Responding to confabulation in dementia is a crucial aspect of caregiving. This guide dives deep into understanding confabulation in dementia, from its definition and triggers to effective response strategies and communication techniques. We’ll explore how to identify confabulation, differentiate it from other cognitive impairments, and create supportive environments to help manage these episodes.
This comprehensive guide covers various facets of confabulation in dementia, from identifying potential triggers and factors to effective communication strategies and environmental modifications. It emphasizes the importance of validating the individual’s feelings and experiences, and provides practical tools for caregivers and healthcare professionals.
Defining Confabulation in Dementia
Confabulation, a common symptom in various neurological conditions, including dementia, presents as the production of fabricated, or distorted, memories. It’s not simply lying, but rather a genuine, albeit inaccurate, recollection of events. Crucially, this symptom is a manifestation of underlying cognitive impairment, not an intentional attempt to deceive. Understanding confabulation is vital for accurate diagnosis and effective care of individuals experiencing dementia.Confabulation in dementia is characterized by the involuntary creation of false memories, often vivid and detailed.
Dealing with confabulation in dementia can be tricky, but sometimes a simple change of environment can make a huge difference. For example, like how adjusting your home for allergic asthma can significantly improve quality of life for sufferers, changes to make at home with allergic asthma can also be beneficial. These changes, from removing allergens to controlling humidity, can surprisingly have a positive impact on managing the symptoms and ultimately helping those with dementia feel more comfortable and secure in their own space, which can help in addressing the confabulation itself.
This phenomenon stems from a breakdown in the brain’s ability to distinguish between real and imagined experiences, a direct consequence of the progressive nature of the disease. The false memories often serve as a compensatory mechanism, an attempt to fill in gaps in the individual’s memory.
Defining Confabulation in Dementia
Confabulation in dementia is the production of fabricated, or distorted, memories. It’s characterized by the involuntary creation of false memories, often vivid and detailed, in response to memory gaps. This isn’t deliberate lying but a genuine, though inaccurate, recollection of events, arising from impaired cognitive function.
Types of Confabulation in Dementia
Confabulation in dementia can manifest in various forms, reflecting the underlying cognitive impairments.
- Memory-Based Confabulation: This type is driven by a need to fill gaps in memory. An individual might create a narrative to account for a forgotten event, or invent a complete episode. For example, a person with dementia might vividly recount a visit to a friend’s house, when in fact they never visited.
- Suggestibility-Based Confabulation: This occurs when an individual’s memories are influenced by external cues or suggestions. A question, a conversation, or even a visual stimulus can trigger the fabrication of a memory. Imagine a caregiver suggesting a specific event happened, and the individual then “remembers” it with remarkable detail.
- Emotional-Motivational Confabulation: In this case, the fabricated memory might serve a psychological function, such as alleviating anxiety or enhancing self-esteem. A person might recount a successful career accomplishment that never actually occurred, bolstering their sense of self-worth in the face of declining abilities.
Cognitive Mechanisms Underlying Confabulation
Several cognitive mechanisms contribute to confabulation in dementia. These impairments affect the brain’s ability to accurately process and retrieve information.
- Impaired Source Monitoring: The inability to distinguish the origin of a memory—where, when, and how it was acquired—is a key factor. This is fundamental to understanding how the individual struggles to differentiate between real and imagined experiences.
- Executive Dysfunction: Dementia often affects the brain’s ability to plan, organize, and regulate thoughts and behaviors. This disruption can lead to a breakdown in the individual’s ability to critically evaluate their own memories.
- Hippocampal Damage: The hippocampus plays a crucial role in memory formation and consolidation. Damage to this area, a common occurrence in dementia, can disrupt the ability to distinguish real from false memories.
Comparison of Confabulation with Other Memory-Related Impairments
| Feature | Confabulation | Amnesia ||——————-|—————————————————————————-|——————————————————————————|| Definition | Production of fabricated or distorted memories.
| Inability to recall past experiences. || Mechanism | Impaired source monitoring, executive dysfunction, hippocampal damage.
| Damage to memory encoding and retrieval mechanisms. || Content | Often vivid and detailed, can serve a psychological function.
| May involve gaps or total loss of memories. || Intentionality | Not intentional; individual believes the memory is real.
| Not intentional; individual is unaware of the memory deficit. |
Identifying Triggers and Factors: Responding To Confabulation In Dementia
Unraveling the complexities of confabulation in dementia often involves understanding the circumstances that precede these episodes. While the underlying neurological changes are significant, environmental and internal factors can act as triggers, influencing the frequency and nature of confabulatory events. Understanding these triggers is crucial for caregivers and clinicians to provide better support and strategies for managing these episodes.Confabulation isn’t simply a random occurrence; it’s a response to internal and external stimuli.
