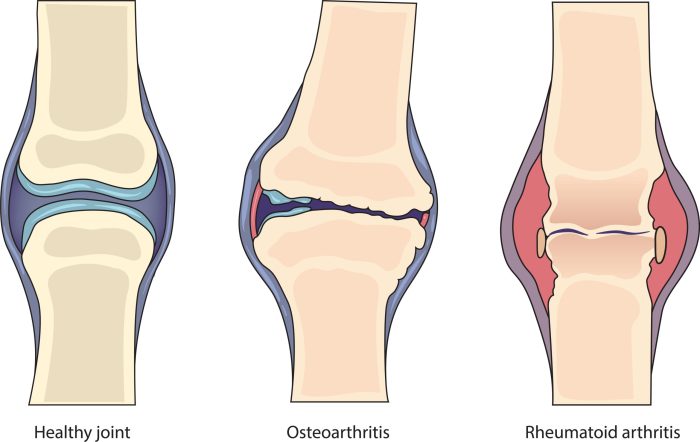
Can arthritis shorten your lifespan? This question delves into the complex relationship between arthritis and overall health. Different types of arthritis, like osteoarthritis and rheumatoid arthritis, impact daily life in various ways, from mobility to overall well-being. Understanding the potential effects on physical function, mental health, and nutrition is crucial in comprehending how arthritis might…
Tag: arthritis
Gout in the Fingers Overview and More
Gout in the fingers overview and more: Understanding this painful condition is crucial for effective management. This in-depth look explores the causes, symptoms, and treatment options for gout in the fingers, distinguishing it from other similar conditions. We’ll also delve into risk factors, prevention strategies, and the practical aspects of living with gout in the…
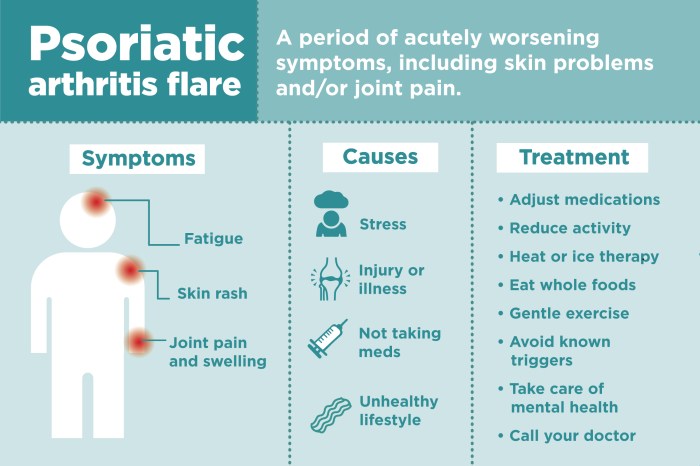
Psoriatic Arthritis Differential Diagnosis Explained
Psoriatic arthritis differential diagnosis is crucial for accurate treatment. Understanding the subtle distinctions between PsA and similar conditions like reactive arthritis, lupus, or even osteoarthritis is key to effective management. This guide dives deep into the various facets of diagnosing PsA, exploring its clinical presentation, potential overlaps with other conditions, and the diagnostic tools used…
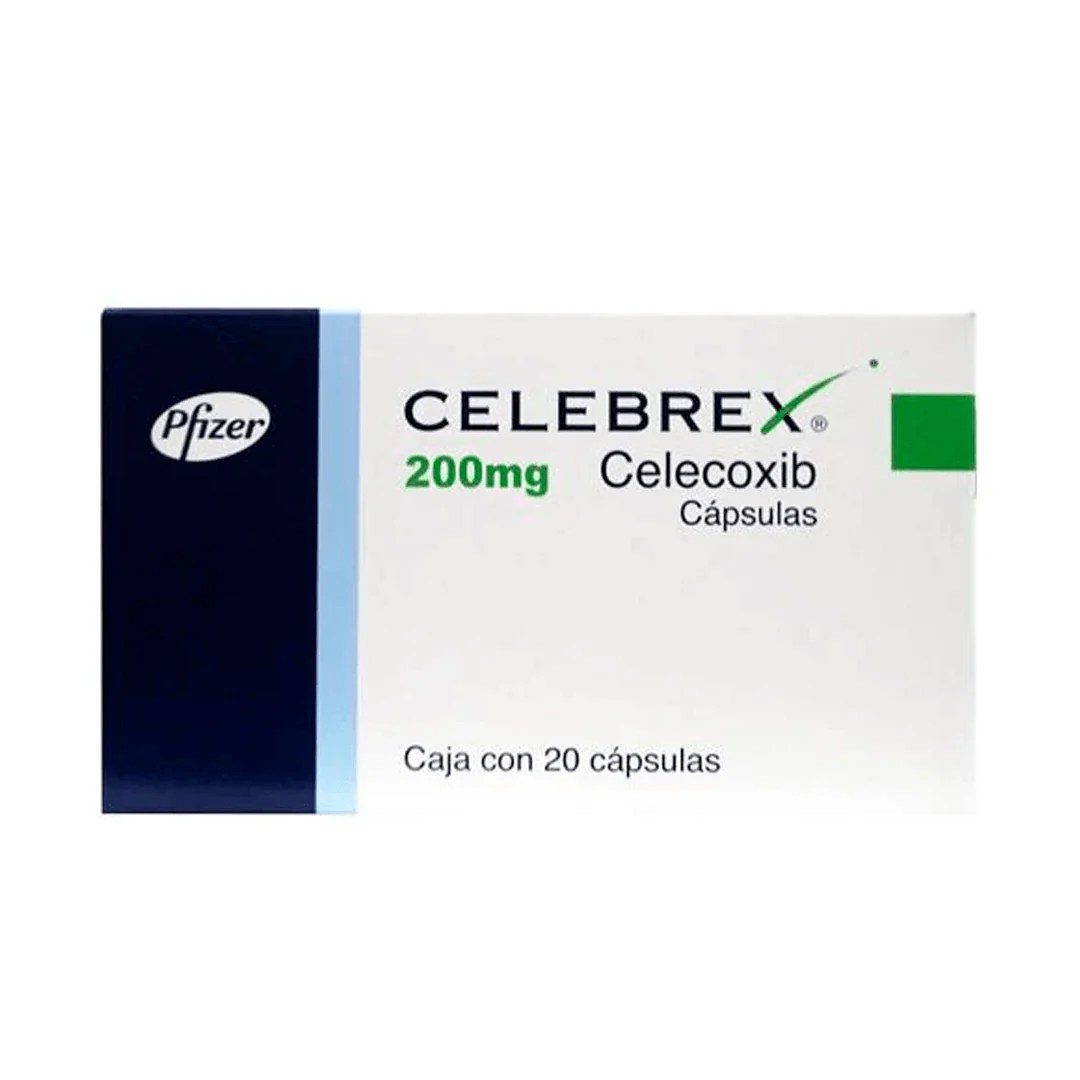
Celebrex vs Ibuprofen Which Pain Reliever?
Celebrex vs ibuprofen how to decide which you should use – Celebrex vs ibuprofen: how to decide which you should use. Choosing between these common pain relievers can be tricky. Both ibuprofen and celecoxib are effective, but they work differently in the body and have varying side effects. This guide will walk you through the…
The Health Benefits of Boswellia A Deep Dive
The health benefits of boswellia, a resinous extract from the Boswellia tree, have captivated herbalists and health enthusiasts for centuries. This ancient remedy, often used in traditional medicine, boasts a range of potential applications, from easing arthritis pain to supporting digestive health. We’ll explore the science behind this intriguing plant, delving into its anti-inflammatory properties,…
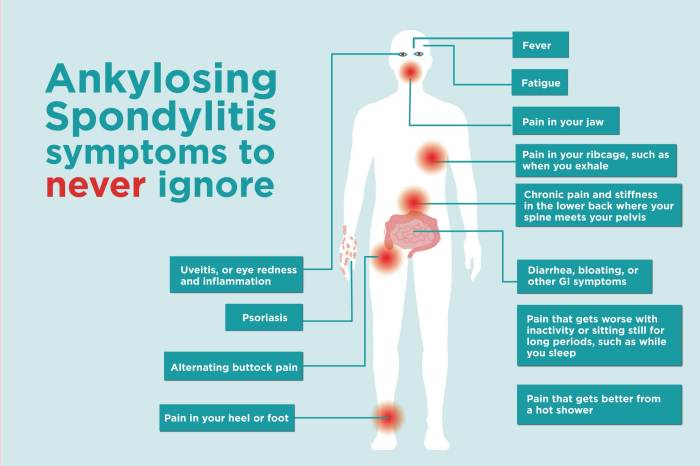
Exercises for Ankylosing Spondylitis A Guide
