Cholesterol heart disease and African Americans is a complex issue with significant health disparities. This in-depth look examines the prevalence of high cholesterol, the contributing risk factors, and the impact of socioeconomic and genetic factors on heart disease within this community. We’ll explore the role of lifestyle choices, dietary influences, and cultural contexts, along with available diagnosis and treatment approaches.
The prevalence of high cholesterol in African Americans, coupled with unique socioeconomic factors and genetic predispositions, significantly increases their risk of heart disease. This analysis will unravel the intricate web of these contributing elements to offer a comprehensive understanding of the challenges and potential solutions.
Prevalence and Risk Factors
High cholesterol poses a significant health risk, particularly within the African American community. Understanding the prevalence of this condition, alongside the contributing factors, is crucial for developing targeted prevention and treatment strategies. This knowledge empowers individuals and healthcare providers to proactively address the issue.The prevalence of high cholesterol varies considerably across racial and ethnic groups. African Americans often experience a higher incidence of high cholesterol compared to other populations, contributing to a greater risk of developing heart disease.
This disparity highlights the need for tailored interventions to mitigate the impact of this health concern.
Prevalence of High Cholesterol
African Americans frequently exhibit higher rates of high cholesterol compared to other racial groups. This disparity may stem from a complex interplay of genetic predispositions, lifestyle choices, and socioeconomic factors. Data from the National Health and Nutrition Examination Survey (NHANES) consistently demonstrates this trend. Understanding the reasons behind these higher rates is essential for developing targeted interventions.
Contributing Risk Factors
Several factors contribute to the elevated prevalence of high cholesterol in African Americans. Socioeconomic factors play a role, as limited access to healthy foods, affordable healthcare, and opportunities for physical activity can influence dietary habits and lifestyle choices. Genetic predispositions may also contribute, as certain genetic variations may increase the risk of high cholesterol.
- Socioeconomic Factors: Limited access to healthy food options, affordable healthcare, and safe environments for physical activity can influence dietary habits and lifestyle choices, making it harder to adopt healthier behaviors. Financial constraints often dictate food choices, leading to diets higher in saturated and unhealthy fats.
- Lifestyle Choices: Dietary habits, particularly high intake of saturated and trans fats, are often linked to high cholesterol. Sedentary lifestyles and a lack of physical activity contribute to weight gain, further increasing the risk. Stress levels and lack of sleep can also negatively affect cholesterol levels.
- Genetic Predisposition: Certain genetic variations may increase the risk of high cholesterol. Family history of high cholesterol is a significant risk factor, as inherited genetic factors can influence lipid metabolism and cholesterol levels.
Incidence of Heart Disease
Heart disease carries a substantial burden within the African American community. The incidence of heart disease is often higher in African Americans compared to other racial groups, due to a combination of genetic predisposition, lifestyle factors, and socioeconomic factors. This disparity in heart disease incidence necessitates targeted interventions and public health initiatives.
Correlation between High Cholesterol and Heart Disease
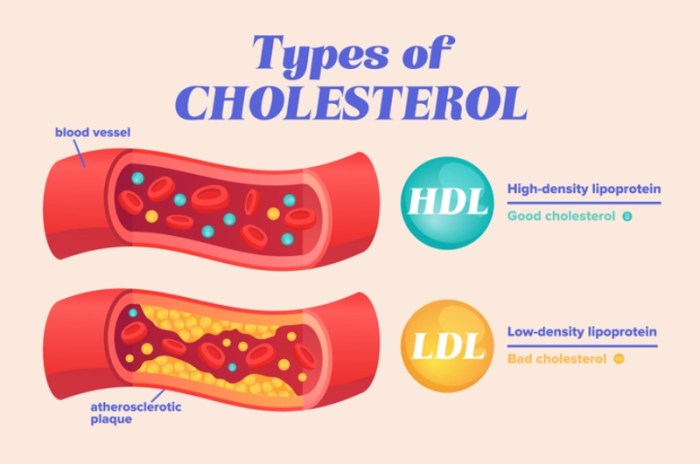
High cholesterol is a major risk factor for heart disease. High levels of cholesterol can lead to the buildup of plaque in the arteries, narrowing the vessels and potentially leading to heart attacks and strokes. This correlation underscores the importance of managing cholesterol levels to reduce the risk of heart disease.
