Pcr vs rapid test for covid 19 – PCR vs rapid test for COVID-19: Understanding the nuances of these two testing methods is crucial for accurate diagnosis and effective public health management. Both PCR and rapid antigen tests play vital roles in identifying COVID-19, but they differ significantly in their methodology, accuracy, and practical applications. This exploration delves into the intricacies of each test, examining their steps, strengths, weaknesses, and ultimately, their optimal use cases.
This in-depth comparison will cover the scientific principles behind each test, providing a clear picture of their capabilities and limitations. We’ll also examine the factors influencing their cost, accessibility, and ethical implications. From sample collection to result interpretation, we’ll dissect the entire process, equipping you with a comprehensive understanding of PCR and rapid antigen tests in the context of COVID-19 diagnosis.
Introduction to COVID-19 Testing Methods
Rapid and accurate COVID-19 testing is crucial for effective disease management and containment. It allows for timely identification of infected individuals, enabling isolation and preventing further transmission. Different testing methods provide varying levels of speed, sensitivity, and specificity, making informed choices vital for public health interventions.The two most common methods for COVID-19 testing are Polymerase Chain Reaction (PCR) and rapid antigen tests.
Both play distinct roles in the diagnostic process, with PCR offering high sensitivity for detecting the virus’s genetic material and rapid antigen tests providing faster results, though with potential limitations in sensitivity. Understanding the underlying principles and methodologies of each test is essential for appreciating their respective strengths and weaknesses.
Quick COVID-19 tests like PCR and rapid tests are important tools, but understanding their differences is key. While a PCR test is more accurate for confirming infections, rapid tests are helpful for quick results. Knowing the nuances of these tests can be vital, just as understanding the uses of a total thyroxine test, like diagnosing thyroid issues, is crucial for overall health.
To learn more about the different applications of the total thyroxine test, check out this helpful resource: total thyroxine test uses. Ultimately, choosing the right test depends on the specific situation, and both PCR and rapid tests play a role in managing the COVID-19 pandemic.
General Principles of PCR Testing
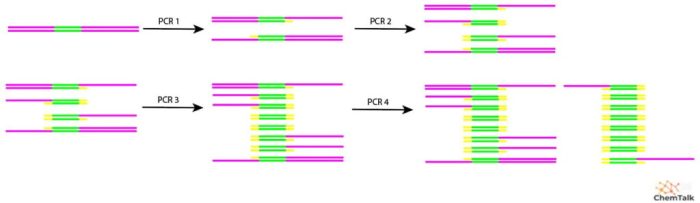
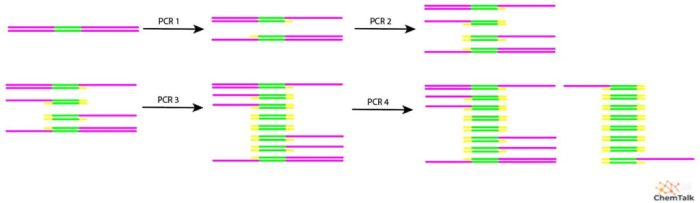
PCR tests detect the presence of viral RNA by amplifying specific genetic material of the virus. This process involves multiple cycles of heating and cooling, allowing for exponential duplication of the target DNA sequence. The amplified material is then detected, confirming the presence of the virus. This high sensitivity makes PCR a gold standard for diagnosing COVID-19.
The amplification process significantly increases the detectable amount of viral genetic material, thus improving the test’s ability to identify even low viral loads.
General Principles of Rapid Antigen Testing
Rapid antigen tests detect specific proteins of the virus. These tests use antibodies to bind to the viral proteins, forming a complex that is visually detected. The visual confirmation of this complex indicates the presence of the virus. This approach, though faster than PCR, is generally less sensitive and can yield false negatives, especially in individuals with low viral loads.
Comparison of Methodologies
| Characteristic | PCR Test | Rapid Antigen Test |
|---|---|---|
| Method | Detects viral RNA (genetic material) through amplification | Detects viral proteins (antigens) using antibodies |
| Sensitivity | High, capable of detecting low viral loads | Lower, may miss infections with low viral loads |
| Specificity | Generally high | Potentially lower, may produce false positives |
| Speed | Slower, typically 1-3 days | Faster, results available within 15-30 minutes |
| Cost | Generally higher per test | Generally lower per test |
| Equipment Requirements | Specialized laboratory equipment and trained personnel | Relatively simpler equipment and less technical expertise |
The table above summarizes the key distinctions between PCR and rapid antigen tests, highlighting their differing characteristics.
