Proprioception in multiple sclerosis lays bare the intricate relationship between the nervous system and our sense of body awareness. This complex topic explores how multiple sclerosis impacts our ability to perceive our body’s position and movement, leading to a cascade of effects on daily activities. We’ll delve into the neurological underpinnings of proprioception, the specific ways MS affects it, and ultimately, the rehabilitation strategies to help manage these challenges.
From understanding the fundamental neural pathways involved in proprioception to the practical implications of impaired proprioception in everyday tasks, this discussion will cover various aspects. We’ll examine how proprioceptive dysfunction impacts balance, gait, and mobility in MS patients, ultimately exploring the profound impact on their quality of life.
Introduction to Proprioception

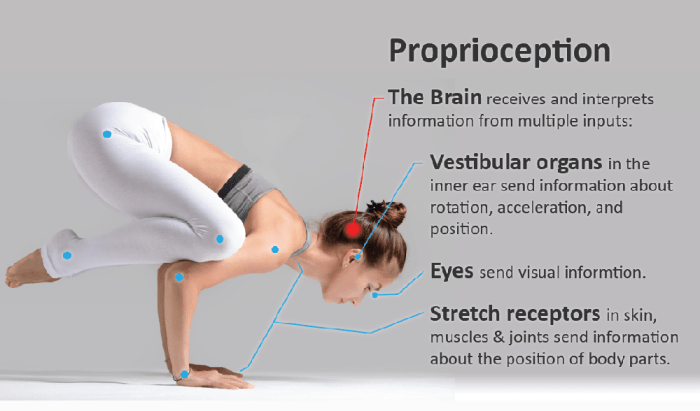
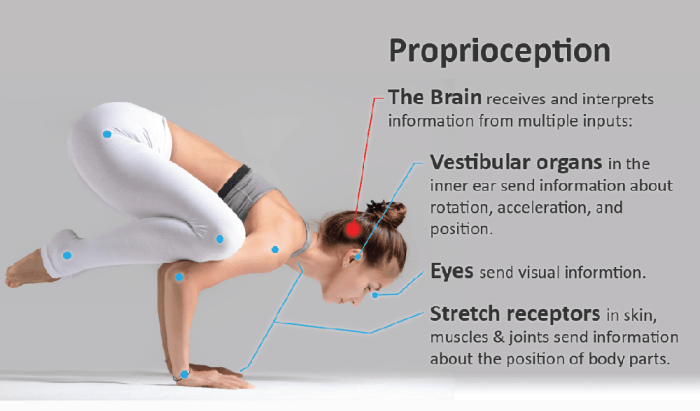
Proprioception is our sense of body position and movement. It’s a crucial component of motor control, allowing us to navigate the world without constantly looking at our limbs. Imagine walking down the street – you don’t need to consciously think about how to move your legs; your body automatically adjusts. This seamless execution relies heavily on proprioceptive input.
This input is constantly being processed and used to adjust our movements, enabling us to perform tasks ranging from simple actions like picking up a glass to complex ones like playing a musical instrument.The brain interprets signals from various sensory receptors throughout the body to understand where our limbs are in space. These signals provide vital information about joint position, muscle length, and tension, allowing for precise and coordinated movements.
Accurate proprioception is fundamental to our overall sense of self and the environment.
Neural Pathways Involved in Proprioception
Proprioceptive information travels through complex neural pathways to reach the brain. Sensory receptors in muscles (muscle spindles), tendons (Golgi tendon organs), and joints (joint receptors) detect changes in body position and movement. These receptors convert mechanical stimuli into electrical signals that are transmitted along sensory neurons. These signals travel through the spinal cord, up the dorsal columns, and ultimately reach the cerebellum and somatosensory cortex in the brain.
The brain integrates this information with other sensory inputs to create a comprehensive understanding of body position and movement.
Assessment of Proprioception
Assessing proprioception involves evaluating the ability to sense body position and movement without visual cues. Common assessments include:
- Joint Position Sense: This test gauges the accuracy with which a person can identify the position of a joint, typically a finger or toe, in space.