Comparison of Prevalence, Risk Factors, and Heart Disease Incidence
| Racial Group | Prevalence of High Cholesterol | Risk Factors | Incidence of Heart Disease |
|---|---|---|---|
| African American | Higher than other groups | Socioeconomic factors, lifestyle choices, genetic predispositions | Higher than other groups |
| Caucasian | Lower than African American group | Socioeconomic factors, lifestyle choices, genetic predispositions | Lower than African American group |
| Hispanic | Varying rates depending on subgroups | Socioeconomic factors, lifestyle choices, genetic predispositions | Varying rates depending on subgroups |
Impact of Socioeconomic Factors
The stark reality of health disparities in the African American community often stems from deeply entrenched socioeconomic factors. These disparities, which extend beyond access to healthcare, create a complex web of challenges that significantly influence the prevalence of heart disease, specifically concerning cholesterol levels. Understanding these factors is crucial for developing targeted interventions and fostering equitable health outcomes.Socioeconomic factors play a pivotal role in shaping the health landscape for African Americans, creating barriers to accessing essential resources for heart health.
Limited access to nutritious food options, restricted opportunities for physical activity, and the compounding stress associated with poverty all contribute to elevated cholesterol levels and an increased risk of heart disease. This unequal playing field underscores the urgent need for comprehensive strategies that address these systemic issues.
Access to Healthcare
Limited access to quality healthcare, including preventative screenings and timely interventions for high cholesterol, disproportionately affects African Americans in lower socioeconomic groups. Insurance coverage gaps and geographic barriers to care create significant obstacles to receiving necessary medical attention. This lack of access often leads to delayed diagnosis and treatment, resulting in the progression of heart disease and its associated complications.
Healthy Food Options
The availability and affordability of healthy food options are often limited in communities with lower socioeconomic status. This lack of access can lead to dietary patterns rich in saturated and trans fats, contributing to elevated cholesterol levels. Supermarkets and grocery stores may be less prevalent in these areas, replaced by convenience stores offering less nutritious choices. This disparity significantly increases the risk of heart disease.
Physical Activity Opportunities
Restricted access to safe and affordable recreational facilities and the lack of accessible green spaces within these communities often limits opportunities for regular physical activity. This lack of physical activity is a significant factor in the development of high cholesterol and heart disease. Limited access to safe and enjoyable recreational activities directly impacts the ability to maintain a healthy weight and overall cardiovascular health.
Stress and Mental Health
The chronic stress associated with poverty, systemic racism, and discrimination can have a profound impact on cholesterol levels and heart health. High levels of stress can elevate cortisol, a hormone that can increase cholesterol production. This ongoing stress can also weaken the cardiovascular system, increasing susceptibility to heart disease. Mental health services are often inaccessible or less readily available in underserved communities.
High cholesterol and heart disease are serious concerns, especially for African Americans. While researching related factors, I stumbled upon some fascinating information about Crohn’s disease, a chronic inflammatory condition that can affect the digestive system. Learning about the specifics of Crohn’s disease from crohn s disease facts definitely broadened my understanding of health disparities. Ultimately, further research into the complex interplay between genetics, lifestyle, and environmental factors is crucial when exploring heart disease risks in African American communities.
Comparison of Preventative Care and Treatment
The ability to access preventative care and treatment options for heart disease varies significantly across different socioeconomic groups. Individuals with higher socioeconomic status often have greater access to advanced diagnostic tools, cutting-edge treatments, and comprehensive cardiac rehabilitation programs. Conversely, individuals in lower socioeconomic groups may face significant barriers to accessing these crucial resources, leading to poorer health outcomes.