Identifying the triggers can lead to proactive strategies to minimize confabulatory episodes and create a more supportive environment for individuals living with dementia. By recognizing patterns and associations, we can better understand the motivations behind these seemingly fabricated memories.
Potential Triggers of Confabulatory Episodes
Confabulatory episodes aren’t always linked to a single, identifiable cause. Often, a combination of factors contributes to the manifestation of these events. These factors can include both internal physiological states and external environmental influences.
Dealing with confabulation in dementia can be tricky, but understanding the underlying reasons is key. Sometimes, these fabricated memories are linked to other health issues, like the complex relationship between diabetes and blood pressure. For instance, a better understanding of does diabetes cause high blood pressure might help us better interpret the patient’s narrative.
Ultimately, a compassionate and patient approach is vital when responding to these situations, focusing on validating the person’s feelings rather than correcting the confabulations.
- Stress: High levels of stress, whether emotional or physical, can significantly increase the likelihood of confabulation. Stress hormones can affect cognitive function, making it more difficult for the individual to distinguish between reality and imagined events. Examples include stressful interactions with caregivers, unexpected changes in routines, or even minor anxieties. For example, a resident in a care facility might confabulate more frequently when facing a new staff member or a change in their meal schedule.
- Medication Side Effects: Certain medications used to treat dementia or other conditions can have side effects that affect cognitive processes. These effects can include disorientation, confusion, and memory problems, potentially leading to confabulation. It’s crucial to assess the possible influence of medications when confabulatory episodes arise. A specific example would be a patient on a medication known to induce confusion reporting an event that never happened, attributed to the medication.
- Sleep Deprivation: Adequate sleep is essential for cognitive function. Sleep deprivation can impair memory consolidation and processing, increasing the likelihood of confabulatory episodes. The brain’s ability to accurately recall and differentiate information is affected when sleep is insufficient. An example would be a patient experiencing sleeplessness due to pain or discomfort, and subsequently confabulating about events that did not occur during their sleeplessness.
- Sensory Deprivation: Limited sensory input can lead to confabulation. A lack of stimulation, whether visual, auditory, or tactile, can increase the individual’s reliance on internal imagery and potentially lead to confabulation. For instance, a patient with limited visual stimulation might confabulate about a visit from a relative they have not seen in months, due to their need for sensory stimulation.
Situations Frequently Associated with Confabulation
Specific situations and contexts can often trigger confabulatory episodes. Understanding these situations is helpful in mitigating the frequency and impact of these episodes.
- Changes in Routine: Significant alterations in daily routines can cause disorientation and confusion, which can manifest as confabulation. For example, a patient who is accustomed to a set schedule might confabulate about activities that were not part of their usual routine, but which were associated with a period of disruption.
- Social Interactions: During conversations or interactions, especially if there’s a change in personnel or new individuals, confusion and confabulation can arise. For example, a patient might confabulate about conversations with someone they have not met before.
- Ambiguous or Unclear Environments: A lack of clarity or visual cues in a new or unfamiliar environment can lead to confabulation. For example, a patient visiting a different part of the care facility might report events from a different location, creating a confabulation.
Correlation Between Triggers and Frequency
The following table provides a hypothetical representation of the correlation between specific triggers and the frequency of confabulatory episodes. This is a generalized example and individual experiences may vary greatly.
| Trigger | Frequency of Confabulatory Episodes (Hypothetical) |
|---|---|
| Stress (High) | High |
| Medication Side Effects (Significant) | Moderate to High |
| Sleep Deprivation (Chronic) | Moderate |
| Sensory Deprivation (Prolonged) | Low to Moderate |
| Changes in Routine | Moderate |
Assessing and Diagnosing Confabulation
Unraveling the complexities of confabulation in dementia requires a multifaceted approach. Simply put, confabulation is not a straightforward diagnosis. It’s crucial to differentiate it from other cognitive impairments that might present with similar symptoms. This necessitates a comprehensive evaluation process that goes beyond relying solely on reported accounts. A careful investigation into the individual’s background, medical history, and current cognitive status is essential.The process of diagnosing confabulation in dementia is nuanced and requires a blend of observation, testing, and careful consideration of the patient’s individual circumstances.