- Kinesthesia: This involves determining the direction and range of movement of a joint.
- Romberg Test: This test evaluates balance and stability, often used to detect proprioceptive deficits. Loss of balance is indicative of a problem with proprioception.
These assessments can be performed by trained professionals, such as physical therapists or neurologists. The results can be used to diagnose conditions affecting the nervous system, including multiple sclerosis.
Types of Proprioceptive Input
Different types of sensory receptors provide various forms of proprioceptive information. The table below summarizes the characteristics of these receptors:
| Type of Receptor | Location | Stimulus Detected | Role in Movement |
|---|---|---|---|
| Muscle Spindles | Skeletal Muscles | Changes in muscle length and rate of change | Maintaining muscle length, preventing overstretching, and initiating reflex contractions |
| Golgi Tendon Organs | Tendons | Changes in muscle tension | Protecting tendons from excessive force, modulating muscle activity |
| Joint Receptors | Joints | Changes in joint position and movement | Providing information about joint angle and range of motion |
Proprioception in Healthy Individuals
Proprioception, our sense of body position and movement, is crucial for everyday tasks. It’s the silent partner in our motor control system, constantly providing feedback to the brain about where our limbs are in space. This information is vital for smooth, coordinated movements, and its absence or impairment can significantly impact our ability to function.Understanding proprioception’s role in healthy individuals is essential for recognizing the implications of its disruption in conditions like multiple sclerosis.
This understanding provides a baseline for evaluating how proprioceptive deficits affect movement and coordination in those with MS.
Importance for Motor Control and Coordination
Proprioception acts as a crucial feedback loop, enabling precise and controlled movements. Specialized sensory receptors in muscles, tendons, and joints send signals to the brain regarding the position, tension, and movement of body parts. The brain uses this information to refine motor commands, ensuring smooth and efficient execution of tasks. Without this constant feedback, movements would be jerky, imprecise, and likely to lead to falls or injuries.
Reliance on Proprioceptive Feedback in Activities
Various activities, from simple actions like reaching for a glass to complex tasks like walking or playing a musical instrument, rely heavily on proprioceptive feedback.
- Walking, for example, involves a constant stream of proprioceptive information. The brain receives data on limb position, joint angles, and muscle tension to adjust steps, maintain balance, and adapt to uneven surfaces. This continuous monitoring allows us to navigate our environment smoothly and efficiently.
- In sports, proprioception is essential for precise movements and quick reactions. Athletes rely on this sensory input to track their body’s position during activities like running, jumping, or catching a ball. The ability to perceive limb position and adjust accordingly allows for improved performance and reduced risk of injury.
Examples of Disrupted Proprioception
Disrupted proprioception can manifest in several ways, leading to noticeable impairments in motor skills.
Navigating the complexities of multiple sclerosis often involves a range of challenges, including disruptions to proprioception, the sense of body position. Finding the right medication can be a crucial part of managing these symptoms, and understanding comparisons like effexor xr vs lexapro is important for individuals exploring treatment options. Ultimately, regaining a strong sense of body awareness remains a key goal in managing MS and improving daily life.
- Uncoordinated movements: Individuals with disrupted proprioception may experience jerky, uncoordinated movements, difficulty with balance, and a general lack of control over their limbs. Imagine trying to walk a straight line while blindfolded – this is akin to the experience of someone with significantly impaired proprioception.
- Difficulty with tasks requiring precise movements: Performing tasks that require fine motor control, such as buttoning a shirt or writing, can become challenging. The lack of precise body position awareness can lead to inaccurate movements and struggles with dexterity.
- Increased risk of falls: Proprioception is critical for maintaining balance and stability. When this sensory input is compromised, the risk of falls and injuries increases. This is particularly evident in individuals with conditions like vestibular disorders or those recovering from injuries.
- Changes in gait: Walking becomes unsteady and less coordinated. A person might have a tendency to stumble, widen their base of support, or exhibit a shuffling gait pattern. These changes are noticeable in daily activities, impacting overall mobility.
