Suboxone vs methadone how do they differ? This critical comparison delves into the nuances of opioid substitution therapies (OSTs), examining the distinct mechanisms, administration methods, potential side effects, and ultimately, the suitability of each treatment for individual patients. Understanding the differences is key to making informed decisions about managing opioid use disorder.
Opioid substitution therapies, like Suboxone and methadone, play a vital role in treating opioid use disorder. These medications work by providing a safe and controlled alternative to opioids, easing withdrawal symptoms and reducing cravings. While both aim to help individuals overcome addiction, they differ in their composition, how they work in the body, and the potential outcomes.
Introduction to Opioid Substitution Therapies (OSTs)
Opioid Substitution Therapies (OSTs) are crucial interventions for individuals struggling with opioid use disorder (OUD). They offer a safe and medically supervised approach to managing withdrawal symptoms and reducing cravings, enabling patients to focus on recovery. These therapies are not a cure-all, but a critical component of a comprehensive treatment plan.OSTs work by providing a substitute opioid medication, which helps to block the intense cravings and withdrawal symptoms associated with opioid use.
This allows individuals to gradually reduce their dependence on illicit opioids, leading to a more stable and healthier life. Crucially, OSTs are not intended to be a long-term solution on their own. They serve as a bridge to recovery, facilitating access to other therapies and support systems, such as counseling and behavioral treatments, for a more holistic approach to recovery.
General Principles of OSTs
OSTs are based on the principle of gradually replacing the problematic opioid with a medically controlled, safer alternative. This controlled environment allows healthcare professionals to closely monitor patients, manage potential side effects, and adjust dosages as needed. The goal is to mitigate withdrawal symptoms, reduce cravings, and promote a stable physiological state that supports further recovery.
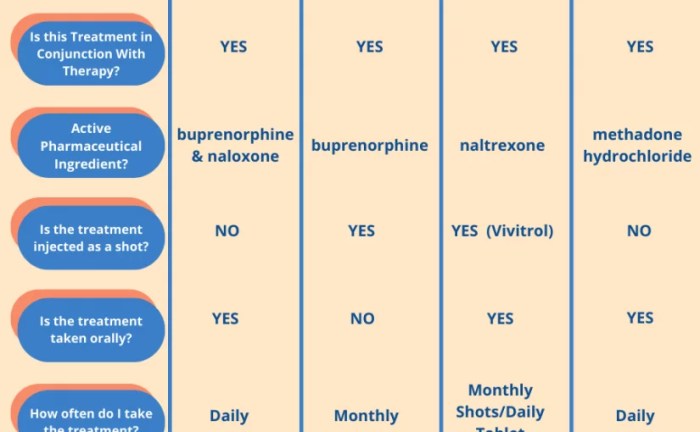
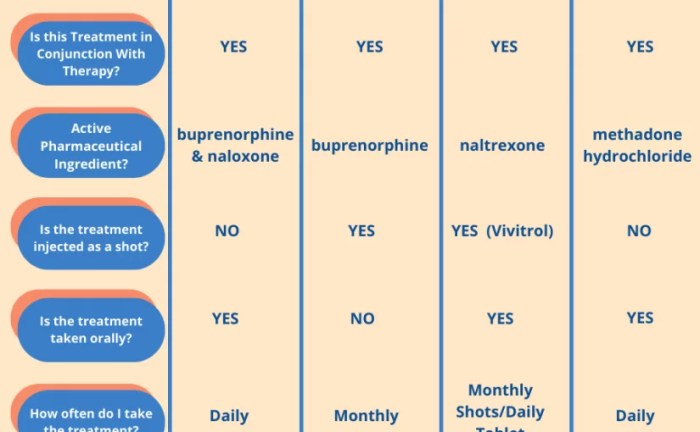
Comparison of OST Approaches
| Characteristic | OSTs in General | Suboxone | Methadone |
|---|---|---|---|
| Mechanism of Action | OSTs work by providing a safe substitute opioid medication to manage withdrawal and cravings. The substitute opioid is often a combination of drugs to reduce the risk of abuse. | Suboxone, a combination of buprenorphine and naloxone, acts as an opioid partial agonist. Buprenorphine binds to opioid receptors, reducing cravings and withdrawal symptoms, while naloxone, an opioid antagonist, prevents misuse by making intravenous injection less rewarding. | Methadone is a full opioid agonist. It binds to opioid receptors, effectively blocking cravings and withdrawal symptoms. Its long-lasting effects require careful monitoring and dosage adjustments. |
| Dosage Administration | Dosage administration is carefully managed and monitored by healthcare professionals to prevent overdose and ensure patient safety. This may involve daily or weekly appointments for medication adjustments. | Suboxone is typically administered orally, often in film or tablet form. The dosage can be adjusted as needed based on patient response and healthcare provider evaluation. | Methadone is generally administered orally. Due to its long-lasting effects and potential for overdose, precise dosage control and close monitoring are crucial. Methadone clinics often use specialized dispensing protocols. |
| Potential Side Effects | Potential side effects include, but are not limited to, nausea, constipation, drowsiness, and respiratory depression. The specific side effects and their severity can vary depending on the individual and the medication. | Potential side effects of Suboxone include nausea, constipation, drowsiness, and headache. Because of naloxone, abuse is less likely. Overdose is less likely with proper dosage and monitoring. | Potential side effects of methadone include nausea, constipation, drowsiness, respiratory depression, and potentially more severe cardiac effects if not carefully monitored. The potential for overdose is greater compared to Suboxone. |
Suboxone (Buprenorphine/Naloxone): Suboxone Vs Methadone How Do They Differ