Practical Implications of the Differences
The different methodologies translate into different practical applications. PCR testing is often used for initial diagnosis, particularly in outbreaks, or when high sensitivity is critical. Rapid antigen tests, on the other hand, are well-suited for point-of-care testing, such as in community settings, or for screening large populations. The choice of test depends on the specific needs of the testing scenario, taking into account factors like speed, sensitivity, and cost.
For example, in a large-scale community screening, rapid antigen tests might be preferable due to their speed and lower cost, while PCR tests might be required for confirming suspected cases identified through initial screening.
PCR Test Details

The Polymerase Chain Reaction (PCR) test is a powerful diagnostic tool for detecting the presence of viral genetic material, including COVID-19. It works by amplifying a specific segment of the virus’s DNA or RNA, allowing for its detection even when present in small quantities. This method is highly sensitive and specific, making it a crucial tool in identifying and managing outbreaks.PCR tests are more complex than rapid antigen tests, requiring specialized laboratory equipment and trained personnel.
However, this complexity yields a highly accurate result, playing a critical role in confirming diagnoses and guiding public health strategies.
Sample Collection and Preparation
Proper sample collection is paramount for accurate PCR results. Nasopharyngeal swabs are frequently used to collect samples from the back of the nose and throat. This area is rich in viral particles, increasing the likelihood of a positive result. Saliva samples are also sometimes used, though they might require specific collection and processing techniques to ensure optimal yield.
The collected sample is then transported to the laboratory for processing. Proper preservation of the sample and adherence to strict handling protocols are crucial to maintain the integrity of the genetic material.
Nucleic Acid Amplification
The core principle of PCR is nucleic acid amplification. This process involves repeatedly copying a specific DNA or RNA segment, exponentially increasing its amount. This amplification allows scientists to detect the presence of the target genetic material even when it’s present in extremely small quantities. The repeated cycles of heating and cooling denature and copy the target sequence.
This process is controlled by specialized reagents and thermal cyclers.
PCR Steps: A Detailed Overview
- Sample Collection: A sample is collected from the patient using a nasopharyngeal swab, oropharyngeal swab, or saliva collection kit. The sample is then transported to the lab.
- Extraction: The collected sample is processed to isolate the viral genetic material (RNA). This often involves lysing the cells to release the RNA and then separating it from other cellular components.
- Reverse Transcription (if needed): If the target is RNA (like in COVID-19), a process called reverse transcription converts it into complementary DNA (cDNA). This step is necessary before PCR amplification.
- PCR Amplification: This is the core process where the target DNA sequence is copied many times. The process involves repeated cycles of heating and cooling (denaturation, annealing, and extension) to separate the DNA strands, bind primers to the target sequence, and synthesize new DNA strands.
- Detection: After multiple cycles, the amplified DNA product is detected. This is often done using gel electrophoresis, which separates the DNA fragments based on size, or by fluorescence detection methods. The presence or absence of the amplified product indicates whether the virus is present.
- Result Interpretation: A positive result indicates the presence of the virus, while a negative result indicates its absence. The results are typically reported within a few hours to a few days depending on the laboratory’s capacity and protocols.
Sensitivity and Specificity
PCR tests are renowned for their high sensitivity, meaning they can detect even minute amounts of the virus’s genetic material. This high sensitivity is essential for early diagnosis, particularly in cases where the viral load is low. However, the sensitivity is not absolute, and false negatives can occur. Specificity refers to the test’s ability to accurately identify the target virus.
High specificity minimizes false positives, ensuring the test identifies only the intended target and not other similar genetic sequences.
Figuring out PCR vs. rapid tests for COVID-19 can be tricky, right? While I’m no expert, I’ve been doing some research and it seems like PCR tests are often more accurate, but rapid tests are quicker. Interestingly, the debate about whether pineapple aids in weight loss is quite similar to understanding these tests – is pineapple good for weight loss is a complex question with no easy answer.
Ultimately, both PCR and rapid tests have their strengths and weaknesses, and knowing the difference is key to staying informed.