Proprioception in Multiple Sclerosis (MS)
Proprioception, the sense of body position and movement, plays a crucial role in our daily activities. It allows us to navigate our environment, perform tasks with precision, and maintain balance. In multiple sclerosis (MS), a chronic autoimmune disease affecting the central nervous system, proprioceptive function often deteriorates, leading to various functional impairments.The mechanisms through which MS affects proprioception are multifaceted, stemming from the disease’s disruptive impact on the neural pathways responsible for transmitting proprioceptive information.
Myelin, the protective sheath surrounding nerve fibers, is a primary target in MS. Damage to myelin impairs the efficient transmission of nerve impulses, which are essential for accurate proprioceptive feedback. This demyelination process, coupled with axonal damage, results in impaired signal transduction, hindering the brain’s ability to accurately perceive body position and movement.
Neurological Damage Underlying Proprioceptive Dysfunction
MS causes demyelination and axonal loss primarily in the sensory tracts of the spinal cord and brain stem, which are critical for transmitting proprioceptive signals. This damage disrupts the smooth flow of information from the body’s sensory receptors to the brain, resulting in a reduced or distorted awareness of body position and movement. The specific locations and extent of damage vary between individuals, contributing to the diverse range of symptoms experienced.
Inflammation and scarring (sclerosis) further contribute to the progressive degradation of these pathways, compounding the proprioceptive impairment.
Common Symptoms of Proprioceptive Impairment
Proprioceptive deficits in MS patients manifest in various ways, often affecting coordination, balance, and overall motor function. These symptoms can range from subtle difficulties to severe impairments, impacting daily activities. Common symptoms include:
- Ataxia: An inability to coordinate voluntary movements, leading to unsteady gait, clumsiness, and difficulty with tasks requiring precision. For example, a person with ataxia might have trouble walking a straight line or buttoning a shirt.
- Balance problems: Difficulties maintaining equilibrium, leading to frequent falls or a sense of instability. This can be particularly problematic when navigating stairs or uneven surfaces.
- Loss of limb position sense: Difficulty in identifying the position of one’s limbs without visual feedback. This can make it challenging to perform tasks that require awareness of limb position, such as dressing or manipulating objects.
- Dysmetria: Inability to accurately judge the distance or range of movement, resulting in overshooting or undershooting intended targets. For instance, a person with dysmetria might miss a target when trying to reach for an object.
- Hypotonia: Reduced muscle tone, contributing to weakness and difficulty with movement initiation. This can lead to difficulties with tasks requiring muscle strength and control.
Potential Causes of Proprioceptive Problems in MS
The following table Artikels potential causes contributing to proprioceptive issues in individuals with MS. It is crucial to understand that these factors are interconnected and can manifest in various combinations within each patient.
Understanding proprioception, or your body’s awareness of its position in space, is crucial for everyday tasks. Unfortunately, in multiple sclerosis, this sense can be significantly affected. This often leads to balance issues and challenges with coordination. While not directly related, quadruple bypass heart surgery, a procedure where multiple blockages in the coronary arteries are treated, can sometimes improve overall health, and therefore potentially impact proprioception.
Knowing how these different health factors can influence one another is key to a comprehensive understanding of the body. The effects of proprioception issues on MS patients can be lessened by finding the right treatment and care. For more details on quadruple bypass heart surgery, check out this informative resource: what is quadruple bypass heart surgery.
Ultimately, regaining and maintaining proprioception remains a significant focus in MS management.
| Potential Cause | Description |
|---|---|
| Demyelination of sensory pathways | Damage to the myelin sheath surrounding nerve fibers in the spinal cord and brain stem disrupts the transmission of sensory information, including proprioceptive input. |
| Axonal loss | The degeneration of nerve fibers (axons) themselves directly impairs the transmission of nerve impulses, leading to a reduction in proprioceptive signals. |
| Inflammation | Inflammation in the central nervous system can further exacerbate demyelination and axonal damage, worsening proprioceptive dysfunction. |
| Sclerosis (scar tissue formation) | Scar tissue formation in the CNS can impede the normal transmission of nerve impulses, contributing to the disruption of proprioceptive signaling. |
| Cerebellar involvement | Damage to the cerebellum, which plays a vital role in coordinating movement and balance, can result in ataxia and proprioceptive difficulties. |
Impact of Proprioception Impairment in MS
Proprioception, our sense of body position and movement, plays a crucial role in coordinating daily activities. When proprioception is impaired, as it often is in multiple sclerosis (MS), the consequences can significantly impact a person’s quality of life. This impairment affects not only basic movements but also more complex tasks and social interactions. Understanding these effects is essential for developing appropriate strategies to manage MS and improve functional independence.Impaired proprioception in MS directly influences motor control, balance, and coordination.