A thorough understanding of the underlying cognitive deficits and potential contributing factors is paramount to avoid misdiagnosis. This nuanced approach ensures that the individual receives appropriate support and interventions tailored to their specific needs.
Methods Employed to Detect Confabulation
A multi-pronged approach is vital to accurately identify and assess confabulation. This involves not only observing the individual’s behaviour but also utilizing standardized cognitive assessments. Direct questioning, observation of inconsistencies in narratives, and evaluation of memory performance are crucial components of this assessment.
Assessment Tools and Techniques, Responding to confabulation in dementia
Various assessment tools and techniques are employed to detect confabulation. These tools range from structured interviews to neuropsychological testing. Examples include:
- Detailed Interviews: These interviews delve into the individual’s reported experiences, focusing on potential inconsistencies and gaps in their narratives. Careful attention is paid to the individual’s emotional state and any signs of distress or agitation during the questioning process. A skilled interviewer will note any unusual embellishments or fantastical details, and assess the individual’s confidence level in their accounts.
- Neuropsychological Testing: These tests evaluate various cognitive functions, including memory, attention, and executive function. Discrepancies between reported events and the results of these tests can be indicators of confabulation. For example, a patient might consistently claim to have performed actions that are contradicted by the results of memory tests, such as a test showing significant deficits in their ability to recall recent events.
Further investigation into the nature and extent of the cognitive impairments is essential.
- Behavioral Observation: Close observation of the individual’s behaviour in different settings provides valuable insights. Inconsistencies between verbal accounts and observed actions, or repetitive confabulatory narratives, are significant indicators of the condition. For example, if a patient repeatedly claims to have performed tasks they clearly did not, such as having a conversation with a prominent figure when they have no memory of the occasion, this would trigger further investigation.
Differentiating Confabulation from Other Cognitive Impairments
Distinguishing confabulation from other cognitive impairments is crucial for accurate diagnosis. Conditions like delirium, depression, and other forms of memory loss can exhibit overlapping symptoms. It is essential to rule out these other potential causes before confirming a diagnosis of confabulation.
Structured Approach for Evaluating Confabulation
A structured approach is necessary for accurate evaluation. This approach involves a systematic process encompassing the following steps:
- Comprehensive Medical History: Gathering a detailed medical history, including the patient’s prior health conditions and any current medications, helps identify potential contributing factors to confabulation. For instance, a recent stroke or head injury could be contributing to the symptoms.
- Neurological Examination: A neurological examination assesses the patient’s motor skills, reflexes, and sensory functions. This helps identify potential neurological causes that could be affecting the cognitive functions.
- Cognitive Assessment: Standardized cognitive tests evaluate memory, attention, language, and other cognitive functions. Discrepancies in performance can point to confabulation.
- Behavioral Observation: Carefully observing the patient’s behaviour in different situations can uncover inconsistencies between their reported accounts and observed actions. This approach is particularly useful in identifying patterns of confabulation.