Equipment and Materials
PCR testing relies on specialized equipment and materials. These include:
- Thermal Cyclers: These machines precisely control the temperature changes needed for the PCR reaction. Different types of thermal cyclers exist, each with its own capacity and features.
- Pipettes and Micropipettes: These tools are used to precisely measure and dispense reagents and samples in small volumes.
- Centrifuges: These devices spin samples to separate components, facilitating the isolation of the desired material.
- Reagents: Specialized reagents, including DNA polymerase, primers, and nucleotides, are essential for the PCR process. The specific reagents used are optimized for the target virus and the chosen testing method.
- Labware: A variety of labware, including tubes, plates, and other containers, are necessary for sample handling and processing.
Types of PCR Tests
Different types of PCR tests exist, each with its own advantages and disadvantages.
| Type of PCR Test | Description |
|---|---|
| Real-time PCR (qPCR) | Detects the amplified product as it is generated, providing faster results. |
| Conventional PCR | Amplifies the target DNA, followed by detection using gel electrophoresis. |
| Reverse Transcription PCR (RT-PCR) | Specifically designed to detect RNA viruses, like COVID-19, by converting the RNA to DNA before amplification. |
Rapid Antigen Test Details: Pcr Vs Rapid Test For Covid 19
Rapid antigen tests for COVID-19 are a crucial tool in the fight against the pandemic, providing quick results to aid in identifying and isolating infected individuals. These tests, unlike PCR tests, offer results within minutes, making them ideal for screening large populations or when a rapid response is needed. Understanding the process, advantages, and disadvantages of these tests is vital for informed decision-making.
Sample Collection Process
The process of collecting a sample for a rapid antigen test is relatively straightforward and non-invasive. A swab is typically used to collect a nasal or throat sample, similar to the procedure used for PCR testing. The collected sample is then placed onto a test device, where it interacts with reagents designed to detect specific viral antigens.
Result Interpretation
Interpreting the results of a rapid antigen test involves observing the presence or absence of a colored line or lines on the test device. A positive result typically shows two distinct lines, while a negative result will show only one. It’s important to note that false negative results can occur, particularly if the viral load is low or the test is performed too early in the infection cycle.
Conversely, false positive results are also possible, often due to cross-reactivity with other respiratory viruses. Thus, a negative result does not definitively rule out infection, and a positive result should be confirmed with a PCR test.
Advantages of Rapid Antigen Tests
Rapid antigen tests offer several key advantages over PCR tests. The most significant advantage is their speed; results are typically available within 15-30 minutes. This rapid turnaround time allows for quicker isolation and contact tracing, minimizing the potential for further transmission. Additionally, rapid antigen tests are often less expensive than PCR tests, making them more accessible for widespread screening in various settings, such as schools, workplaces, and community events.
Disadvantages of Rapid Antigen Tests
Despite their advantages, rapid antigen tests have certain limitations. One significant drawback is their potential for false-negative results, especially in individuals with low viral loads. This can lead to missed diagnoses and potentially contribute to continued transmission. Furthermore, the accuracy of rapid antigen tests can vary depending on the specific test kit and the individual’s viral load.
Role of Antibodies in Rapid Antigen Tests
Antibodies are not directly used in rapid antigen tests. Instead, these tests detect viral antigens, which are fragments of the virus itself. Antibodies are produced by the body’s immune system in response to an infection, but they are not a component of the testing process. The rapid antigen test directly detects the presence of viral particles.
Equipment and Materials Used
The equipment and materials used in rapid antigen tests are generally simple and portable. These include a swab for sample collection, a test device containing reagents, and a method for observing the results (usually a visual indicator). Test devices typically come with instructions for proper use and interpretation of results.
Comparison of Turnaround Time
| Test Type | Turnaround Time (Approximate) |
|---|---|
| PCR Test | 1-3 days |
| Rapid Antigen Test | 15-30 minutes |
This table highlights the significant difference in turnaround time between PCR and rapid antigen tests. The quick turnaround of rapid antigen tests is a major benefit in various settings, allowing for timely interventions.
Accuracy and Reliability
COVID-19 testing methods, particularly PCR and rapid antigen tests, play a crucial role in managing the pandemic. Understanding their accuracy and reliability is essential for making informed decisions regarding diagnosis, treatment, and public health measures. This section delves into the comparative accuracy of these tests, exploring potential sources of error and limitations in each approach.
