Lower back pain after sleeping is a common complaint, affecting countless individuals. This detailed exploration delves into the multifaceted causes, from poor sleep posture to underlying medical conditions. We’ll uncover the symptoms, diagnostic processes, and effective treatment options, providing you with actionable strategies for prevention and self-care. Understanding the nuances of this prevalent issue is…
Tag: back pain
When Back Pain Is Serious Understanding the Signs
When back pain is serious, it’s crucial to understand the potential indicators and know when to seek immediate medical attention. This comprehensive guide delves into the various symptoms, underlying conditions, diagnostic procedures, and treatment options associated with serious back pain. We’ll explore the nuances between acute and chronic pain, red flag symptoms, and the importance…
Back Pain A Lung Cancer Symptom
Back pain as a symptom of lung cancer is a complex and often overlooked possibility. While back pain is frequently associated with other conditions, its unusual manifestation in relation to lung cancer warrants careful consideration. This exploration delves into the potential link, highlighting the various ways back pain can manifest, its location, characteristics, and the…
Disc Extrusion, Protrusion, and Sequestration A Deep Dive
Disc extrusion protrusion and sequestration – Disc extrusion, protrusion, and sequestration are common spinal conditions. This comprehensive guide delves into the intricacies of each, from defining the terms to exploring treatment options and long-term outcomes. Understanding the anatomical location, causes, symptoms, and management strategies is crucial for anyone seeking information about these spinal issues. The…
Rheumatoid Arthritis Back Pain Understanding the Impact
Rheumatoid arthritis back pain is a complex condition that significantly impacts a person’s life. It’s not just about aches and stiffness; it’s about understanding the underlying mechanisms, the various symptoms, and the available treatment options. This comprehensive guide delves into the nuances of RA back pain, providing a detailed overview of its causes, diagnosis, and…
Steroid Injections Chronic Back Pain A Deep Dive
Steroid injections chronic back pain are a potential treatment option, but understanding the specifics is crucial. This in-depth look explores the mechanics, efficacy, procedures, patient considerations, and alternatives to help you make informed decisions. We’ll cover everything from the different injection types and their mechanisms of action to the potential risks and long-term management strategies….
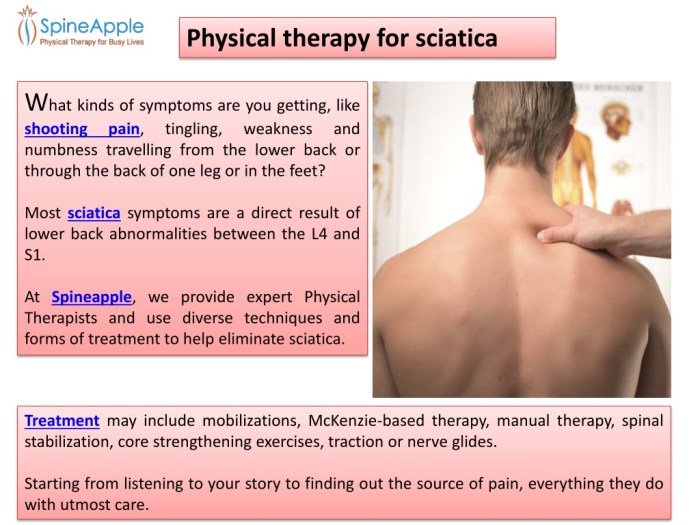
Physical Therapy for Sciatica A Comprehensive Guide
Physical therapy for sciatica offers a powerful approach to managing and relieving this debilitating condition. It delves into understanding the root causes, identifying effective treatments, and empowering patients with self-management strategies. This guide will explore the various techniques and exercises used in physical therapy to alleviate sciatica pain, improve posture, and enhance overall well-being. This…
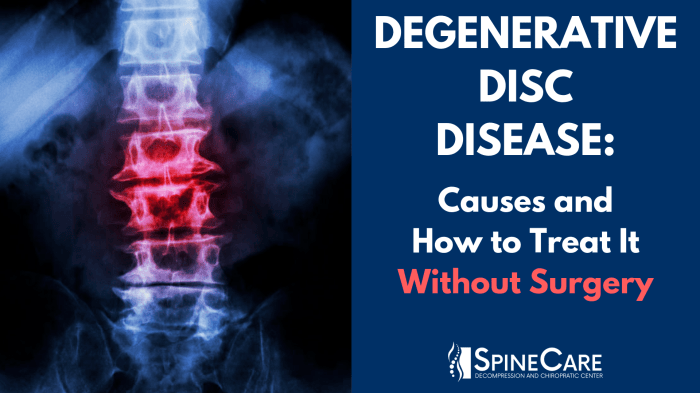
Preventing Degenerative Disc Disease A Guide
Preventing degenerative disc disease is crucial for maintaining a healthy spine and overall well-being. This comprehensive guide explores lifestyle modifications, the importance of spinal health, therapeutic interventions, prevention through early detection, supporting research, and illustrative examples of healthy spinal practices. We’ll delve into dietary recommendations, stress management, exercise plans, posture, and more, empowering you to…
Understanding What is Discogenic Pain
What is discogenic pain? This deep dive explores the complexities of this often-misunderstood back pain, examining its causes, symptoms, diagnosis, and treatment options. We’ll uncover the anatomical structures involved, the differences between types of discogenic pain, and the various approaches to managing this condition. Discogenic pain, originating from the spinal discs, can manifest in a…
What are Herniated Disc Symptoms? A Guide
What are herniated disc symptoms? This comprehensive guide delves into the various ways a herniated disc can manifest, from common pain to more complex complications. Understanding these symptoms is crucial for early diagnosis and effective management. Herniated discs occur when the soft inner material of a spinal disc bulges or ruptures, putting pressure on surrounding…