Rectal ulcer overview and more: Understanding rectal ulcers involves exploring their diverse types, common causes, and a range of potential symptoms. This comprehensive guide will delve into the complexities of these conditions, providing a detailed overview of diagnosis, treatment options, and preventative measures. From ischemic to inflammatory and infectious ulcers, we’ll uncover the factors contributing to their development, the diagnostic processes employed, and the various approaches to managing these often-challenging issues.
This exploration will cover the full spectrum of rectal ulcer considerations, from identifying the risk factors and potential complications to examining the diverse treatment options available. We’ll also discuss the importance of preventative strategies and the vital role of supportive care in managing the condition. The detailed tables and illustrations will further enhance our understanding, offering a comprehensive and visual approach to the topic.
Introduction to Rectal Ulcers
Rectal ulcers are sores that develop within the lining of the rectum, the final portion of the large intestine. These lesions can vary in size, depth, and cause, impacting both comfort and overall health. Understanding the different types, causes, and symptoms is crucial for prompt diagnosis and appropriate treatment.Rectal ulcers are a relatively common condition that can affect individuals of various ages and backgrounds.
While often associated with more serious underlying conditions, many cases resolve with appropriate medical intervention. Early detection and treatment are key to preventing potential complications and ensuring a positive outcome.
Types of Rectal Ulcers
Rectal ulcers are broadly categorized based on their underlying cause. Understanding these categories allows for a more targeted approach to diagnosis and treatment. Different types of ulcers may have different symptoms and potential complications.
- Ischemic Ulcers: These ulcers arise due to a reduced blood supply to the rectal area. Factors such as narrowing of blood vessels or reduced blood flow, sometimes related to underlying circulatory problems, can lead to ischemic ulcers. For example, patients with peripheral artery disease (PAD) might experience reduced blood flow, potentially leading to ischemic ulcers.
- Inflammatory Ulcers: These ulcers are frequently associated with inflammatory bowel diseases (IBD), such as Crohn’s disease and ulcerative colitis. The chronic inflammation in these conditions can lead to ulcerations within the rectum. Symptoms of IBD may include abdominal pain, diarrhea, and fatigue.
- Infectious Ulcers: Infections, both bacterial and viral, can cause inflammation and ulceration within the rectum. Bacterial infections, like those caused by certain strains of bacteria, can cause rectal ulcers. Viral infections can also play a role, such as herpes simplex virus, although this is less common.
Common Causes of Rectal Ulcers
Several factors can contribute to the development of rectal ulcers. Identifying the underlying cause is crucial for effective management.
- Inflammatory Bowel Disease (IBD): As mentioned, chronic inflammation associated with Crohn’s disease and ulcerative colitis is a significant cause of rectal ulcers.
- Ischemic Conditions: Reduced blood flow to the rectum, potentially from narrowed blood vessels or other circulatory issues, can lead to ischemic ulcers. This might occur in patients with underlying cardiovascular disease.
- Infections: Bacterial and viral infections can directly irritate and damage the rectal lining, leading to ulcer formation. Examples include infections caused by certain bacteria or viruses.
- Radiation Therapy: Radiation therapy for nearby cancers can sometimes cause damage to the rectum, resulting in ulcerations.
- Trauma: Physical trauma to the rectal area, such as from certain medical procedures or injury, can lead to ulcer formation.
Symptoms of Rectal Ulcers
Symptoms associated with rectal ulcers can vary depending on the underlying cause and the severity of the condition.
- Pain: Pain during bowel movements is a common symptom, ranging from mild discomfort to severe pain.
- Bleeding: Blood in the stool is a significant indicator of rectal ulceration.
- Discharge: Mucus or pus discharge from the rectum is possible.
- Changes in bowel habits: Changes in bowel frequency or consistency, such as diarrhea or constipation, can be associated with rectal ulcers.
- Fever: In some cases, a fever might indicate an infection as a cause of the ulcer.