Comparing PCR and Rapid Antigen Test Accuracy
PCR tests are considered the gold standard for COVID-19 detection. They are highly sensitive, meaning they can detect even low viral loads, which often correlates with early stages of infection. Rapid antigen tests, on the other hand, are quicker and less expensive but less sensitive. They primarily detect the presence of viral proteins on the surface of the virus, and are typically used for initial screening or confirmation in specific scenarios.
Factors Affecting PCR Test Accuracy
Several factors can influence the accuracy of PCR tests. Sample collection technique, the time elapsed between infection and testing, and the quality of the laboratory equipment and reagents are all important considerations. Errors in sample handling or storage, for instance, can lead to inaccurate results. Furthermore, the presence of other respiratory viruses or infections can sometimes complicate the analysis and lead to false positives.
Finally, variations in laboratory procedures and personnel training can also contribute to discrepancies in results.
Factors Affecting Rapid Antigen Test Accuracy
Rapid antigen tests are also susceptible to various factors affecting their accuracy. The sensitivity of the test kit itself varies, and this directly influences its ability to detect the virus. Sample collection technique and proper reagent mixing are critical for accurate results. Furthermore, the viral load at the time of testing can significantly impact the test’s outcome.
If the viral load is too low, the test may produce a false negative result. Finally, the individual performing the test needs to follow the manufacturer’s instructions carefully to avoid errors.
Potential Sources of Error in PCR Testing
Potential errors in PCR testing can stem from several sources. Errors in sample collection, such as contamination or insufficient sample volume, can lead to false results. Issues with the reagents or equipment used in the laboratory can also affect the accuracy of the test. Poor laboratory practices, like inadequate handling of samples, improper temperature control, or errors in the PCR amplification process can also yield inaccurate outcomes.
In some cases, the presence of other pathogens or high viral loads can lead to false positives or negatives.
Potential Sources of Error in Rapid Antigen Testing
Rapid antigen tests are susceptible to errors in sample collection, similar to PCR tests. Additionally, the time elapsed between infection and testing, along with the specific viral load, can impact the test’s ability to detect the virus. The test itself may have limitations in detecting certain strains or variants of the virus, and the accuracy of the test can vary between manufacturers.
Furthermore, the user performing the test needs to adhere to the instructions meticulously to prevent errors.
Limitations of PCR Testing
PCR tests, while highly sensitive, have limitations. They are typically more expensive and require specialized laboratory equipment, which can sometimes limit their availability, especially in resource-constrained settings. The time required for processing can also be a factor, especially in situations requiring rapid results. Furthermore, false positives can occur due to the presence of other respiratory viruses.
Limitations of Rapid Antigen Testing
Rapid antigen tests are often less expensive and faster than PCR tests. However, they are less sensitive, meaning they might not detect low viral loads. This can lead to false negatives, especially in the early stages of infection or when viral loads are low. Another limitation is the need for careful training and adherence to the manufacturer’s instructions for accurate results.
Table of Common Errors in Test Interpretation
| Test Type | Error | Potential Cause |
|---|---|---|
| PCR | False Positive | Contamination, presence of other pathogens, laboratory error |
| PCR | False Negative | Insufficient sample, degraded sample, low viral load, improper procedure |
| Rapid Antigen | False Positive | Contamination, non-specific reactions, inadequate technique |
| Rapid Antigen | False Negative | Low viral load, improper sample handling, test expiry, inaccurate reading |
Test Use Cases and Applications
Choosing the right COVID-19 test depends heavily on the specific situation and desired outcome. A PCR test offers superior sensitivity, detecting even low viral loads, while rapid antigen tests provide faster results, albeit with a lower sensitivity. Understanding these nuances is crucial for appropriate application in various contexts.
PCR Test Preferences
PCR tests are generally the gold standard for confirming COVID-19 diagnoses, especially in situations requiring high sensitivity and accuracy. They are invaluable in epidemiological studies, where large-scale surveillance is critical to track virus spread and identify potential outbreaks.