This leads to a range of difficulties in performing activities of daily living (ADLs) and participating in social activities. The impact varies from person to person, depending on the extent of proprioceptive loss and the overall severity of MS.
Effects on Daily Activities
Proprioceptive deficits in MS patients can manifest in subtle ways, impacting seemingly simple tasks. Difficulties arise when performing tasks requiring precise movements and coordination, such as buttoning a shirt, using utensils, or writing. The inability to accurately perceive body position can also lead to awkward movements and increased risk of falls.
Impact on Balance, Gait, and Mobility
Proprioception is essential for maintaining balance and coordinating gait. In MS, impaired proprioception can result in unsteady gait, difficulty with turning, and increased risk of falls. These problems can significantly limit mobility, impacting a person’s ability to navigate their environment and participate in desired activities. For example, a person with MS might find it challenging to walk up stairs or cross uneven terrain due to their proprioceptive deficit.
Impact on Activities of Daily Living (ADLs)
A diminished sense of body position and movement directly affects many ADLs. Simple tasks such as dressing, bathing, eating, and using the restroom become more challenging and time-consuming. The lack of precise body awareness can lead to clumsiness and potential injuries. For example, a person with MS might struggle to tie their shoes or brush their teeth effectively due to proprioceptive difficulties.
Potential Impact on Social Participation
The limitations imposed by proprioceptive deficits in MS can affect social participation. Difficulty with balance, gait, and coordination can make it challenging to participate in social activities, such as attending social gatherings, playing sports, or even simply engaging in conversations. Fear of falling or embarrassment due to clumsiness can also discourage social interaction. A person with MS might avoid social situations due to the difficulties they anticipate encountering.
Assessment and Management of Proprioceptive Impairment
Understanding proprioceptive deficits in multiple sclerosis (MS) is crucial for developing effective management strategies. These deficits can significantly impact a person’s ability to perform daily tasks, navigate environments, and maintain balance. This section details methods for assessing and managing proprioceptive impairments in MS patients.Assessing proprioceptive function in MS patients requires a multifaceted approach. Different methods are used to evaluate the subtle changes in awareness of body position and movement.
These assessments are essential for identifying the extent of the impairment and tailoring interventions to address specific needs.
Proprioceptive Assessment Procedures in MS Patients
A comprehensive assessment of proprioception in MS patients should involve a series of standardized tests, adapted to suit the individual’s abilities and limitations. This individualized approach is critical to ensure accurate results and prevent misdiagnosis. The process must consider the potential for fatigue, cognitive impairment, and other MS symptoms that may influence test performance.
Methods for Assessing Proprioceptive Function in MS Patients, Proprioception in multiple sclerosis
Several methods are employed to assess proprioceptive function, each with its strengths and limitations. The choice of method often depends on the specific aspect of proprioception being assessed and the patient’s capacity to participate.
- Joint Position Sense Tests: These tests evaluate the patient’s ability to identify the position of a joint in space. Common tests involve passively moving a joint and asking the patient to identify the direction and degree of movement. Different joint positions and speeds of movement can be used to evaluate the sensitivity of the patient’s proprioceptive system. For example, a patient might be asked to identify whether a finger is pointing up or down, or if a leg is straight or bent.
This allows the clinician to gauge the patient’s accuracy and responsiveness.