Strategies for Responding to Confabulation
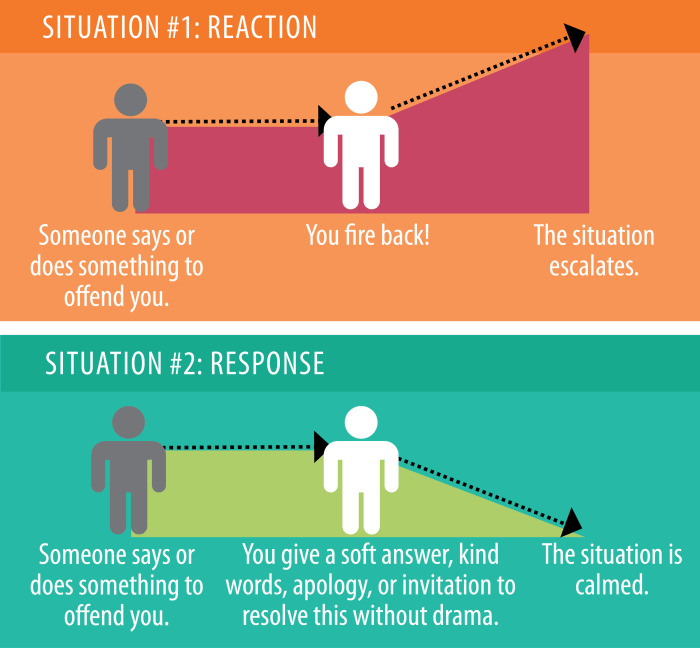
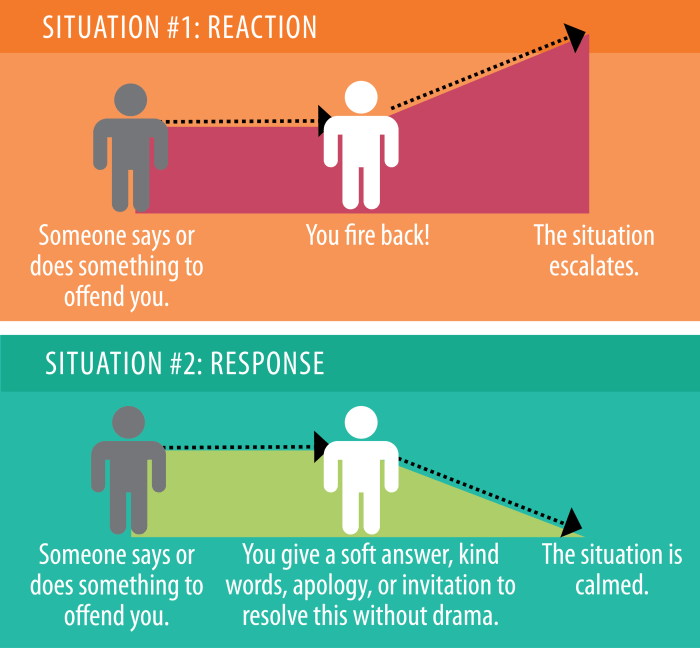
Navigating confabulation in dementia requires a delicate balance of understanding and support. It’s crucial to remember that confabulatory statements are not intentional lies, but rather a symptom of the disease process. This means caregivers and healthcare professionals need to adopt strategies that prioritize the individual’s well-being and dignity while managing the challenging nature of these episodes.
Understanding the Individual’s Perspective
Effective responses to confabulation hinge on a deep understanding of the individual’s experiences and the context surrounding their confabulatory statements. This includes recognizing that the individual is not deliberately trying to deceive, but is struggling with memory and reality processing. Rather than challenging their account, try to understand the underlying needs and emotions that may be driving the confabulation.
For example, if someone repeatedly describes a visit from a long-deceased relative, it might reflect a desire for connection with that person. Understanding these emotional underpinnings allows for a more compassionate and effective response.
Responding Constructively to Confabulatory Statements
Instead of directly contradicting confabulatory statements, which can be disorienting and upsetting, focus on gently redirecting the conversation. For example, if someone claims to have gone to the grocery store, instead of saying “You didn’t go to the grocery store,” you could say, “Tell me about the things you enjoy buying at the grocery store.” This approach acknowledges the individual’s perspective while gently steering the conversation toward more grounded and relatable topics.
Validating Feelings and Experiences
Acknowledging and validating the individual’s feelings and experiences is paramount. Confabulation often arises from unmet emotional needs. If someone is distressed about a missing item, instead of focusing on the reality of the situation, acknowledge their concern. For example, “I understand you’re feeling worried about the missing item. Let’s find a way to help you feel more secure.” This validation process helps create a supportive environment and reduces the individual’s distress.
Strategies for Managing Confabulatory Episodes
- Focus on the present: Shifting the focus to the present moment can help redirect attention away from confabulatory statements. Engage the individual in activities like listening to music, playing games, or having a conversation about the current time.
- Use visual aids and reminders: Visual aids, such as photos or calendars, can provide concrete reminders and help ground the individual in reality. They can be particularly helpful in stimulating memories associated with familiar faces or places.
- Maintain a consistent routine: A structured daily routine can provide a sense of stability and predictability, reducing anxiety and potentially lessening confabulatory episodes. This predictability is crucial for individuals with dementia.