Exercises for ankylosing spondylitis are crucial for managing this chronic inflammatory condition. This guide delves into the types of exercises, routines, and considerations needed to effectively incorporate movement into your life with AS. We’ll explore everything from personalized programs to lifestyle integration and how exercise impacts your overall well-being. Understanding the specific needs of those…
Collagen for Rheumatoid Arthritis A Deep Dive
Collagen for rheumatoid arthritis: Understanding this potential treatment option requires a deep dive into the complexities of both conditions. Rheumatoid arthritis, a chronic autoimmune disease, attacks the body’s own tissues, particularly the joints. This inflammation can lead to significant pain, stiffness, and decreased mobility. The body’s natural collagen production, crucial for joint health, may be…
Rheumatoid Arthritis vs Arthritis A Deep Dive
Rheumatoid arthritis vs arthritis: Understanding the differences between these conditions is crucial for effective management and treatment. This comprehensive overview explores the nuances of rheumatoid arthritis (RA), contrasting it with general arthritis, to provide a clearer picture of these often-confused ailments. We’ll delve into their causes, symptoms, diagnostic processes, and treatment options, offering a practical…
What Medications Treat Psoriatic Arthritis? A Comprehensive Guide
What medications treat psoriatic arthritis? This comprehensive guide delves into the various treatments available for this complex condition. Psoriatic arthritis, a chronic inflammatory disease, affects not only the joints but also the skin, causing pain, stiffness, and inflammation. Understanding the different medication options and their mechanisms of action is crucial for effective management. We’ll explore…
Ankylosing Spondylitis and Teeth Problems A Deep Dive
Ankylosing spondylitis and teeth problems are intricately linked, creating a complex interplay between spinal health and oral well-being. This exploration delves into the specifics of this connection, examining the common oral health concerns associated with AS, the underlying mechanisms, and effective management strategies. This comprehensive guide will cover various aspects of oral health in individuals…