- Kinesthesia Tests: These tests assess the patient’s awareness of movement. The examiner moves a limb passively and asks the patient to describe the direction and extent of the movement. These tests can be performed with various body parts and speeds of movement, providing a more comprehensive understanding of the patient’s kinesthetic awareness. For instance, a patient might be asked to describe whether a leg is being moved forward or backward, or if an arm is being extended or flexed.
- Balance Tests: Balance tests, like the Romberg test or the tandem stance test, indirectly assess proprioception. Impaired proprioception often manifests as a greater tendency toward balance problems. These tests are crucial for evaluating the patient’s stability and how proprioceptive deficits affect their ability to maintain equilibrium.
Comparison and Contrast of Assessment Tools
Different assessment tools have varying levels of sensitivity and specificity, and each has advantages and disadvantages.
- Standardized tests (e.g., Modified Clinical Test of Sensory Function): These tests provide a standardized framework for assessing proprioception, allowing for comparisons across patients and over time. However, they might not always capture the subtle nuances of proprioceptive impairment in MS.
- Clinician-developed tests: These tests can be tailored to the specific needs of the patient and provide a more individualized assessment. However, standardization and reliability may be lower compared to standardized tests.
- Neurophysiological tests (e.g., electromyography): These tests provide insights into the underlying neurological mechanisms of proprioceptive impairment. However, they are often more complex and expensive compared to other assessment methods.
Common Interventions for Proprioceptive Deficits in MS
Various interventions can help manage proprioceptive deficits in MS patients. A tailored approach is essential, considering the patient’s specific needs and functional limitations.
Proprioception, the sense of body position, often gets significantly impaired in multiple sclerosis (MS). This can lead to balance issues and make everyday tasks challenging. Interestingly, similar issues with balance and coordination can sometimes be seen in patients recovering from achilles tendon rupture, which can sometimes be treated non-operatively with physical therapy and rehabilitation. achilles tendon rupture non operative treatment can be an important part of the recovery process.
Fortunately, there are often effective strategies to help regain proprioceptive function in MS, like targeted exercises and specialized therapies.
| Intervention Type | Description | Potential Benefits |
|---|---|---|
| Physical Therapy | Exercises focusing on balance, coordination, and proprioceptive retraining. These may include activities like standing exercises, gait training, and proprioceptive neuromuscular facilitation (PNF) techniques. | Improved balance, coordination, and reduced fall risk. |
| Occupational Therapy | Adaptive equipment and strategies to compensate for proprioceptive deficits in daily activities. This could involve modifying tasks, using assistive devices, or providing education on energy conservation techniques. | Improved independence in daily tasks, improved mobility, and enhanced quality of life. |
| Sensory Stimulation | Techniques like proprioceptive input (e.g., massage, resistance exercises) or visual cues to improve awareness of body position. | Increased body awareness and potentially enhanced coordination. |
| Medications | Symptomatic medications to address other MS symptoms that might contribute to proprioceptive deficits. | Reduced overall symptom burden, improving patient function and participation. |
Rehabilitation Strategies for Proprioception
Rehabilitating proprioception in Multiple Sclerosis (MS) is crucial for improving functional independence and quality of life. Proprioceptive deficits in MS often lead to instability, balance problems, and difficulties with fine motor skills. Targeted rehabilitation exercises can significantly improve these deficits and help individuals with MS maintain their independence.
Specific Proprioceptive Exercises for MS
Proprioceptive exercises for MS should be tailored to the individual’s specific needs and limitations. They should focus on restoring the body’s ability to sense its position and movement in space. These exercises should be performed under the guidance of a physical therapist experienced in working with individuals with MS. The exercises should progress gradually in difficulty and intensity, always ensuring the individual feels comfortable and safe.
Rationale Behind Exercise Design
The design of proprioceptive exercises for MS patients is based on principles of neuroplasticity. Exercises are carefully selected to stimulate and strengthen the neural pathways involved in proprioception. By repeatedly performing these exercises, the brain can re-establish and strengthen connections that were previously compromised. This process is often supported by other interventions, such as medication management and lifestyle modifications.
