Ask an expert how does asthma impact daily life? This exploration delves into the multifaceted ways asthma affects everyday routines, from physical exertion and sleep to social interactions and mental well-being. We’ll examine how varying asthma severities influence daily life, and uncover practical strategies for managing symptoms and challenges. From the subtle impact on sleep…
Tag: chronic illness
Charmayne Andersons Asthma Journey A Personal Account
Charmayne anderson my personal journey with asthma – Charmayne Anderson’s My Personal Journey with Asthma takes readers on a deeply personal exploration of living with this chronic condition. From the initial diagnosis to the daily challenges and triumphs, Charmayne shares her experiences with honesty and vulnerability. This journey is not just about managing symptoms; it’s…
My Familys Asthma Journey A Personal Account
My family s journey with asthma – My family’s journey with asthma sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with personal experiences. We delve into the initial diagnosis, the challenges faced, and the ways we adapted our lives to manage this…
Hyvelle Fergusons Type 2 Diabetes Journey
Hyvelle ferguson my journey with type 2 diabetes – Hyvelle Ferguson’s journey with type 2 diabetes offers a compelling personal account of navigating a chronic condition. This in-depth exploration dives into the challenges and triumphs of managing type 2 diabetes, sharing insights into her experiences and strategies. From understanding the fundamental mechanisms of type 2…
Christina Herreras Diabetes Journey
Christina herrera my journey with type 2 diabetes – Christina Herrera’s journey with type 2 diabetes sets the stage for this enthralling narrative, offering readers a glimpse into a story rich in personal detail and insightful reflections. She shares her experiences, challenges, and triumphs in managing this condition, providing valuable insights and inspiration for others…
Lupus and MS Whats the Difference?
Lupus and ms whats the difference – Lupus and MS: What’s the Difference? These two autoimmune diseases can share similar symptoms, making diagnosis and management challenging. This post delves into the key differences between lupus and multiple sclerosis, exploring their distinct characteristics, diagnostic criteria, treatment approaches, and impact on daily life. We’ll compare symptoms, underlying…
Types of Rheumatoid Arthritis A Deep Dive
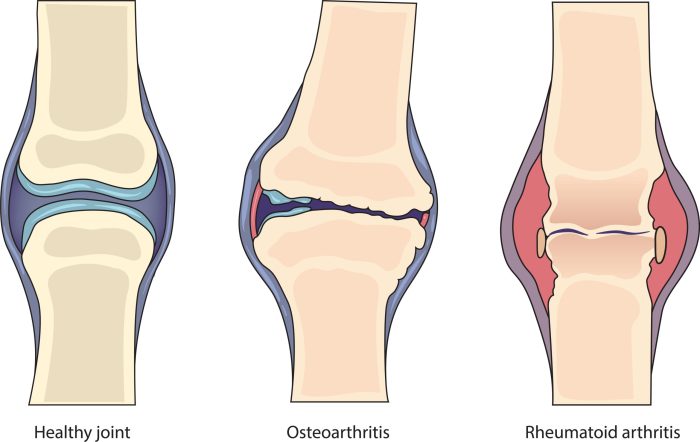
Types of rheumatoid arthritis sets the stage for this enthralling narrative, offering readers a glimpse into the complexities of this chronic autoimmune disease. We’ll explore the various forms of rheumatoid arthritis, examining their unique characteristics, symptoms, and treatment approaches. Understanding the different types is crucial for effective management and a better quality of life. This…
Rheumatoid Arthritis vs Arthritis A Deep Dive
Rheumatoid arthritis vs arthritis: Understanding the differences between these conditions is crucial for effective management and treatment. This comprehensive overview explores the nuances of rheumatoid arthritis (RA), contrasting it with general arthritis, to provide a clearer picture of these often-confused ailments. We’ll delve into their causes, symptoms, diagnostic processes, and treatment options, offering a practical…
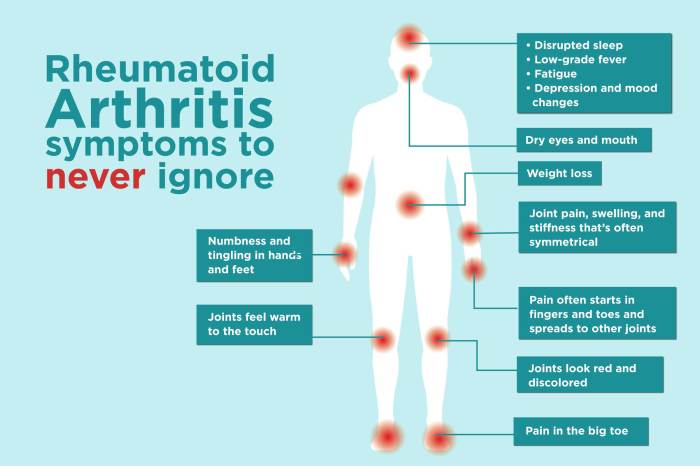
Symptoms of Rheumatoid Arthritis Flares A Deep Dive
Symptoms of rheumatoid arthritis flares sets the stage for this enthralling narrative, offering readers a glimpse into the complexities of this chronic condition. We’ll explore the various symptoms, their progression, and triggers, shedding light on how flares impact daily life. Understanding these nuances is crucial for effective management and improved quality of life. This comprehensive…
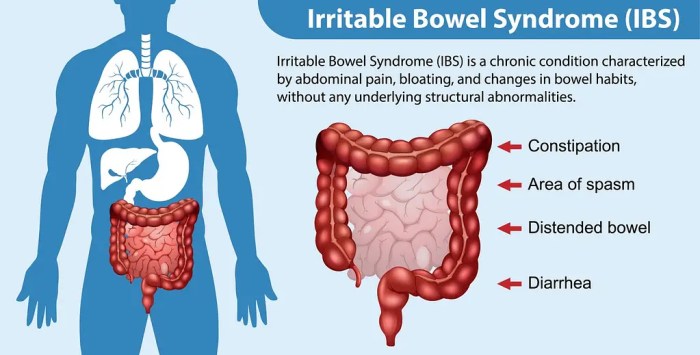
Facts About Irritable Bowel Syndrome A Deep Dive
Facts about irritable bowel syndrome: Understanding this common digestive disorder is crucial for effective management. IBS affects millions worldwide, causing a range of uncomfortable symptoms. This guide delves into the complexities of IBS, exploring its types, potential causes, diagnostic methods, treatment options, and lifestyle modifications. We’ll also discuss coping strategies, potential complications, and the latest…