Chemotherapy side effects a2 are a crucial aspect of cancer treatment, and understanding them is vital for both patients and caregivers. This exploration delves into the common, categorized, and managed side effects, examining their impact on quality of life, and even considering potential long-term consequences. We’ll cover everything from the mechanisms behind these effects to…
Tag: cancer treatment
Chemotherapy for Metastatic Breast Cancer A Deep Dive
Is chemotherapy used to treat metastatic breast cancer? This in-depth exploration delves into the role of chemotherapy in managing this aggressive form of breast cancer. We’ll uncover the complexities of metastatic breast cancer, examining its progression from localized disease, and explore the specific chemotherapy regimens employed to combat the spread of cancer cells. Understanding the…
Should I Take Vitamins During Cancer Treatment?
Should I take vitamins during cancer treatment? This crucial question weighs heavily on many facing cancer and their families. The nutritional needs of cancer patients are complex, often significantly altered by the disease and its treatments. This exploration delves into the intricate relationship between vitamins, cancer treatment, and overall well-being, offering a comprehensive overview of…
Treatment of Colon Cancer A Comprehensive Guide
Treatment of colon cancer is a multifaceted journey, demanding a deep understanding of the disease’s stages, diverse treatment approaches, and individualized care plans. This exploration delves into the various strategies, from surgical interventions to innovative therapies, providing a comprehensive overview of the complexities involved. We’ll examine the different types of colon cancer, the diverse range…
Lymph Node Positive Breast Cancer A Comprehensive Guide
Lymph node positive breast cancer presents a significant challenge, but understanding the complexities of this condition is crucial for navigating the journey ahead. This guide delves into the specifics of lymph node involvement, exploring its implications for prognosis, treatment, and ultimately, the patient’s well-being. We’ll uncover the different stages of lymph node involvement, compare it…
De Novo Metastatic Breast Cancer A Deep Dive
De novo metastatic breast cancer presents a unique challenge, representing breast cancer that spreads to other parts of the body from the start, without any prior evidence of local or regional spread. This contrasts with other forms of metastatic breast cancer, and understanding its distinct characteristics, risk factors, diagnostic procedures, and treatment options is crucial…
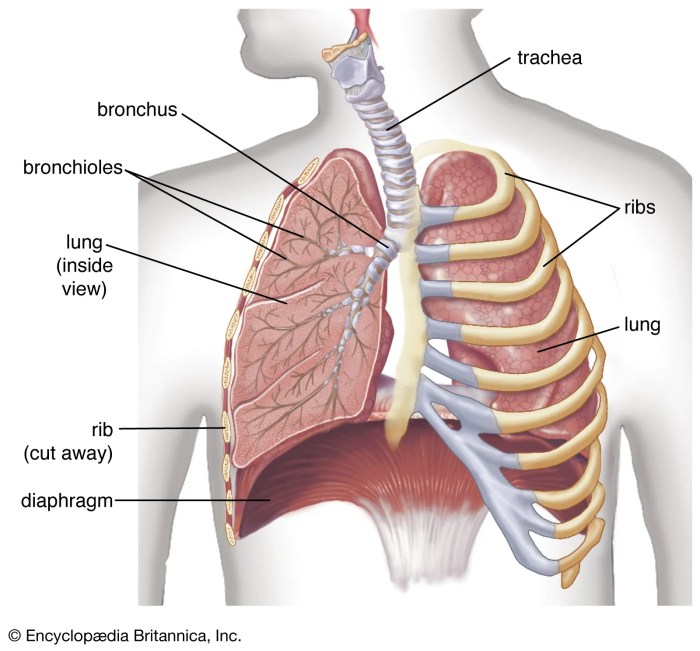
Maintenance Therapy for Lung Cancer A Deep Dive
Maintenance therapy for lung cancer is a crucial aspect of treatment, aiming to prevent the cancer from returning or spreading. It’s a strategy that seeks to keep the cancer at bay after initial treatment, often by targeting specific mechanisms that drive the disease. This in-depth look explores the various types, mechanisms, patient considerations, protocols, side…
Sun Sensitivity During Chemotherapy A Comprehensive Guide
Sun sensitivity during chemotherapy sets the stage for a crucial discussion about managing this common side effect. Understanding the mechanisms behind this sensitivity, recognizing the symptoms, and implementing preventative strategies are all key to navigating this challenging time. This comprehensive guide will cover everything from the science behind sun sensitivity to practical tips for managing…
Breast Cancer Treatment Aging Study A Deep Dive
Breast cancer treatment aging study examines how age impacts the effectiveness and side effects of various therapies. This in-depth exploration considers the diverse factors influencing treatment decisions for patients of different ages, from the available treatment options today to the challenges faced by older adults. It delves into research findings, highlighting the varying responses to…
Lung Cancer with EGFR Mutation A Comprehensive Guide
Lung cancer with an EGFR mutation is a specific type of lung cancer driven by abnormal growth signals. This condition requires a nuanced understanding of the EGFR protein’s role in healthy lung cells, how mutations disrupt this function, and the diverse mutations themselves. Understanding the different types of EGFR mutations, along with their prevalence and…