- High-risk settings: PCR testing is the preferred method in hospitals, nursing homes, and other high-risk environments. Early detection in these settings can prevent further transmission and facilitate timely isolation and treatment. For instance, if a patient presents with severe respiratory symptoms and a history of exposure, a PCR test can confirm the diagnosis and allow for appropriate isolation and treatment.
- Suspected exposure, even if asymptomatic: In cases of suspected exposure, even without noticeable symptoms, PCR testing is often the preferred method to identify infection early. This proactive approach helps in reducing transmission chains, particularly in communities with high infection rates or potential exposure to contagious individuals.
- Investigating outbreaks: PCR tests are essential for tracing the source and spread of outbreaks. This involves testing individuals who have been in contact with confirmed cases to prevent further community transmission. The high sensitivity of PCR allows for identification of even those individuals who may not exhibit symptoms, and therefore may be unknowingly spreading the virus.
- Research purposes: PCR tests play a critical role in research studies related to COVID-19. The ability to detect minute quantities of viral RNA provides crucial data for understanding viral evolution, transmission dynamics, and the development of effective treatments.
Rapid Antigen Test Preferences
Rapid antigen tests offer a faster turnaround time, making them ideal for situations where a quick result is paramount. They are valuable for screening large populations, providing immediate guidance for isolation and contact tracing.
- Mass screenings: Rapid antigen tests are highly suitable for large-scale screenings in schools, workplaces, or community events. The speed of results enables rapid response measures like isolation and contact tracing, minimizing potential transmission.
- Self-testing: Rapid antigen tests are increasingly popular for self-testing, enabling individuals to quickly assess their infection status. This can be crucial for managing personal health and minimizing the risk of transmission to others, particularly in situations where access to healthcare facilities might be limited or delayed.
- Routine monitoring of individuals with mild symptoms: Rapid antigen tests can be used to monitor individuals with mild symptoms. The speed of results enables a quicker decision-making process regarding isolation and treatment options. This can help prevent the spread of infection and potentially allow individuals to avoid unnecessary hospitalizations.
- Screening for asymptomatic individuals: Rapid antigen tests can effectively screen individuals who might be asymptomatic carriers of the virus. This can be particularly important in community settings, allowing for proactive measures to mitigate transmission risks.
Optimal Use in Different Clinical Scenarios
The optimal testing strategy often involves a combination of PCR and rapid antigen tests, depending on the specific clinical scenario.
The choice between PCR and rapid antigen tests depends on the clinical context and the desired outcome. For instance, a rapid antigen test can provide a preliminary assessment, followed by a PCR test for confirmation, especially in cases of suspected infection or outbreaks. This dual approach allows for a faster response to potential outbreaks while maintaining the high accuracy of PCR.
Comparison for Various Populations
The choice of testing method can differ based on the population being screened. For example, in a school setting, rapid antigen tests might be suitable for mass screening, providing quick results for managing classroom situations. However, in a healthcare setting, PCR tests remain crucial for confirming diagnoses and managing patients with severe symptoms.
| Situation | Most Suitable Testing Method | Rationale |
|---|---|---|
| Mass screening in a community setting | Rapid Antigen Test | Speed and efficiency for large-scale screening |
| Suspected infection in a hospital setting | PCR Test | High sensitivity for confirming diagnosis and managing severe cases |
| Contact tracing after an outbreak | PCR Test | High sensitivity for identifying asymptomatic cases |
| Self-monitoring at home | Rapid Antigen Test | Accessibility and speed for individual assessment |
Cost and Accessibility
COVID-19 testing has become a crucial part of public health strategies, and understanding the associated costs and accessibility is vital for effective implementation. Different testing methods, such as PCR and rapid antigen tests, present varying price points and availability, influencing their suitability in diverse settings.The cost of testing, coupled with the logistical considerations of deploying and managing the tests, greatly impacts the overall strategy for controlling the spread of the virus.
Accessibility, in terms of both physical location and affordability, plays a significant role in ensuring equitable access to testing for all populations.
Cost Comparison
Factors like reagent costs, infrastructure needs, and personnel training significantly affect the price of PCR and rapid antigen tests. The cost-effectiveness of each test varies based on the specific context and goals.
- PCR tests, while often more accurate, generally involve a higher upfront cost due to more complex laboratory procedures. Reagents, specialized equipment, and trained personnel contribute to this higher price point. This increased complexity also leads to longer turnaround times for results, potentially impacting public health interventions.
