with recognizing the subtle and sometimes overlooked initial symptoms, progressing through neurological examinations, and culminating in a series of diagnostic tests. Understanding the various methods used in the diagnostic process can help patients and their families navigate this…
Signs of Liver Disease Early Detection Matters
Signs of liver disease can be subtle, often overlooked, but early detection is crucial. This guide delves into the various indicators, from common symptoms to risk factors, empowering you to understand your liver health better. We’ll explore different types of liver disease, their causes, and how to recognize the early warning signs. From digestive issues…
How Autoimmune Hepatitis Is Diagnosed A Comprehensive Guide
How autoimmune hepatitis is diagnosed is a crucial step in ensuring timely and effective treatment. This intricate process involves a multifaceted approach, combining various tests and assessments to pinpoint the presence and severity of this condition. Understanding the diagnostic journey is vital for both patients and healthcare professionals alike, and this guide delves into the…
How Graft-Versus-Host Disease GvHD Is Diagnosed
How graft versus host disease GvHD is diagnosed is a crucial aspect of patient care. This comprehensive guide delves into the intricacies of identifying GvHD, from understanding its underlying mechanisms to employing various diagnostic tools. We’ll explore the different types of GvHD, their clinical manifestations, and the essential factors to consider when evaluating a patient…