Socioeconomic Factors, Access to Resources, and Impact on Cholesterol and Heart Health
| Socioeconomic Factor | Access to Resources | Impact on Cholesterol and Heart Health |
|---|---|---|
| Limited Income | Limited access to nutritious foods, less access to healthcare, fewer recreational opportunities. | Higher risk of unhealthy dietary habits, delayed diagnosis and treatment, reduced physical activity, increased stress levels, leading to elevated cholesterol and heart disease risk. |
| Lack of Insurance | Delayed or missed preventative screenings, limited access to treatment options. | Delayed diagnosis and treatment, leading to advanced stages of heart disease. |
| Limited Access to Healthy Foods | Greater reliance on processed foods high in saturated and trans fats. | Elevated cholesterol levels, increased risk of heart disease. |
| Limited Access to Physical Activity | Fewer safe and affordable recreational facilities, lack of accessible green spaces. | Reduced physical activity, contributing to weight gain, higher cholesterol, and increased risk of heart disease. |
| Chronic Stress | Limited access to mental health services, lack of support networks. | Increased cortisol levels, weakened cardiovascular system, elevated cholesterol, increased risk of heart disease. |
Genetic and Biological Factors

High cholesterol and its link to heart disease in African Americans are complex issues, influenced by a combination of genetic predispositions and biological factors. Understanding these factors is crucial for developing targeted prevention and treatment strategies. While lifestyle choices play a significant role, inherent biological differences can significantly impact cholesterol levels and increase the risk of heart disease.
Genetic Predispositions
Genetic variations can influence how the body processes cholesterol. Certain genes play a crucial role in regulating cholesterol production, absorption, and elimination. African Americans, like other racial groups, possess a diverse range of genetic variations. Some genetic predispositions might lead to higher levels of LDL (“bad”) cholesterol or lower levels of HDL (“good”) cholesterol. This can increase the risk of plaque buildup in arteries, ultimately leading to heart disease.
Research has identified specific genetic variants that are more prevalent in African Americans and associated with elevated cholesterol levels.
Biological Factors
Beyond genetics, biological differences in body composition, metabolism, and hormone levels can also influence cholesterol levels. Differences in body mass index (BMI) and distribution of fat can impact cholesterol profiles. Metabolism, the process of converting food into energy, can vary between individuals and populations, affecting how the body manages cholesterol. Furthermore, variations in hormone levels, such as insulin, can also contribute to altered cholesterol metabolism.
Comparison with Other Racial Groups
Studies comparing genetic and biological factors related to cholesterol and heart disease across racial groups highlight variations. While specific genes and their interactions might differ, the overarching principle remains: genetic predisposition and biological variations can influence cholesterol levels and heart disease risk in all populations. However, the specific genetic variants and their impact on cholesterol levels can differ significantly between racial groups.
Interaction of Genetics and Lifestyle
The interplay between genetic predispositions and lifestyle choices is critical in determining cholesterol levels and heart disease risk. Individuals with a genetic predisposition to high cholesterol may be more susceptible to developing the condition if they adopt unhealthy lifestyles, such as a poor diet and lack of physical activity. Conversely, a healthy lifestyle can mitigate the impact of genetic risk factors, reducing the risk of developing high cholesterol and heart disease.
Maintaining a healthy weight, consuming a balanced diet, and engaging in regular physical activity can help manage cholesterol levels regardless of genetic background.
Summary Table: Genetic Variations and Cholesterol Risk in African Americans
| Genetic Variation | Association with Cholesterol Levels | Association with Heart Disease Risk |
|---|---|---|
| APOE gene variants (e.g., APOE4) | Increased LDL cholesterol levels | Increased risk of coronary artery disease |
| Other genes related to lipid metabolism | Varied effects on cholesterol synthesis, absorption, and excretion | Potentially elevated risk of dyslipidemia and heart disease |
| Genes related to inflammation | Possible impact on inflammatory responses | Possible contribution to the development of atherosclerosis |
Note: This table is not exhaustive and represents a selection of potentially relevant genetic variations. Further research is continuously exploring the complex interactions between genes, lifestyle, and cardiovascular health.