- Create a safe and supportive environment: A calm and supportive environment can be incredibly helpful in managing confabulatory episodes. Reduce distractions and ensure the individual feels secure and understood.
Response Styles and Impact
| Response Style | Potential Impact on Individual |
|---|---|
| Direct contradiction | Confusion, frustration, increased anxiety, feelings of being invalidated. |
| Ignoring the statement | Feeling unheard, diminished sense of importance, possible escalation of confabulation. |
| Gentle redirection | Sense of being understood, reduced frustration, possibility of grounding in reality. |
| Validation of feelings | Sense of security, reduced anxiety, increased comfort and cooperation. |
Communication Techniques for Caregivers
Navigating the complexities of dementia, especially when confabulation arises, requires a delicate balance of understanding and empathy. Caregivers often find themselves in a challenging position, needing to respond to fabricated stories without dismissing the person’s feelings or reality. Effective communication strategies can help foster a more positive and supportive environment for both the individual and the caregiver.Confabulation, while frustrating for caregivers, is a symptom of the underlying cognitive decline.
Addressing it directly can sometimes worsen the situation, leading to emotional distress or confusion. Instead, a focus on validation and understanding is key. Effective communication is a crucial tool to maintain connection and respect.
Empathetic Responses to Confabulatory Statements
Understanding the emotional needs behind confabulation is essential. Confabulatory statements are often driven by a need to fill in gaps in memory or maintain a sense of self. An empathetic response acknowledges these needs without validating the factual inaccuracies.
- Instead of: “That’s not true, you were never in Paris.” Try: “I understand you have a strong memory of being in Paris. Tell me more about that trip. What was it like?”
- Instead of: “You’re mistaken, we haven’t seen that movie.” Try: “It sounds like you’re very excited about this movie. What aspects of it are you most looking forward to?”
- Instead of: “No, you don’t live with your parents anymore.” Try: “It’s lovely that you have such warm memories of living with your parents. What was your favourite part of that time?”
These examples illustrate a shift from direct correction to open-ended questioning, which invites the person to elaborate and connect with their feelings about the situation. The focus remains on understanding their perspective rather than challenging their fabricated account.
Reframing Conversations During Confabulation
Direct confrontation can be counterproductive. Instead of arguing or correcting, gently redirect the conversation to a more familiar or comforting topic. This approach allows the individual to feel heard and understood, while also keeping the interaction positive.
- If the person recounts a visit to the Grand Canyon, try: “Remember that wonderful trip we took to the beach last summer? Tell me about the beautiful colours of the sand.”
- If the person insists on a specific task they have to complete, ask: “How can we make sure you have everything you need to feel comfortable and safe today?”
- If the person talks about a specific event from the past, suggest: “You seem very happy recalling that memory. Let’s talk about some of your favourite hobbies.”
These examples highlight how reframing the conversation can help to shift the focus from the inaccurate detail to a more positive and relevant topic. This can help maintain a sense of connection and respect.
Addressing the Issue Without Confrontation
Maintaining a calm and reassuring demeanor is crucial. Avoid arguing or correcting the person. Acknowledge their feelings and experiences, even if they are inaccurate.
- Use gentle reminders or cues that focus on positive and familiar experiences. For example, “It’s so nice to see you smiling; you always enjoyed gardening, perhaps we could take a look at your favourite plants today.”
- Maintain a calm and reassuring tone, showing that you are present and engaged with the person’s feelings.
- Validate their feelings and emotions, even if the content of their statements is inaccurate. “I understand you feel very strongly about this.”
Environmental Modifications
Creating a supportive and predictable environment is crucial for managing confabulation in dementia. A well-structured environment can reduce stress and anxiety, both of which can trigger confabulatory episodes. Understanding how the environment affects cognitive function and memory is key to tailoring a space that promotes well-being and reduces the need for confabulation as a coping mechanism.The impact of the environment on a person with dementia is multifaceted.
A chaotic or unfamiliar environment can heighten confusion and lead to confabulation. Conversely, a structured and familiar space can provide a sense of security and reduce the likelihood of these episodes. The goal is to minimize sensory overload and maximize the use of familiar cues to aid memory and recognition.
