The history of surgery timeline sets the stage for this enthralling narrative, offering readers a glimpse into the evolution of surgical techniques throughout history. From ancient civilizations to modern marvels, this journey explores the incredible advancements, the courageous pioneers, and the constant quest for better healing. We’ll uncover the fascinating stories behind the development of…
How Often Should I Wash My Face? Your Guide
How often should I wash my face? This question plagues many, but the answer isn’t one-size-fits-all. Your skin type, daily activities, and even the environment play a crucial role in determining the ideal washing frequency. This guide delves into the factors affecting your face-washing routine, offering personalized insights for healthy skin. We’ll explore various skin…
Can I Keep Working with Fibromyalgia and CFS?
Can I keep working with fibromyalgia and CFS? This question is crucial for many, as these conditions can significantly impact daily life and work performance. This guide explores the complexities of maintaining employment while living with fibromyalgia (FM) and chronic fatigue syndrome (CFS), providing insights into understanding these conditions, exploring work options, managing symptoms, and…
Raw Honey vs Honey A Deep Dive
Raw honey vs honey – a seemingly simple comparison, yet one that reveals a fascinating world of flavor, nutrition, and processing. This exploration delves into the differences between raw and processed honey, examining their unique characteristics and highlighting the factors that contribute to their distinct qualities. We’ll unpack everything from the production methods to the…
Safe OTC Pain Relievers During Pregnancy
Safe OTC pain relievers to take while pregnant are crucial for managing discomfort during pregnancy. Each trimester brings unique aches and pains, from morning sickness to backaches and headaches. Choosing the right, safe over-the-counter medication is vital for both your well-being and the health of your developing baby. This guide will explore the different types…
Three Things to Do with Expired Condoms
Three things to do with expired condoms: Proper disposal, understanding the risks of use, and exploring safe alternatives. This post dives into the crucial aspects of handling expired condoms, from safe disposal methods to the potential risks and ethical considerations. We’ll also explore alternative contraceptive options and the environmental impact of improper disposal. Expired condoms,…
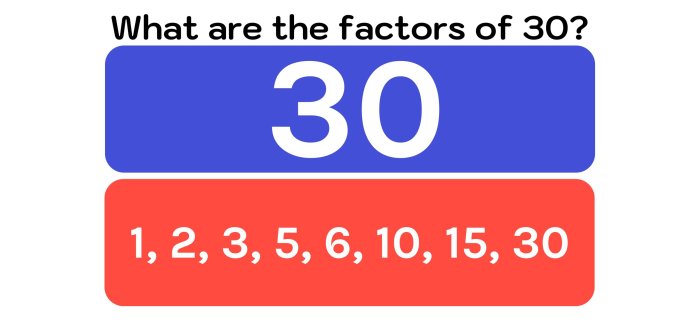
The 30 Most Prescribed Drugs in Pediatrics
The 30 most prescribed drugs in pediatrics play a crucial role in treating various childhood illnesses. Understanding the factors influencing these prescriptions, including dosage adjustments specific to children, is essential for optimal patient care. This exploration delves into the selection process, highlighting safety profiles, and examining the potential for drug interactions. We will also discuss…
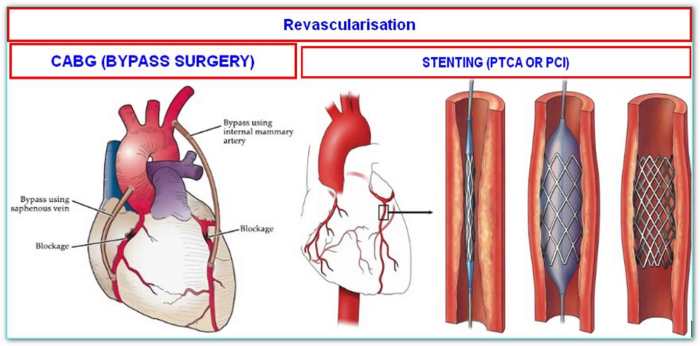
What is a Double Bypass Heart Surgery? A Comprehensive Guide
What is a double bypass heart surgery? This procedure, a significant step in cardiovascular care, aims to improve blood flow to the heart. It involves rerouting blood flow around blocked coronary arteries, often caused by atherosclerosis. Understanding the historical context, different types of bypasses, and the meticulous preparation and recovery process is crucial for patients…
Early Stage Toenail Fungus A Guide
Early stage toenail fungus is a common condition that often goes unnoticed in its initial stages. This guide dives into the specifics, from recognizing the early symptoms and causes to understanding preventative measures, diagnostic methods, and treatment options, including home remedies. We’ll explore everything from visual comparisons of healthy and infected nails to detailed tables…
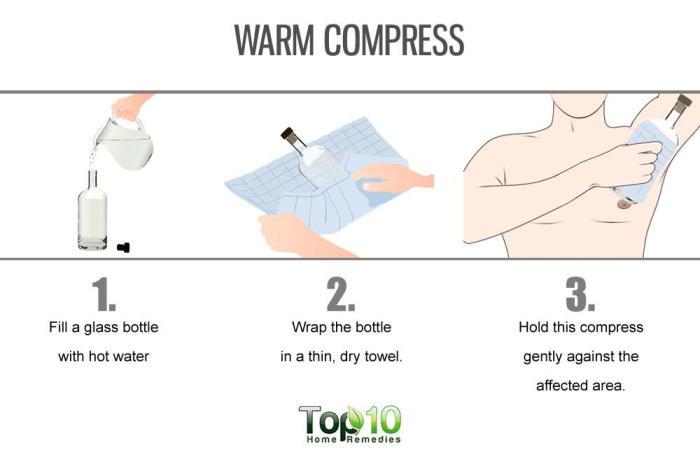
Hidradenitis Suppurativa Home Remedies A Guide
Hidradenitis suppurativa home remedies offer a potential path toward managing this chronic skin condition. This guide explores various approaches, from natural ingredients to lifestyle changes, to provide a comprehensive overview. We’ll delve into potential benefits and drawbacks, along with essential considerations before trying any home remedy. Understanding the nuances of Hidradenitis Suppurativa (HS) is crucial…