Suboxone, a combination medication, is a crucial part of opioid substitution therapy (OST). It helps manage opioid use disorder by reducing cravings and withdrawal symptoms. Understanding its components and how it works is vital for anyone considering this treatment option.The unique blend of buprenorphine and naloxone creates a controlled release of medication, supporting sustained recovery. This approach differs from other OSTs and plays a key role in the management of opioid dependence.
Comparing Suboxone and Methadone often comes down to their different mechanisms of action. While both are used to treat opioid use disorder, understanding their distinct approaches is key. For instance, exploring the underlying causes of pulmonary arterial hypertension, a condition sometimes linked to opioid use, can provide context to the nuances in how these medications affect the body.
pulmonary arterial hypertension causes can vary greatly, and this impacts how doctors might prescribe these medications. Ultimately, the best choice between Suboxone and Methadone depends heavily on individual patient needs and circumstances.
Mechanism of Action
Buprenorphine, the primary component of Suboxone, is a partial opioid agonist. This means it activates opioid receptors in the brain, but to a lesser extent than full opioid agonists like heroin or morphine. This controlled activation helps reduce cravings and withdrawal symptoms. Naloxone, an opioid antagonist, is included to deter misuse by intravenous injection. If Suboxone is misused in this manner, the naloxone will trigger a strong unpleasant reaction, making intravenous use significantly less appealing.
How Suboxone Works to Reduce Cravings and Withdrawal Symptoms
Buprenorphine’s partial agonist action helps regulate the brain’s reward system, making the effects of opioids less intense and less rewarding. This dampening of the “high” is a key factor in reducing cravings. Simultaneously, it binds to opioid receptors, preventing the influx of other opioid-related chemicals that would otherwise trigger withdrawal symptoms.
Forms and Routes of Administration
Suboxone comes in various forms, including sublingual tablets, buccal films, and extended-release tablets. The sublingual tablets are placed under the tongue, and the buccal films are placed in the mouth against the cheek. These forms ensure rapid absorption into the bloodstream. Extended-release tablets offer a more consistent level of medication throughout the day, minimizing fluctuations.
Potential Side Effects and Risks
Like any medication, Suboxone has potential side effects. Common side effects may include nausea, constipation, drowsiness, headache, and dizziness. Less common, but potentially serious side effects, include respiratory depression, and allergic reactions. It’s crucial to discuss any concerns or unusual symptoms with a healthcare provider.
Comparison of Suboxone’s Long-Term and Short-Term Effects
Suboxone’s long-term effects are focused on maintaining stability and preventing relapse. In many cases, long-term use leads to reduced cravings, a decreased need for opioids, and a greater sense of well-being. Short-term effects primarily address acute withdrawal symptoms and help stabilize a patient’s physical and mental health. Short-term use often focuses on managing symptoms until a more stable, long-term treatment plan can be implemented.
The long-term use of Suboxone, when administered as prescribed, helps patients develop healthier coping mechanisms and decrease the likelihood of future opioid use. It’s important to note that the specific effects and their duration can vary significantly depending on individual circumstances and responses to the medication.
Methadone
Methadone, another crucial component of Opioid Substitution Therapies (OSTs), is a synthetic opioid used to manage opioid use disorder. It acts on opioid receptors in the brain, but with a significantly longer duration of action compared to other opioids. This extended duration is a key factor in its effectiveness in managing withdrawal symptoms and cravings. Crucially, it helps prevent the severe and potentially life-threatening effects of abrupt opioid cessation.Methadone’s unique mechanism of action makes it a powerful tool in addiction treatment, but its use must be carefully monitored due to its potential side effects.