Creating a Supportive and Stimulating Environment
Familiar surroundings play a vital role in mitigating confabulatory episodes. Visual reminders, such as photos of loved ones, familiar landmarks, or personal belongings, can provide a sense of comfort and continuity. This allows individuals to connect with their past and present, reducing the need to fabricate memories. The use of personal items can also trigger positive emotions, creating a more pleasant and secure atmosphere.
Environmental Cues and Memory Aids
Implementing visual and auditory cues can be highly effective. A calendar with large, clear dates and a daily schedule can help individuals track time and events. Using clocks with large numbers and clear displays of the time can minimize confusion. Familiar sounds, like calming music or recordings of loved ones’ voices, can also trigger positive associations and reduce anxiety.
Minimizing Sensory Overload
A key aspect of environmental modification is reducing sensory overload. Loud noises, flashing lights, and excessive visual stimulation can be overwhelming for individuals with dementia. A quiet and calming atmosphere, with muted colors and soft lighting, can be significantly beneficial. This allows for clearer focus and reduced confusion.
Utilizing Spatial Organization
Organizing spaces with clear pathways and minimal clutter is important. Using color-coded systems for different areas (e.g., red for kitchen, blue for bathroom) can help individuals navigate their surroundings more easily. This predictability reduces confusion and frustration, which can contribute to confabulation.
Table Summarizing Environmental Factors
| Environmental Factor | Description | Potential Impact on Confabulation | Effectiveness (Scale of 1-5, 5 being highest) |
|---|---|---|---|
| Familiar Objects | Personal belongings, photos, familiar items | Provides comfort, reduces anxiety, connects to past | 4 |
| Clear Time Cues | Large clocks, calendars with clear dates | Reduces confusion about time, increases orientation | 4 |
| Minimal Clutter | Organized spaces, clear pathways | Reduces sensory overload, improves navigation | 3 |
| Calming Sensory Environment | Soft lighting, muted colors, calming music | Reduces anxiety, promotes relaxation | 4 |
| Consistent Routines | Regular daily schedules, predictable activities | Provides structure, reduces confusion, promotes predictability | 5 |
Managing Underlying Conditions
Confabulation in dementia isn’t always a standalone issue. Often, it’s intertwined with other medical conditions that can exacerbate the symptoms. Understanding and addressing these underlying health problems is crucial for effectively managing confabulation and improving the overall well-being of the individual. Identifying and managing these conditions requires a collaborative approach between caregivers, family members, and medical professionals.A significant portion of confabulatory behaviors might stem from underlying medical issues.
These issues can range from easily treatable conditions to more complex ones, making early diagnosis and intervention vital. It’s important to remember that confabulation itself isn’t a disease but a symptom that can be linked to other underlying medical conditions. Therefore, a comprehensive approach that considers all potential factors is essential.
Impact of Underlying Conditions on Confabulation
Managing underlying medical conditions can significantly impact the frequency and severity of confabulatory episodes. Improved management of conditions like infections, dehydration, or medication side effects can often lead to a reduction in confabulatory behaviors. For instance, a patient experiencing a urinary tract infection might exhibit increased confusion and confabulation, which can be alleviated by treating the infection. Conversely, certain medications can induce or worsen confabulation as a side effect.
Potential Connections Between Medical Issues and Confabulatory Behaviors
Numerous medical conditions can potentially contribute to or exacerbate confabulatory behaviors in dementia. These include infections (like urinary tract infections or pneumonia), electrolyte imbalances, thyroid problems, vitamin deficiencies (especially B12), and even certain types of medication side effects. For example, a patient with uncontrolled diabetes might experience episodes of confabulation due to fluctuating blood sugar levels. Similarly, a medication interaction or an adverse reaction to a new prescription can also trigger confabulatory episodes.
Dealing with confabulation in dementia can be tricky, but understanding the underlying reasons can help caregivers respond more effectively. While there’s no magic bullet, staying informed about the latest advancements in COPD treatment, like what’s new in COPD treatment , can offer valuable insights into managing similar challenges related to cognitive function. Ultimately, a compassionate and patient approach is key to supporting individuals living with dementia.
Collaborative Approach with Medical Professionals
A structured and collaborative approach is crucial when working with medical professionals to address potential underlying medical conditions. Open communication with the patient’s physician is essential, sharing detailed information about the confabulatory episodes, including their frequency, context, and any potential triggers. This includes presenting medical records, providing a detailed account of the patient’s daily routine, and noting any recent changes in behavior or medical history.