Lifestyle and Dietary Influences: Cholesterol Heart Disease And African Americans
African Americans face a disproportionately high risk of heart disease, often linked to a complex interplay of genetic predisposition, socioeconomic factors, and lifestyle choices. Understanding the role of diet and nutrition, physical activity, and cultural influences is crucial for developing effective strategies to reduce this risk. Addressing these factors requires a nuanced approach that considers the unique cultural context and preferences of the community.A significant contributor to heart disease risk is an unhealthy diet often characterized by high saturated and trans fats, excessive sodium intake, and insufficient consumption of fruits, vegetables, and whole grains.
These dietary patterns are often exacerbated by limited access to healthy food options and a lack of nutrition education. In addition, physical inactivity further contributes to the problem, leading to weight gain and an increase in cholesterol levels. Recognizing the importance of these factors is vital to crafting effective preventive measures.
Dietary Recommendations for Lowering Cholesterol
A heart-healthy diet for African Americans emphasizes whole foods, lean proteins, and plenty of fruits and vegetables. Dietary cholesterol, though important to understand, is often less of a concern than saturated and trans fats in raising LDL cholesterol. Prioritizing foods rich in soluble fiber, such as oats, beans, and fruits, can help lower LDL cholesterol levels. Limiting processed foods, fast food, and sugary drinks is essential for reducing overall calorie intake and unhealthy fat consumption.
Specific Dietary Recommendations
- Prioritize whole grains over refined grains. Switching to whole-wheat bread, brown rice, and whole-grain cereals provides essential fiber and nutrients, contributing to better blood sugar control and reduced cholesterol levels. For example, replacing white bread with whole-wheat bread can significantly impact cholesterol levels over time.
- Increase intake of fruits and vegetables. Fruits and vegetables are excellent sources of vitamins, minerals, and antioxidants, which are crucial for overall health and contribute to lowering LDL cholesterol. Aim for a variety of colors, as different colored fruits and vegetables offer different nutritional benefits. For example, incorporating berries, leafy greens, and citrus fruits into the daily diet can significantly contribute to better cardiovascular health.
- Choose lean protein sources. Lean meats, poultry without skin, fish, beans, and lentils are preferable to red meat and processed meats. These options are lower in saturated fat and cholesterol, supporting heart health. For example, substituting ground beef with lean ground turkey or chicken can lower the overall fat intake in the diet.
- Limit saturated and trans fats. These fats raise LDL cholesterol levels, increasing the risk of heart disease. Saturated fats are found in animal products like red meat, whole milk, and butter, while trans fats are often present in processed foods and fried foods. Reducing these fats in the diet can significantly contribute to better heart health.
Impact of Physical Activity
Regular physical activity plays a vital role in managing cholesterol levels and reducing heart disease risk. Physical activity helps lower LDL cholesterol, raise HDL cholesterol, and maintain a healthy weight. For African Americans, incorporating physical activity into daily routines is crucial for overall health and disease prevention. Finding activities that are enjoyable and sustainable is key to long-term adherence.
High cholesterol and heart disease disproportionately affect African Americans. Taking proactive steps to manage your health is key, and that includes finding the right oral care routine. For example, a custom-fitted night guard for teeth can help protect your smile while you sleep, night guard for teeth the right fit is crucial for overall well-being.
Ultimately, understanding these connections empowers us to make better choices about our health, especially regarding heart health in the African American community.
For example, engaging in brisk walking, jogging, swimming, or dancing for at least 150 minutes per week can significantly improve cardiovascular health.
Cultural Factors Influencing Dietary Choices and Physical Activity
Cultural norms and traditions significantly influence dietary choices and physical activity levels. Family meals, social gatherings, and religious practices often revolve around specific foods and activities. Understanding these cultural factors is essential when developing culturally appropriate lifestyle interventions. For example, community-based programs that incorporate traditional dishes while emphasizing healthy preparation methods can be more effective than generalized dietary recommendations.