- Rapid antigen tests, on the other hand, are typically more affordable and quicker to administer. The simpler procedures and readily available reagents translate to a lower cost per test. However, the reduced cost often comes at the expense of sensitivity, making them less suitable for all situations. Faster results, however, can expedite contact tracing and isolation protocols.
Accessibility Considerations
The availability of COVID-19 testing methods varies significantly based on factors such as geographic location, healthcare infrastructure, and policy decisions.
- Access to PCR testing is generally higher in areas with well-developed healthcare systems. The presence of well-equipped laboratories and trained personnel ensures reliable testing capabilities. However, remote areas or regions with limited resources may face challenges in obtaining PCR testing. High demand in some areas can also lead to shortages.
- Rapid antigen tests, being simpler and cheaper to administer, are more readily available in diverse settings, including community testing centers and even at home. This broader accessibility is particularly advantageous in regions with limited laboratory infrastructure, where rapid antigen testing can provide a critical early warning system.
Influencing Factors
Various factors contribute to the cost and accessibility of COVID-19 tests.
Figuring out the best COVID-19 test, PCR versus rapid, can be tricky. While rapid tests are convenient, PCR tests are often more accurate, especially for early detection. Interestingly, similar diagnostic challenges exist when assessing potential heart abnormalities in fibromyalgia, a condition often accompanied by various symptoms. Understanding the nuances of these tests, like exploring heart abnormalities in fibromyalgia , is key for informed decisions, whether it’s about COVID-19 or other potential health concerns.
Ultimately, both PCR and rapid tests have their pros and cons, and the choice often depends on individual needs and circumstances.
- Reagent costs are a key factor. Fluctuations in reagent prices can impact the overall cost of tests. Global supply chain issues, for example, can lead to price volatility. The availability and cost of reagents for PCR and rapid antigen tests can vary significantly.
- Infrastructure requirements play a crucial role. PCR testing necessitates well-equipped laboratories and trained personnel, which can be costly to establish and maintain. In contrast, rapid antigen tests often require less sophisticated infrastructure and training, leading to a lower cost for implementation.
- Government policies and funding also influence test accessibility. Government subsidies, insurance coverage, and public health initiatives can make testing more affordable and accessible to the public. Strategic allocation of resources and policies aimed at improving testing access are crucial.
Logistical Considerations
Implementing and managing both PCR and rapid antigen testing methods involve unique logistical considerations.
- For PCR tests, logistics involve sample collection, transportation to the laboratory, processing, and reporting results. These steps require a well-organized system to ensure timely and accurate results.
- Rapid antigen tests, being easier to administer, involve less complex logistics. However, efficient distribution channels and training for healthcare workers are still critical to their successful implementation.
Comparative Cost-Effectiveness
The table below summarizes the comparative cost-effectiveness of PCR and rapid antigen tests, considering various factors.
| Characteristic | PCR Test | Rapid Antigen Test |
|---|---|---|
| Accuracy | High | Moderate |
| Cost per test | Higher | Lower |
| Turnaround time | Longer | Shorter |
| Accessibility | Higher in well-resourced areas | Broader, more accessible |
| Infrastructure needs | Higher | Lower |
Ethical Considerations and Public Health Impact
COVID-19 testing has had a profound impact on public health, but its implementation raises critical ethical considerations. Ensuring equitable access to testing, particularly for vulnerable populations, is paramount. The differing characteristics of PCR and rapid antigen tests further complicate the ethical landscape, as their varied accuracy and accessibility necessitate nuanced approaches.The widespread adoption of testing has fundamentally reshaped public health strategies, from contact tracing to quarantine protocols.
The societal effects of these strategies, however, are not always uniform and can exacerbate existing inequalities. Understanding the implications of these tests for various populations and the broader public is essential for responsible implementation.
Ethical Considerations Regarding Access and Equity
Ensuring equitable access to COVID-19 testing is crucial for effective public health management. Disparities in access to testing based on socioeconomic status, geographic location, or other factors can perpetuate health inequities. For example, communities with limited access to healthcare infrastructure or those experiencing language barriers may face significant hurdles in obtaining necessary testing.