Types of Rectal Ulcers: A Summary
| Type of Rectal Ulcer | Possible Causes | Common Symptoms | Potential Complications |
|---|---|---|---|
| Ischemic | Reduced blood flow (e.g., peripheral artery disease), narrowing of blood vessels | Pain, bleeding, changes in bowel habits | Severe bleeding, perforation, infection |
| Inflammatory | Inflammatory bowel disease (Crohn’s disease, ulcerative colitis), certain medications | Pain, bleeding, diarrhea, abdominal pain | Strictures, fistula formation, cancer |
| Infectious | Bacterial or viral infections, foreign bodies | Pain, bleeding, discharge, fever | Sepsis, abscess formation |
Diagnosis and Evaluation
Uncovering the cause of rectal ulcers requires a systematic approach involving a combination of methods. A thorough understanding of the patient’s medical history, a comprehensive physical examination, and sophisticated diagnostic tools are crucial for accurate diagnosis and appropriate management. This process helps to pinpoint the underlying issue and guide treatment strategies, leading to better patient outcomes.Understanding the various diagnostic procedures, their advantages and limitations, and their respective roles in identifying the cause of rectal ulcers is paramount.
Rectal ulcers can be a real pain, and understanding their various causes and treatments is key. While we’re diving into the details of rectal ulcer overview and more, it’s worth considering how different conditions can affect our overall well-being. For instance, knowing the life expectancy for stage 3 lung cancer can help patients and their families prepare for the future.
what is stage 3 lung cancer life expectancy Ultimately, though, understanding rectal ulcer overview and more is crucial for proactive health management.
This knowledge allows healthcare professionals to tailor the diagnostic approach to the individual patient, optimizing the likelihood of an accurate diagnosis and efficient treatment planning.
Rectal ulcers can sometimes be a symptom of underlying issues, like inflammatory conditions or even iron deficiency anemia. Understanding the causes is key, and knowing how to address potential deficiencies like iron is crucial. Fortunately, there are effective treatments for iron deficiency anemia, which can significantly improve overall health and potentially alleviate the symptoms of rectal ulcers. Exploring these options, like those outlined in this resource on treatments for iron deficiency anemia , could lead to a more comprehensive approach to managing rectal ulcer issues and improving your overall well-being.
More research into the root causes is vital to developing a comprehensive treatment plan for rectal ulcer overview and more.
Medical History and Physical Examination
A detailed medical history is essential in identifying potential risk factors and contributing conditions. This includes inquiries about recent infections, medications, dietary habits, and previous medical issues. The physical examination, focusing on the rectal area, allows for the detection of visible abnormalities, such as inflammation, bleeding, or masses. These initial assessments can often point towards possible causes and guide the subsequent diagnostic steps.
Imaging Techniques
Imaging plays a critical role in evaluating the extent and characteristics of rectal ulcers. Endoscopy, particularly colonoscopy, is a valuable tool for visualizing the lining of the rectum and colon. It allows for direct observation of the ulcer, its location, size, and depth. Colonoscopy can identify other potential sources of bleeding or inflammation in the colon. Furthermore, the procedure enables the collection of tissue samples (biopsies) for further analysis.
Rectal ulcers can be tricky, and understanding the various causes and treatments is key. Sometimes, minimally invasive procedures, like those using a Kirschner wire ( what is a Kirschner wire ), are employed. Learning about these techniques is helpful for anyone seeking more information about rectal ulcer overview and potential treatment options.
Biopsy Acquisition
Obtaining biopsies is a crucial step in the diagnostic process. These tissue samples are examined microscopically by pathologists to determine the precise nature of the ulcer, identifying the underlying cause and ruling out potential malignancies. Biopsy techniques ensure the collection of representative samples, maximizing the accuracy of the pathological analysis. A proper biopsy procedure minimizes the risk of complications and ensures the quality of the tissue sample for accurate diagnosis.