Tailoring Lifestyle Interventions
Effective lifestyle interventions must be tailored to the cultural context and preferences of African Americans. Interventions should consider the unique challenges and opportunities faced by the community, such as limited access to healthy food options, cultural preferences for certain foods, and social support networks. For example, providing culturally relevant cooking demonstrations and nutrition education workshops in community centers can empower individuals to make informed choices about their health.
Dietary Recommendations by Food Group
| Food Group | Examples | Cholesterol Content (mg/serving) | Impact on Heart Health |
|---|---|---|---|
| Fruits and Vegetables | Apples, bananas, spinach, broccoli | Low | High in fiber, vitamins, and minerals; promotes heart health. |
| Whole Grains | Brown rice, quinoa, whole-wheat bread | Moderate | High in fiber; helps lower LDL cholesterol. |
| Lean Proteins | Chicken breast, fish, beans, lentils | Moderate | Lower in saturated fat and cholesterol compared to red meat. |
| Dairy Products | Low-fat milk, yogurt | Moderate | Choose low-fat options to reduce saturated fat intake. |
| Fats and Oils | Olive oil, avocado oil | Low | Use in moderation; choose healthy unsaturated fats. |
Diagnosis and Treatment Approaches
High cholesterol and its associated heart disease pose significant risks for African Americans, often manifesting differently and requiring tailored approaches to diagnosis and treatment. Understanding the specific challenges faced by this population is crucial for effective intervention and improved health outcomes. Early detection and proactive management are paramount in mitigating the impact of these conditions.
Diagnostic Methods for High Cholesterol and Heart Disease
Accurate diagnosis is essential for effective treatment. African Americans may experience different cholesterol levels and heart disease symptoms compared to other populations. Therefore, comprehensive assessments are critical. This involves a thorough medical history, including family history of cardiovascular disease, physical examination, and appropriate blood tests to measure cholesterol levels (LDL, HDL, and triglycerides). Cardiovascular risk assessments, such as Framingham risk scores, are also important tools for evaluating individual risk factors.
High cholesterol and heart disease disproportionately affect African Americans. Understanding the complex interplay of genetics and lifestyle factors is key. Interestingly, conditions like congenital adrenal hyperplasia, which can affect hormone levels, can also sometimes impact cholesterol. Learning more about congenital adrenal hyperplasia symptoms can offer insight into potential underlying causes, helping us better address the heart health disparities within the African American community.
This deeper understanding is vital to developing targeted interventions and preventative strategies for this population.
These assessments consider multiple factors, including age, gender, blood pressure, smoking status, and cholesterol levels, to predict an individual’s likelihood of developing heart disease. Echocardiograms and other imaging techniques may be used to evaluate the structure and function of the heart.
Treatment Strategies for High Cholesterol
Effective treatment for high cholesterol and heart disease involves a multifaceted approach, encompassing lifestyle modifications and potentially medication. Addressing underlying risk factors, like diabetes and hypertension, is crucial. A balanced diet, regular exercise, and weight management are often the initial steps. These lifestyle changes can significantly reduce the risk of heart disease and improve overall health. For individuals who do not respond adequately to lifestyle modifications, medications may be necessary to control cholesterol levels.
Statins, for instance, are commonly prescribed to lower LDL cholesterol. Other medications, such as bile acid sequestrants, niacin, or fibrates, may be considered in specific situations. It is essential to note that treatment strategies must be individualized based on the patient’s specific condition and risk factors.
Importance of Early Detection and Intervention
Early detection and intervention are crucial in preventing heart disease. Prompt identification of high cholesterol and risk factors allows for timely intervention, preventing further progression of the disease and reducing the risk of serious cardiovascular events. Early interventions can include lifestyle modifications and, when necessary, medication, which can effectively slow or halt the progression of atherosclerosis and reduce the likelihood of heart attack or stroke.