It’s important to understand how it works, its various forms, and potential risks to ensure responsible and effective treatment.
Mechanism of Action
Methadone’s primary mechanism involves binding to opioid receptors in the brain, similar to other opioids. However, its unique chemical structure allows it to have a longer duration of action compared to other opioids like heroin or morphine. This extended duration is a critical aspect of its efficacy in managing opioid withdrawal and cravings.
“Methadone’s prolonged action helps stabilize brain chemistry and prevent the fluctuating highs and lows associated with opioid use.”
This sustained effect allows for more consistent relief from withdrawal symptoms and a reduction in cravings, which are often a significant obstacle in recovery.
Management of Opioid Withdrawal and Cravings
Methadone effectively manages opioid withdrawal symptoms by mimicking the effects of opioids. This helps to alleviate physical discomfort, such as muscle aches, nausea, and anxiety, associated with withdrawal. Furthermore, it reduces cravings by dampening the intense desire for opioids. This reduction in cravings is crucial for helping individuals maintain abstinence and focus on recovery.
Forms and Routes of Administration
Methadone is available in various forms, each with specific advantages for administration. Oral solution is the most common form, enabling convenient daily dosing. However, other options include oral tablets, and, in specialized settings, intravenous administration may be necessary. The choice of form and route depends on individual needs and preferences, as well as the specific treatment setting.
Potential Side Effects and Risks
Like any medication, methadone comes with potential side effects. These include drowsiness, constipation, nausea, and vomiting. More serious, but less frequent, side effects include respiratory depression, if dosages are not carefully managed. Careful monitoring of vital signs and patient observation are crucial during methadone treatment. Overdose is a significant concern, highlighting the need for close supervision and adherence to prescribed dosages.
Potential Long-Term Consequences and Their Management
Potential long-term consequences of methadone use include dependence. However, with appropriate medical management and patient support, this dependence can be effectively managed. Regular check-ups, consistent medication adherence, and counseling are crucial in mitigating any potential negative consequences. Furthermore, careful monitoring of potential interactions with other medications is essential to prevent complications. Long-term management focuses on minimizing adverse effects while maximizing the therapeutic benefits.
Differences between Suboxone and Methadone
Opioid substitution therapies (OSTs) like Suboxone and Methadone offer crucial support for individuals struggling with opioid use disorder. While both aim to reduce cravings and withdrawal symptoms, they differ significantly in their mechanisms, potential side effects, and the level of supervision required. Understanding these distinctions is vital for informed decision-making in treatment planning.These medications provide a controlled environment for managing opioid dependence, allowing individuals to gradually wean off of illicit opioids and develop healthier coping mechanisms.
Careful consideration of the unique characteristics of each medication is essential for tailoring treatment to individual needs and promoting successful recovery.
Mechanisms of Action
Suboxone and methadone work by occupying opioid receptors in the brain, but they do so in distinct ways. Suboxone, containing buprenorphine and naloxone, acts as a partial opioid agonist at the mu-opioid receptor. This means it activates the receptor to a lesser extent than full agonists like heroin or morphine, thus reducing cravings and withdrawal symptoms. Importantly, naloxone, a potent opioid antagonist, is included to deter misuse by injection, as it causes unpleasant effects if injected.
Methadone, on the other hand, is a full opioid agonist that acts on the mu-opioid receptor, completely blocking the effects of other opioids. It effectively suppresses withdrawal symptoms and reduces cravings by occupying these receptors for an extended period.
Potential Side Effects and Risks
Both Suboxone and methadone carry potential side effects, although their profiles differ. Common side effects of Suboxone include drowsiness, constipation, nausea, and headache. More serious side effects, while less frequent, are possible. Methadone, due to its full agonist nature and longer duration of action, carries a higher risk of respiratory depression and overdose if not properly monitored.
Cardiac complications are also a concern with methadone. It’s crucial to note that individual responses to both medications vary, and careful monitoring is essential throughout treatment.
Dosage Forms, Administration, and Daily Regimens
| Characteristic | Suboxone | Methadone |
|---|---|---|
| Dosage Forms | Film strips, sublingual tablets, and buccal films. | Oral solution, tablets, and liquid. |
| Administration | Sublingual or buccal administration; avoid crushing or chewing. | Oral administration only; avoid crushing or chewing. |
| Daily Regimen | Typically administered once daily, with flexibility based on individual needs. | Requires frequent monitoring and dosage adjustments, often multiple times per day. |
These variations in dosage forms and administration reflect the different ways these medications work in the body and the differing levels of supervision required.