Examples of Proprioceptive Exercises
| Exercise | Proprioceptive Aspect Targeted | Description |
|---|---|---|
| Standing on one leg | Balance and single-limb proprioception | Patient stands on one leg, maintaining balance for a set duration, progressively increasing the duration as they improve. Variations can include eyes open/closed, using a support, and incorporating arm movements. |
| Heel-toe walking | Kinesthetic awareness and postural control | Patient walks along a line or a straight path, placing the heel of one foot directly in front of the toes of the other foot. This exercise improves awareness of limb positioning and coordination. |
| Proprioceptive exercises with resistance bands | Joint position sense and movement awareness | The patient uses resistance bands to perform various movements, such as arm curls, leg extensions, and rotations. The resistance provided by the bands helps in improving the sensory feedback during the movement. |
| Using a wobble board | Balance and dynamic stability | The patient stands on a wobble board, which is a unstable surface, and performs various movements like squats, lunges, and balance holds. This exercise targets both static and dynamic balance. |
| Blindfolded reaching tasks | Spatial awareness and hand-eye coordination | Patient reaches for objects or targets while blindfolded, relying solely on proprioceptive feedback. This helps to enhance the understanding of body position and movement in relation to the surrounding environment. |
Importance of Monitoring and Adjustments
Regular monitoring of the patient’s progress is essential for adapting the rehabilitation program. Progress may vary significantly from individual to individual, and adjustments need to be made as needed. The physical therapist should assess the patient’s responses to the exercises, making modifications to the intensity, duration, and type of exercise. This ensures that the exercises remain challenging enough to stimulate improvement but not so difficult as to cause pain or discouragement.
Careful monitoring helps to prevent potential setbacks and ensures the exercise regimen remains effective. This iterative process of evaluation and adaptation is key to a successful rehabilitation program.
Future Directions and Research
Unraveling the complexities of proprioceptive impairment in multiple sclerosis (MS) demands a proactive and multifaceted approach. Future research should focus on developing more effective assessment tools, therapies, and ultimately, treatments to mitigate the debilitating impact of these impairments on individuals with MS. The need for innovative strategies to address this significant issue is paramount.
Potential Areas for Future Research
Research into proprioceptive function in MS should encompass a broader range of methodologies and populations. The goal is to move beyond simply identifying the presence of deficits to understanding the underlying mechanisms and developing targeted interventions. This will involve examining the intricate interplay between neurological damage, sensory processing, and motor control in MS.
New Assessment Tools
Developing more sensitive and specific assessment tools is crucial for monitoring the progression of proprioceptive impairments in MS. Current methods often rely on subjective measures or have limitations in accurately quantifying subtle changes. Future research should explore the use of advanced technologies, such as advanced electromyography (EMG), functional magnetic resonance imaging (fMRI), and sophisticated motion tracking systems, to precisely measure and quantify proprioceptive deficits.
These technologies could potentially provide more objective and reliable data, facilitating earlier diagnosis and more precise monitoring of treatment effectiveness.
New Therapies for Proprioceptive Impairment
Innovative therapies targeting proprioceptive deficits in MS are needed to address the multifaceted nature of the problem. A combination of approaches may be necessary to effectively improve proprioceptive function, such as sensorimotor retraining, virtual reality-based exercises, and tailored sensory feedback interventions. For instance, studies could investigate the effectiveness of specific types of sensory feedback, such as vibrotactile stimulation, or specific forms of movement practice, like rhythmic auditory stimulation, in enhancing proprioceptive performance.
Developing Effective Treatments
The development of effective treatments for proprioceptive impairments in MS is a critical area for future research. The long-term goal is to design therapies that can reverse or slow the progression of these impairments. Research should explore the potential of pharmacological interventions, such as those targeting neural plasticity and regeneration, to address the underlying neurobiological mechanisms of proprioceptive loss.
This includes investigating the role of neurotrophic factors, which promote neuronal survival and growth, in potentially restoring proprioceptive function.
Importance of Multidisciplinary Research
Future research in this area should strongly emphasize multidisciplinary collaboration. Neurologists, physical therapists, occupational therapists, neuroscientists, and engineers should work together to develop comprehensive strategies for assessing and managing proprioceptive impairments in MS. This collaborative approach will ensure that research findings are effectively translated into practical clinical applications and therapies.