Comparison of Diagnostic Procedures
| Diagnostic Procedure | Advantages | Disadvantages | Typical Use in Rectal Ulcer Diagnosis |
|---|---|---|---|
| Medical History and Physical Examination | Initial screening, identifies potential risk factors, non-invasive, cost-effective | Limited in identifying the precise cause, may not detect subtle abnormalities | Initial assessment, guides further investigations |
| Endoscopy (e.g., Colonoscopy) | Direct visualization of the rectal and colonic lining, allows for biopsy collection, identifies extent of ulceration | May be uncomfortable for some patients, carries minimal risk of complications | Detailed evaluation of rectal ulcer, detection of associated lesions, tissue sampling |
| Biopsy | Provides definitive pathological diagnosis, identifies causative agents, differentiates benign from malignant conditions | Invasive procedure, may result in mild discomfort or complications | Confirms the nature of the ulcer, distinguishes between various conditions |
Risk Factors and Complications
Rectal ulcers, while often treatable, can sometimes lead to complications. Understanding the risk factors and potential consequences is crucial for proactive management and improved outcomes. Identifying predisposing conditions and potential complications empowers individuals and healthcare providers to take preventive measures and implement appropriate treatment strategies.
Risk Factors
Several factors can increase the likelihood of developing rectal ulcers. These include inflammatory bowel diseases (IBD), such as Crohn’s disease and ulcerative colitis, which frequently manifest with ulcerative lesions in the digestive tract. Certain medications, radiation therapy, and infections also contribute to the risk. Genetic predisposition and a weakened immune system can also play a role. Furthermore, some individuals with a history of rectal trauma or injury might be more susceptible to developing ulcers.
Potential Complications
Rectal ulcers can lead to a range of complications, some of which are serious. Bleeding is a common complication, potentially causing significant blood loss and requiring medical intervention. Perforation, a tear in the rectal wall, can occur and is a serious medical emergency requiring prompt surgical repair. Strictures, or narrowing of the rectum, can also develop, impacting bowel function and necessitating intervention to restore normal passage.
Long-Term Effects of Untreated Ulcers
Untreated rectal ulcers can have long-lasting consequences. Persistent inflammation and ulceration can lead to scarring and narrowing of the rectal canal, causing chronic pain and discomfort. Furthermore, the condition can increase the risk of colorectal cancer, though this is not a direct causal relationship, but rather a heightened risk factor. It is vital to promptly address any suspected rectal ulcer to mitigate these potential complications.
Table of Risk Factors, Complications, and Management
| Risk Factor | Associated Complications | Preventive Measures | Treatment Options |
|---|---|---|---|
| Inflammatory Bowel Disease (IBD) | Bleeding, perforation, strictures, chronic inflammation | Maintaining a healthy diet, managing stress, adherence to medication regimens, and regular medical check-ups. | Medication management (e.g., corticosteroids, immunomodulators), surgery (in severe cases), and lifestyle adjustments. |
| Radiation Therapy | Ulceration, bleeding, narrowing of the rectal canal | Protecting the rectal area from further radiation exposure if possible, and monitoring for any changes. | Medications to reduce inflammation, and supportive care to manage symptoms. |
| Certain Medications | Ulceration, bleeding | Proper medication management, adherence to prescribed doses, and close monitoring by healthcare providers. | Adjusting medication, switching to alternative medications if possible, and supportive care. |
| Infections | Ulceration, bleeding | Maintaining hygiene, vaccination, and prompt treatment of infections. | Antibiotics or antiviral medications, depending on the specific infection. |
| Rectal Trauma | Ulceration, bleeding, infection | Avoiding activities that could lead to rectal injury, and practicing safe sexual practices. | Surgical repair, pain management, and infection control measures. |
Treatment Options
Treating rectal ulcers involves a multifaceted approach tailored to the individual’s specific condition. The primary goal is to address the underlying cause, alleviate symptoms, and promote healing. This often requires a combination of medical interventions and lifestyle adjustments.
Medications
Medications play a crucial role in managing rectal ulcers. Anti-inflammatory drugs, such as corticosteroids, are often used to reduce inflammation and pain. These drugs can be administered topically, or systemically, depending on the severity and location of the ulcer. In some cases, antibiotics might be necessary if an infection is present. The selection of medication and dosage will be determined by the physician based on a comprehensive evaluation of the patient’s condition.
Surgical Interventions, Rectal ulcer overview and more
Surgical intervention might be considered in cases where the ulcer is severe, persistent, or unresponsive to other treatments. The type of surgical procedure will vary depending on the nature of the ulcer and its impact on the surrounding tissues. For instance, in some cases, a simple resection of the affected tissue may suffice. In more complex scenarios, reconstructive surgery may be required to restore normal function and prevent complications.