Challenges in Diagnosis and Treatment
Disparities in access to healthcare and healthcare providers can pose significant challenges in diagnosis and treatment for African Americans. Limited access to preventive care, cultural and language barriers, and implicit bias in healthcare settings can affect the quality and timeliness of diagnosis and treatment. Addressing these disparities requires a multi-pronged approach involving community outreach programs, culturally competent healthcare providers, and improved access to affordable healthcare services.
Comparison of Treatment Options
| Treatment Option | Description | Medications | Dietary Recommendations | Lifestyle Modifications |
|---|---|---|---|---|
| Medication | Lowering cholesterol through prescribed medications. | Statins, bile acid sequestrants, niacin, fibrates | Following a diet low in saturated and trans fats. | Regular exercise and weight management. |
| Dietary Recommendations | Improving diet quality. | – | Increased intake of fruits, vegetables, and whole grains; reduced intake of processed foods and sugary drinks. | – |
| Lifestyle Modifications | Adopting healthier lifestyle choices. | – | – | Regular physical activity, stress management techniques, smoking cessation. |
Public Health Initiatives
Addressing the disproportionate burden of heart disease in African Americans requires multifaceted public health initiatives. These initiatives must go beyond simply providing information; they need to actively engage communities, address systemic inequities, and create sustainable, culturally relevant solutions. Successful programs recognize the interconnectedness of socioeconomic factors, lifestyle choices, and access to care in shaping heart health outcomes.Community-based programs play a crucial role in fostering a culture of health.
These programs must be designed with the input of the community, ensuring they are relevant and effective. They should incorporate culturally sensitive approaches, empowering individuals to make positive changes in their daily lives. Empowering communities through knowledge, resources, and support is key to long-term health improvements.
Community-Based Programs
Community-based programs are essential for promoting healthy lifestyle choices. These programs often include workshops, cooking demonstrations, and support groups. They can also incorporate health screenings and provide access to healthy food options. Examples include community gardens, cooking classes focusing on heart-healthy recipes, and mentorship programs connecting individuals with resources and support. These programs are vital for empowering communities and fostering a culture of health.
Improving Access to Preventative Care
Expanding access to preventative care is critical for early detection and intervention. This includes addressing barriers such as cost, transportation, and language. Strategies might include mobile health clinics, community health workers, and partnerships with local organizations to increase outreach and accessibility. By reducing these barriers, more individuals can access necessary preventative care.
Strategies for Improving Access to Treatment, Cholesterol heart disease and african americans
Ensuring access to appropriate and timely treatment is equally important. This includes providing financial assistance for medications and procedures, coordinating care across different healthcare providers, and developing culturally competent healthcare teams. Such measures can significantly improve outcomes for African Americans facing heart disease.
Future Research and Intervention
Further research is needed to identify the specific factors contributing to heart health disparities within African American communities. This research should investigate the complex interplay of socioeconomic factors, genetic predispositions, and lifestyle choices. Interventions should be tailored to address these specific factors and incorporate culturally appropriate strategies. For example, research on the impact of stress on heart health within specific cultural contexts could be beneficial.
Table of Public Health Initiatives
| Initiative | Target Population | Impact on Heart Health Outcomes |
|---|---|---|
| Community-Based Heart Health Workshops | African American adults and families | Increased knowledge about heart health, improved dietary habits, and elevated engagement in physical activity. |
| Mobile Health Clinics | African American individuals in underserved areas | Improved access to screenings, education, and basic preventative care. |
| Partnerships with Local Organizations | African American communities | Expanded access to resources and support networks. Community leaders, faith-based organizations, and local businesses can be instrumental in this. |
| Culturally Competent Healthcare Teams | African American patients | Enhanced trust, improved communication, and increased adherence to treatment plans. |
Closing Notes
In conclusion, the relationship between cholesterol, heart disease, and African Americans is multifaceted and deeply rooted in societal and biological factors. Addressing the disparities in access to healthcare, promoting healthy lifestyles, and implementing targeted public health initiatives are crucial to mitigating the impact of heart disease within this community. Continued research and proactive interventions are essential to fostering a healthier future for African Americans.