Misuse and Overdose Potential
While both medications can be misused, methadone presents a higher risk of overdose due to its potent effects. Suboxone, due to the presence of naloxone, is less likely to be abused intravenously, although it can still be misused. In both cases, proper monitoring and support are essential to mitigate the risks associated with misuse. Patients are educated about the risks and strategies for preventing overdose.
Levels of Supervision
Methadone treatment typically requires more intensive supervision due to the higher risk of overdose. This includes frequent monitoring of vital signs and close observation of the patient’s response to the medication. Suboxone, while still requiring monitoring, often allows for a less intensive level of supervision, potentially allowing for more autonomy in treatment. However, the level of supervision can vary based on the individual’s needs and the specific treatment program.
Patient Selection and Considerations
Choosing the right opioid substitution therapy (OST) – Suboxone or Methadone – is crucial for successful treatment. It’s not a one-size-fits-all approach. Individual patient needs, preferences, and circumstances play a significant role in determining the most effective and safe treatment path. Factors like the severity of addiction, co-occurring mental health conditions, and past medical history must be carefully evaluated to tailor the treatment plan.Careful consideration of each patient’s unique situation is paramount.
Ever wondered about the differences between Suboxone and Methadone? They’re both used to treat opioid dependence, but their mechanisms differ significantly. While exploring those differences, it’s important to understand how similar conditions, like metastatic castration-resistant prostate cancer symptoms, can significantly impact a patient’s overall health and the effectiveness of these medications. Metastatic castration resistant prostate cancer symptoms often require careful management of pain and other side effects, making the choice between Suboxone and Methadone even more critical.
Ultimately, the best course of action is to discuss these options with a healthcare professional.
This personalized approach maximizes the likelihood of positive outcomes and minimizes potential risks. A thorough assessment, coupled with open communication, is essential to help patients feel comfortable and supported throughout the treatment process.
Patient History
Patient history provides valuable insights into potential treatment responses and risks. Understanding past medical conditions, substance use patterns, and mental health diagnoses is crucial. For example, a patient with a history of liver disease might be a less suitable candidate for methadone, which can further stress the liver. Similarly, a patient with a history of respiratory issues may require more careful monitoring when starting Suboxone.
While researching Suboxone vs. Methadone, I stumbled upon some fascinating insights into natural remedies for ADHD. Exploring different approaches to managing these conditions can be really helpful, and finding what works best for you is key. For example, natural remedies like certain dietary changes and supplements could offer potential benefits for managing ADHD symptoms. This exploration into alternative treatments is a great reminder that when comparing Suboxone and Methadone, it’s important to consider a holistic approach to your well-being, and not just rely on pharmaceutical options.
Understanding the nuances of these opioid-replacement therapies remains crucial for informed decision-making. natural remedies for adhd
The nuances of past experiences influence the selection of the appropriate treatment.
Severity of Addiction
The severity of the opioid addiction significantly impacts treatment choice. Patients with milder addiction may respond well to Suboxone, which offers a lower risk of overdose compared to methadone. Methadone, with its higher potential for dependence, is often considered for more severe cases, where a higher dose may be necessary to effectively manage withdrawal symptoms and cravings.
Co-occurring Disorders
Co-occurring disorders, such as depression, anxiety, or other mental health conditions, often accompany opioid use disorders. These conditions require careful consideration when selecting a treatment. For instance, a patient with severe anxiety might experience greater side effects with methadone due to its sedative properties. Conversely, Suboxone might be a better option if anxiety is a significant concern.
Patient Counseling and Support
Effective patient counseling and support are indispensable components of OST. This includes comprehensive information about both Suboxone and Methadone, along with ongoing guidance and encouragement. Regular check-ups, support groups, and individual therapy sessions help patients navigate the challenges of recovery and maintain their commitment to treatment. Emphasizing the importance of self-care and healthy coping mechanisms empowers patients to effectively manage their treatment and achieve lasting recovery.
