High cholesterol and stroke risk are serious concerns, but understanding the connection is key to protecting your heart. This guide delves into the complexities of high cholesterol, exploring its impact on the body and its link to stroke. We’ll unpack the different types of cholesterol, the mechanisms behind stroke risk, and the critical role lifestyle…
Tag: cardiovascular health
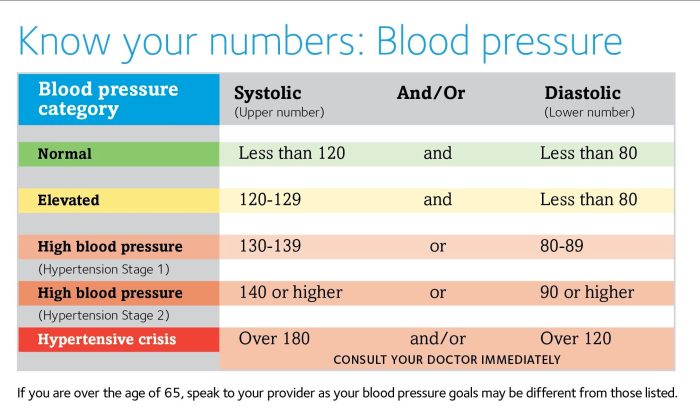
Vitamins to Avoid with Blood Pressure
Vitamins to avoid with blood pressure are crucial for managing hypertension. Certain vitamins, while generally beneficial, can sometimes elevate blood pressure in susceptible individuals. Understanding which vitamins might be problematic, and how to navigate these nuances safely, is key to maintaining cardiovascular health. A balanced diet, coupled with informed decisions about vitamin intake, is essential…
Cholesterol Heart Disease and African Americans A Deep Dive
Cholesterol heart disease and African Americans is a complex issue with significant health disparities. This in-depth look examines the prevalence of high cholesterol, the contributing risk factors, and the impact of socioeconomic and genetic factors on heart disease within this community. We’ll explore the role of lifestyle choices, dietary influences, and cultural contexts, along with…
Normal Blood Pressure Fluctuations Throughout the Day
Normal blood pressure fluctuations throughout the day are a natural part of human physiology. These variations are driven by a complex interplay of internal and external factors, from the simple act of standing to the intricate dance of our autonomic nervous system. Understanding these fluctuations is key to recognizing healthy patterns and identifying potential issues….
Chia Seeds for Heart Disease A Detailed Look
Chia seeds for heart disease offer a fascinating area of exploration, delving into the potential benefits of these tiny seeds for cardiovascular health. Their nutritional profile, rich in fiber and omega-3 fatty acids, suggests a possible role in improving heart health markers. This article investigates the scientific evidence behind this connection, examining how chia seeds…
What Happens to Your Blood Pressure as You Age
What happens to your blood pressure as you age? This is a crucial question for anyone concerned about their health as they get older. Blood pressure regulation is a complex process, and changes in blood vessels and other physiological systems can have a significant impact on your readings throughout life. Understanding these changes, and the…