Illustrative Case Studies
Understanding the impact of multiple sclerosis (MS) on proprioception requires examining real-world examples. Case studies provide valuable insights into the symptoms, assessment methods, and interventions used to manage this sensory challenge. They highlight the diverse ways MS affects individuals and demonstrate the importance of personalized rehabilitation strategies.
Case Study 1: Impact of MS on Proprioception
This case study focuses on a 35-year-old female diagnosed with relapsing-remitting MS approximately five years prior. Her initial symptoms included fatigue and occasional numbness in her extremities. Over time, she experienced increasing difficulty with balance and coordination. She often stumbled or felt unsteady, particularly when walking or turning.
- Symptoms: The patient reported a progressive loss of awareness of limb position, especially in her lower extremities. She described a feeling of “unsteadiness” and “heaviness” in her legs, leading to frequent falls. She also noticed decreased ability to judge distances and difficulty with fine motor tasks, such as buttoning her shirt.
- Assessment: A comprehensive assessment included clinical observations, neurological examinations, and specific proprioceptive tests. The tests evaluated her ability to sense limb position and movement in different body parts. These tests indicated significant impairment in her proprioception, especially in the lower extremities. Additional tests explored gait patterns, balance, and coordination, revealing gait instability and a wide base of support during walking.
These results, coupled with her MS diagnosis, confirmed the link between the neurological condition and the proprioceptive deficits.
- Interventions: The rehabilitation program focused on improving proprioceptive function through targeted exercises and sensory stimulation. This included exercises to enhance awareness of limb position, such as standing on one leg and performing balance drills. Visual and auditory cues were used to aid her in regaining awareness. The therapy also included strengthening exercises for the core and lower extremities to improve stability and reduce the risk of falls.
Furthermore, assistive devices, such as canes or walkers, were considered to provide support during mobility activities. A multidisciplinary approach was adopted, including physiotherapy, occupational therapy, and medication management.
Case Study 2: Proprioception Rehabilitation
This case study highlights a 48-year-old male with MS who presented with severe proprioceptive deficits in both upper and lower extremities. He had experienced a progressive decline in his ability to perform activities of daily living, such as dressing and eating, due to impaired hand-eye coordination and balance issues.
- Rehabilitation Program: A tailored rehabilitation program was implemented to address his specific needs. The program focused on a combination of proprioceptive exercises, such as weighted vest exercises, proprioceptive neuromuscular facilitation (PNF) techniques, and balance training on unstable surfaces like foam pads or wobble boards. These exercises aimed to retrain the nervous system to process proprioceptive input more effectively.
The program was structured to gradually increase the difficulty and challenge to promote neuroplasticity.
- Outcome: After six months of intensive therapy, significant improvements were observed in his proprioceptive abilities. He demonstrated increased awareness of limb position, improved balance, and enhanced coordination. These improvements allowed him to perform activities of daily living more independently and confidently. He reported a noticeable decrease in falls and an increase in his overall quality of life.
Regular follow-up sessions were scheduled to monitor progress and adapt the program as needed.
- Lessons Learned: This case highlights the importance of individualized and tailored rehabilitation programs for individuals with MS. Early intervention and consistent therapy are crucial for maximizing functional outcomes. The program’s success demonstrates the potential for neuroplasticity to improve proprioceptive function, even in individuals with significant MS-related impairments. It also emphasizes the significance of incorporating patient feedback and preferences into the rehabilitation process.
Last Point: Proprioception In Multiple Sclerosis
In conclusion, proprioception in multiple sclerosis is a multifaceted issue that significantly affects a person’s ability to function. This exploration has highlighted the neural mechanisms involved, the diverse symptoms experienced, and the importance of personalized assessment and rehabilitation strategies. Further research and development in assessment tools and therapies are crucial for improving the lives of individuals living with MS and proprioceptive impairments.
We’ve covered a lot of ground, and hopefully, this has shed light on a crucial aspect of MS management.