Careful consideration of the potential benefits and risks is essential in deciding on surgical intervention.
Supportive Care
Supportive care is vital in managing the symptoms and promoting healing. This includes dietary modifications, such as avoiding foods that irritate the affected area, and maintaining a healthy lifestyle that includes adequate rest and hydration. Maintaining good hygiene in the anal area is crucial to prevent further complications. Furthermore, stress management techniques can help reduce inflammation and promote overall well-being.
Comparison of Treatment Options
| Treatment Option | Effectiveness | Potential Side Effects | Suitability |
|---|---|---|---|
| Anti-inflammatory Medications (e.g., corticosteroids) | Generally effective in reducing inflammation and pain. | Potential for side effects such as increased risk of infection, thinning of the skin, and gastrointestinal issues, depending on dosage and duration of use. | Suitable for mild to moderate rectal ulcers, especially when the inflammation is prominent. |
| Antibiotics | Effective in treating infections that may contribute to the ulcer. | Potential side effects include allergic reactions, disruption of gut flora, and development of antibiotic resistance. | Suitable for cases where an infection is identified as a contributing factor. |
| Surgical Intervention | Highly effective in treating severe, persistent, or unresponsive ulcers. | Potential for complications such as bleeding, infection, scarring, and altered bowel function, though the risk depends on the specific procedure. | Suitable for cases where other treatments have failed, or where the ulcer is severe enough to warrant a surgical approach. |
| Supportive Care | Important in managing symptoms and promoting healing. | No direct side effects, but inadequate care may delay healing. | Suitable for all cases to enhance treatment efficacy and improve patient comfort. |
Prevention and Management

Rectal ulcers, while often manageable, can significantly impact daily life. Understanding preventive strategies and effective management techniques is crucial for minimizing discomfort and promoting healing. This section will explore key approaches to both preventing future episodes and effectively managing existing symptoms.
Preventive Strategies
Preventing rectal ulcers often involves addressing underlying factors that contribute to their development. A balanced diet rich in fiber can help maintain healthy bowel movements, reducing strain and irritation. Maintaining a healthy weight and regular exercise are also beneficial. Avoiding prolonged sitting and incorporating regular movement into daily routines can help prevent the pooling of blood in the rectal area, potentially lessening the risk of injury.
Smoking cessation and limiting alcohol consumption are also vital steps in reducing the overall risk of various health issues, including rectal ulcers.
Symptom Management Advice
Effective symptom management for rectal ulcers focuses on reducing inflammation and promoting healing. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help alleviate discomfort. Warm sitz baths can soothe the affected area. Maintaining good hygiene is paramount, ensuring regular cleansing of the anal area with gentle, mild soaps.
Lifestyle Modifications for Healing
Lifestyle modifications play a significant role in supporting the healing process. A diet rich in vitamins, minerals, and antioxidants can bolster the body’s natural healing abilities. Stress management techniques, such as meditation or yoga, can help reduce inflammation and promote overall well-being. Adequate hydration is crucial for maintaining bowel regularity and preventing constipation, which can exacerbate ulcer symptoms.
Avoiding foods that may trigger irritation, such as spicy or acidic foods, can also be helpful.
Home Management Recommendations
Implementing certain home management strategies can help alleviate symptoms and promote healing.
- Gentle Cleansing: Use lukewarm water and a soft cloth or washcloth for cleansing. Avoid harsh soaps or scrubbing, as these can irritate the area.
- Dietary Adjustments: Consider a diet rich in fiber, and avoid foods that might worsen irritation. Examples of such foods include highly spiced, acidic, or overly processed items.
- Over-the-Counter Medications: Consult with a healthcare provider before using any over-the-counter pain relievers, but mild pain relievers can help manage discomfort.
- Warm Compresses/Sitz Baths: Soaking in a warm sitz bath can provide soothing relief for the inflamed area. The warmth helps relax muscles and decrease inflammation.
- Regular Bowel Habits: Maintain regular bowel habits by incorporating fiber-rich foods into the diet and avoiding constipation. Regularity reduces strain on the rectum.