Impact of COVID-19 Testing on Public Health Outcomes, Pcr vs rapid test for covid 19
COVID-19 testing has significantly influenced public health outcomes. Early detection and isolation of infected individuals are crucial for controlling outbreaks. The availability and speed of testing directly affect the efficiency of contact tracing efforts, which in turn impact the rate of infection spread. For example, rapid testing can facilitate quicker identification of cases, enabling faster isolation and limiting transmission.
Implications of Widespread Use of Each Test Type
The widespread use of PCR and rapid antigen tests has had diverse implications. PCR testing, though highly accurate, can be more expensive and time-consuming. This often necessitates careful prioritization of testing resources, especially in resource-constrained settings. Rapid antigen tests, on the other hand, offer quicker results but have lower sensitivity, potentially leading to missed diagnoses and the continued spread of the virus.
Role of Testing in Controlling the Spread of COVID-19
Testing plays a vital role in controlling the spread of COVID-19. By identifying infected individuals, public health authorities can implement measures such as isolation and contact tracing to interrupt transmission chains. This proactive approach can reduce the overall burden of the disease and mitigate the strain on healthcare systems. A comprehensive testing strategy, combining PCR and rapid tests, can provide a more complete picture of infection rates and allow for targeted interventions.
Societal Effects of Differing Test Outcomes
Differing test outcomes can have significant societal effects. A false negative from a rapid antigen test could lead to continued transmission, while a false positive from a PCR test might cause unnecessary anxiety and isolation. The societal impact of these different results needs careful consideration. The availability and characteristics of testing options directly influence the experiences and perceptions of individuals and communities.
Future Trends in COVID-19 Testing
The landscape of COVID-19 testing is constantly evolving, driven by the need for faster, more accurate, and more accessible diagnostics. As the virus continues to mutate and new variants emerge, the field is adapting to meet these challenges. This evolution promises to significantly impact public health strategies and individual well-being.
Emerging Technologies
Future COVID-19 testing will likely incorporate advancements in point-of-care diagnostics. This shift toward rapid, decentralized testing will enhance the speed and efficiency of disease surveillance and response. Imagine a world where testing is available not just in clinics but also in pharmacies, schools, and even at home, providing near-instantaneous results. These technologies will be pivotal in containing outbreaks and facilitating timely interventions.
Improved Accuracy and Speed
The development of more sophisticated molecular diagnostic tools is anticipated. These advancements could potentially lead to even more accurate and faster detection of the virus, enabling quicker isolation and minimizing the spread of the disease. For example, advancements in polymerase chain reaction (PCR) technology could further refine the speed of results, making them available in hours rather than days.
Similarly, the refinement of rapid antigen tests promises even higher accuracy in identifying infected individuals.
Accessibility and Affordability
A key future trend will be the development of more accessible and affordable testing options. Lower costs and greater availability are crucial for widespread implementation, particularly in resource-limited settings. Innovations in test design and manufacturing will be instrumental in driving down the price of these crucial diagnostic tools. This includes exploring self-testing kits that are affordable and easy to use, facilitating widespread participation in surveillance programs.
Potential for Multiplexing
Future COVID-19 tests may incorporate multiplexing capabilities, allowing for the simultaneous detection of multiple pathogens or biomarkers. This capability will enable a broader understanding of disease dynamics, and potentially even allow for the identification of other potential respiratory illnesses. Imagine a test that can detect not only COVID-19 but also other viral infections, improving the efficiency of public health interventions.
Table Summarizing Future Directions of COVID-19 Testing
| Feature | Future Direction |
|---|---|
| Technology | Point-of-care diagnostics, improved PCR, refined rapid antigen tests, multiplex testing |
| Accuracy | Higher accuracy in detecting variants and multiple pathogens |
| Speed | Faster turnaround times, near-instantaneous results |
| Accessibility | More affordable and widely available testing options |
| Impact | Improved disease surveillance, faster response to outbreaks, better individual health management |
Concluding Remarks
In conclusion, choosing between PCR and rapid antigen tests for COVID-19 hinges on specific needs and circumstances. PCR, with its high accuracy, remains the gold standard for definitive diagnosis, especially in situations requiring high sensitivity. Rapid antigen tests, on the other hand, offer a faster turnaround time and are more convenient for widespread screening. Ultimately, a nuanced understanding of both methods, along with careful consideration of factors like cost, accessibility, and intended use, is crucial for effective COVID-19 management.