Portfolio diet heart health is a comprehensive approach to achieving and maintaining cardiovascular well-being. It’s not about strict adherence to one single diet, but rather strategically incorporating diverse dietary patterns to support optimal heart health. This includes understanding different approaches like the Mediterranean or DASH diet, and recognizing the vital role of various nutrients and…
Tag: cardiovascular health
High Blood Pressure and Erectile Dysfunction A Deep Dive
High blood pressure and erectile dysfunction are often linked, and understanding this connection is crucial for proactive health management. This exploration delves into the physiological mechanisms behind this association, examining the prevalence of both conditions and the factors that contribute to their development. We’ll also cover diagnosis, management strategies, potential complications, and ultimately, preventative measures….
Heart Attack in Women Understanding the Differences
Heart attack in women is a critical health issue often misunderstood and under-recognized. Women experience heart attacks differently than men, with symptoms often masked or misconstrued. This detailed look delves into the unique symptoms, risk factors, diagnostic challenges, and treatment options specific to women. Recognizing the variations is crucial for early detection and effective intervention….
Cardiac Effects of Obesity Medications A Deep Dive
Cardiac effects of obesity medications are a crucial area of study, as these drugs can potentially impact the cardiovascular system. This blog post explores the different classes of obesity medications currently available, examining their mechanisms of action and potential physiological pathways through which they might affect the heart. We’ll delve into the potential cardiac risks…
VLDL Understanding Very Low Density Lipoprotein
Very low density lipoprotein vldl – Very low density lipoprotein (VLDL) plays a crucial role in transporting lipids throughout the body. This essential component of lipid metabolism is synthesized in the liver and carries triglycerides to various tissues. Understanding its structure, metabolism, and potential implications for health is vital for anyone interested in maintaining a…
Is Blood Pressure Higher in the Morning? Exploring the Why
Is blood pressure higher in the morning? Yes, it often is, and understanding why this happens is crucial for managing your overall health. Our bodies have a natural rhythm, or circadian rhythm, that influences many functions, including blood pressure. This morning peak in blood pressure isn’t necessarily a cause for alarm, but knowing the factors…
Fish Oil Supplements AFib Risk A Deep Dive
Fish oil supplements AFib risk is a complex issue, with ongoing research attempting to unravel the potential connections between these dietary supplements and the development of Atrial Fibrillation (AFib). This blog post delves into the science behind fish oil’s purported cardiovascular benefits and examines the existing evidence linking fish oil intake to AFib risk. We’ll…
The Benefits of Hawthorn A Comprehensive Guide
The benefits of hawthorn, a versatile plant with a rich history, are now being explored more deeply than ever. From its traditional use in various cultures to modern scientific research, hawthorn’s potential for promoting cardiovascular health and well-being is truly remarkable. This comprehensive guide delves into the different aspects of hawthorn, examining its nutritional profile,…
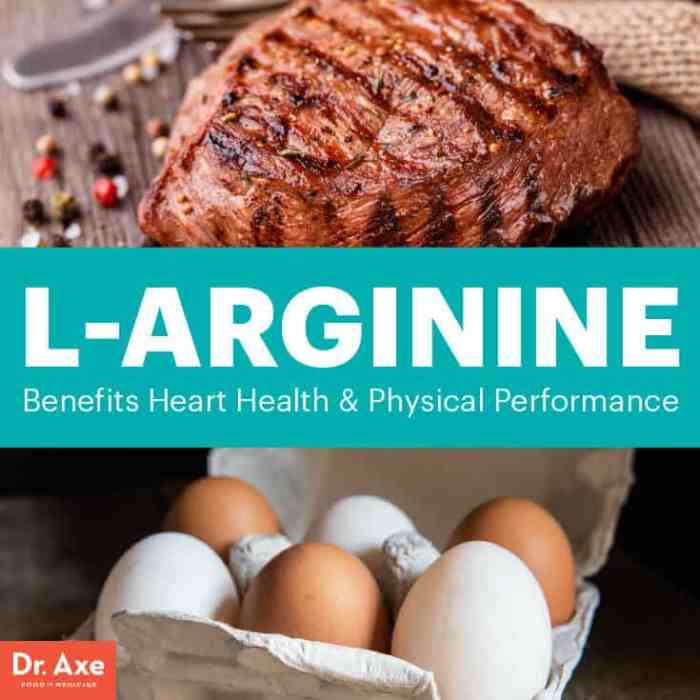
Using L-Arginine for Health A Comprehensive Guide
Using l arginine for health – Using L-arginine for health is a fascinating area of study, exploring how this amino acid can impact various aspects of well-being. From cardiovascular health to exercise performance, and even erectile function, L-arginine’s potential benefits are extensive. This guide delves into the science behind L-arginine, examining its role in the…
The Benefits of Saw Palmetto A Comprehensive Guide
The benefits of saw palmetto, a plant with a rich history of traditional use, are increasingly recognized in modern medicine. This comprehensive guide delves into the potential advantages of saw palmetto, exploring its effects on prostate health, hair growth, cardiovascular function, and even cognitive abilities. We’ll examine the science behind these claims, discuss potential side…