- Stress Management: Chronic stress can worsen inflammation. Incorporate stress-reducing activities like yoga, meditation, or deep breathing exercises into your routine.
Resources for Support and Education
Accessing reliable information and support networks can significantly benefit individuals managing rectal ulcers. Consult a healthcare provider for personalized advice and treatment plans. Support groups can offer a platform for sharing experiences and learning from others who have gone through similar situations. Reliable online resources, including reputable medical websites and patient advocacy organizations, provide valuable information about managing rectal ulcers.
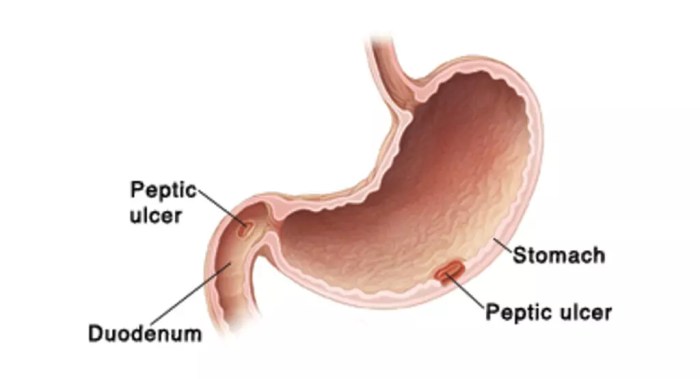
Illustrations and Visual Aids: Rectal Ulcer Overview And More
Visual aids are crucial for understanding complex medical conditions like rectal ulcers. Illustrations and diagrams can help patients and healthcare professionals visualize the location, appearance, and inflammatory processes involved, making diagnosis and treatment planning more effective. They also aid in explaining the stages of healing and potential complications.
Rectal Ulcer Location
This illustration would show a cross-section of the rectum, highlighting the location of the ulcer. The rectum is depicted as a portion of the large intestine, positioned in the pelvis. The ulcer would be clearly marked, showing its proximity to the anal canal and the surrounding tissues. Key anatomical structures like the sphincter muscles, blood vessels, and nerves should be visible to demonstrate the potential impact of the ulcer on these structures.
The surrounding healthy rectal tissue would be contrasted with the ulcer to clearly delineate the affected area.
Endoscopic Appearance of a Rectal Ulcer
An endoscopic image would show a shallow or deep erosion in the rectal lining. The ulcer’s edges might appear irregular, with a reddish-brown or yellowish base. The surrounding rectal mucosa might appear inflamed or swollen. The endoscopic image would clearly differentiate the ulcer from the healthy mucosa. The depth of the ulcer and the presence of any exudates (pus or fluid) should be noted in the image description.
Inflammatory Process in a Rectal Ulcer
An illustration of the inflammatory process would depict a magnified view of the ulcer’s lining. The inflammatory cells, such as neutrophils and lymphocytes, would be shown migrating to the affected area. The illustration would highlight the presence of edema (swelling) and vascular congestion in the ulcer’s immediate vicinity. The illustration should depict the progression of inflammation, from the early stages of infiltration to the later stages of tissue repair.
A comparison to a normal rectal lining would visually demonstrate the extent of the inflammatory response.
Stages of Healing for a Rectal Ulcer
A visual representation of the healing process would showcase sequential stages, starting with the acute ulcer. The first stage could depict the ulcer with a clearly defined margin and a reddish-brown base. The second stage would demonstrate a decrease in inflammation, with a reduction in redness and edema. The third stage would show a healing process with granulation tissue filling the ulcer bed.
The final stage would illustrate a completely healed rectal lining, with no visible signs of the previous ulcer. The illustrations should show the progression from inflammation to resolution, clearly indicating the time frame for each stage. These stages could be illustrated with captions describing the key features of each stage.
Last Point
In conclusion, rectal ulcers, while potentially complex, are manageable with a comprehensive understanding of their various types, causes, and potential complications. This overview has highlighted the importance of early diagnosis and appropriate treatment. By understanding the risk factors, the different treatment approaches, and the potential for complications, individuals can take proactive steps to manage and prevent rectal ulcers.
The provided resources and lifestyle recommendations offer a valuable roadmap for navigating this condition.