Factors Influencing Patient Choice, Suboxone vs methadone how do they differ
| Factor | Suboxone Considerations | Methadone Considerations |
|---|---|---|
| Patient History | Consider previous medical conditions, substance use patterns, and mental health diagnoses. A patient with a history of liver disease might be a less suitable candidate for methadone. | Evaluate past medical history, including liver and respiratory conditions. Patients with pre-existing conditions may require more careful monitoring. |
| Severity of Addiction | Generally suitable for milder to moderate cases. Lower risk of overdose compared to methadone. | Often preferred for more severe cases requiring higher doses for effective withdrawal management. |
| Co-occurring Disorders | May be a better option for patients with significant anxiety or other mental health concerns due to its lower sedative properties. | Potential for increased sedative effects, which could exacerbate existing anxiety or other co-occurring disorders. |
| Patient Preferences | Generally a lower barrier to entry in terms of daily administration. | Requires daily dosing at a clinic due to its potential for abuse. |
| Access to Care | Often available at more locations than methadone clinics. | Typically administered in designated clinics. |
Treatment Outcomes and Monitoring
Opioid substitution therapies (OSTs), like Suboxone and methadone, aim to help individuals manage opioid use disorder (OUD) effectively. Successful treatment hinges on careful monitoring and tailored support. This section will explore expected outcomes, progress monitoring methods, and the importance of ongoing support in achieving sustained recovery.Understanding the specific outcomes and monitoring parameters for each therapy is crucial for optimizing patient care.
Different patients will respond to treatment in unique ways, and a dynamic approach to monitoring is essential.
Expected Outcomes of Suboxone Treatment
Suboxone, containing buprenorphine and naloxone, is designed to reduce opioid cravings and withdrawal symptoms. Patients typically experience a decrease in opioid use, improved mood, and an increased ability to engage in daily activities. Many individuals report improved overall well-being and a greater sense of stability in their lives. Successful outcomes often manifest as reduced instances of relapse and improved relationships with support systems.
Some individuals may experience a significant reduction in opioid-related health problems.
Expected Outcomes of Methadone Treatment
Methadone, a full opioid agonist, acts as a substitute for the abused opioid. Its primary role is to reduce withdrawal symptoms and cravings. Successful methadone treatment often results in a reduction in opioid use and related problems, like overdose risk and criminal activity. Patients may experience improved physical health, enhanced social functioning, and a higher level of engagement in their recovery journey.
Successful outcomes are often measured by a decrease in opioid use, decreased criminal activity, and improved quality of life indicators.
Methods of Monitoring Patient Progress
Monitoring patient progress involves a multi-faceted approach. Regular assessments of vital signs, mood, and cravings are essential. Assessing treatment adherence and exploring potential side effects or complications are key components. Therapists often employ structured interviews and questionnaires to gauge progress. Self-reporting tools and observed behavior provide valuable insights into the effectiveness of the treatment.
Frequent follow-up appointments allow for adjustments to the treatment plan, ensuring the therapy remains relevant to the patient’s evolving needs.
Examples of Successful Treatment Outcomes
Numerous success stories highlight the effectiveness of OSTs. One individual, struggling with heroin addiction for years, found stability through methadone treatment. The treatment helped him reduce his drug use and eventually, he became more involved in his community and family life. Similarly, a patient using Suboxone reported a marked improvement in mental health and stability. These are just a few examples; countless individuals have benefited from these therapies.
Importance of Ongoing Monitoring and Support
Ongoing monitoring and support are critical to long-term recovery. Relapse is possible, and early detection of any signs of relapse is crucial for immediate intervention. A supportive environment that fosters a sense of community is essential. Continued access to counseling, support groups, and medical professionals provides crucial resources to maintain sobriety. Maintaining contact with healthcare providers is key for navigating challenges and ensuring the treatment remains effective.
Monitoring Parameters for Both Treatments
| Monitoring Parameter | Suboxone | Methadone |
|---|---|---|
| Compliance | Regular pill counts, adherence to scheduled appointments, and self-reported usage. | Consistent attendance at appointments, regular drug testing, and monitoring of prescribed dosage. |
| Adverse Effects | Monitor for sedation, dizziness, nausea, constipation, and other potential side effects. | Regular monitoring for respiratory depression, sedation, nausea, constipation, and other potential side effects. |
| Withdrawal Symptoms | Closely monitor for signs of opioid withdrawal, including anxiety, irritability, and muscle aches. | Closely monitor for signs of opioid withdrawal, including anxiety, irritability, and muscle aches. |
| Mood and Mental Health | Regular assessments of mood, depression, anxiety, and other mental health concerns. | Regular assessments of mood, depression, anxiety, and other mental health concerns. |
| Physical Health | Monitor for any physical complications, including liver or kidney issues. | Monitor for any physical complications, including liver or kidney issues. |
Conclusive Thoughts
In conclusion, both Suboxone and methadone offer viable pathways for managing opioid use disorder, but their distinct characteristics make them better suited for different individuals. Careful consideration of a patient’s medical history, the severity of their addiction, and co-occurring disorders is crucial in determining the most appropriate treatment. Ongoing monitoring and support are essential for successful outcomes in either treatment.
Ultimately, a personalized approach tailored to the specific needs of each patient is paramount for optimal results.