- Documentation is key: Maintain a detailed log of confabulatory episodes, including the time, context, and any associated factors. This will be invaluable when discussing the situation with medical professionals.
- Shared decision-making: Collaborate with the medical team to develop a treatment plan that addresses both the underlying medical condition and the confabulatory behaviors.
- Regular follow-ups: Schedule regular check-ups with the physician to monitor the patient’s condition and adjust the treatment plan as needed. This ensures that the underlying conditions are addressed promptly.
Structured Approach to Identifying and Managing Contributing Medical Conditions
A systematic approach to identifying and managing potential contributing medical conditions involves a multi-faceted evaluation process. This involves a thorough review of the patient’s medical history, including any pre-existing conditions or recent illnesses. A comprehensive physical examination and appropriate diagnostic tests can help identify underlying issues.
- Medical History Review: Caregivers should meticulously review the patient’s medical history, noting any potential connections between pre-existing conditions and the observed confabulatory behaviors.
- Physical Examination: A thorough physical examination by the physician is crucial to identify any physical signs that might suggest underlying medical conditions.
- Diagnostic Testing: Diagnostic tests, such as blood tests, urine tests, or imaging studies, may be necessary to identify and diagnose potential medical conditions.
Illustrative Cases
Confabulation in dementia can manifest in various ways, making it crucial to understand how it presents itself in different individuals. Analyzing specific cases allows for a deeper comprehension of the challenges faced by both the person with dementia and their caregivers. By examining real-life situations, we can develop more effective strategies for managing and responding to confabulation, ultimately improving the quality of life for those affected.
Case Study: Mr. Johnson
Mr. Johnson, a 78-year-old man with a history of Alzheimer’s disease, frequently recounted vivid and detailed stories about his life, many of which were entirely fabricated. He would describe elaborate trips to exotic locations, meetings with famous personalities, and even interactions with relatives he had never known. These accounts were often plausible and engaging, but lacked any verifiable evidence.
His confabulations were not always harmful, but they could be frustrating for his family and disrupt his sense of reality, potentially leading to anxiety or agitation.
Evaluation and Management Methods
The evaluation of Mr. Johnson’s confabulation involved a comprehensive assessment of his cognitive abilities, including memory, attention, and language skills. Neuropsychological testing was crucial in determining the extent of his cognitive decline and identifying specific areas of impairment. His medical history, including medications and any potential underlying health issues, was also carefully reviewed. This multi-faceted approach allowed for a more accurate diagnosis and a tailored management plan.
Impact of Strategies on Well-being
The strategies employed to manage Mr. Johnson’s confabulation focused on fostering a supportive and reassuring environment. Caregivers were trained in specific communication techniques to validate his feelings and redirect his attention. Simple, structured routines and predictable activities helped reduce anxiety and disorientation. By creating a calm and consistent environment, the strategies employed had a positive impact on Mr.
Johnson’s overall well-being. He reported feeling more secure and less overwhelmed, leading to a decrease in agitation and a corresponding improvement in his mood.
Response Strategies and Effectiveness
Communication techniques, such as using open-ended questions and active listening, were employed to encourage Mr. Johnson to express his feelings without feeling challenged or judged. Instead of directly contradicting his fabricated accounts, caregivers focused on validating his emotional experiences. For example, if Mr. Johnson described a happy encounter, caregivers acknowledged his joy rather than questioning the accuracy of the event.
This approach was highly effective in managing the confabulation episodes. Caregivers also used redirection techniques to gently steer the conversation towards more realistic and positive topics. This method successfully mitigated the emotional distress associated with confabulation. Structured activities and a predictable daily routine proved invaluable in maintaining a sense of normalcy and reducing disorientation, which in turn minimized the frequency of confabulation episodes.
Visual cues and memory aids were also incorporated to help Mr. Johnson recall real-life events and experiences. The use of these techniques further contributed to a decrease in confabulatory episodes.
Final Review
In conclusion, responding to confabulation in dementia requires a multifaceted approach that addresses the individual’s unique needs and challenges. By understanding the underlying mechanisms, identifying triggers, and implementing effective communication and environmental strategies, caregivers and healthcare professionals can create a supportive and meaningful experience for individuals with dementia. This guide aims to empower caregivers with the knowledge and tools to navigate these complex situations with compassion and empathy.