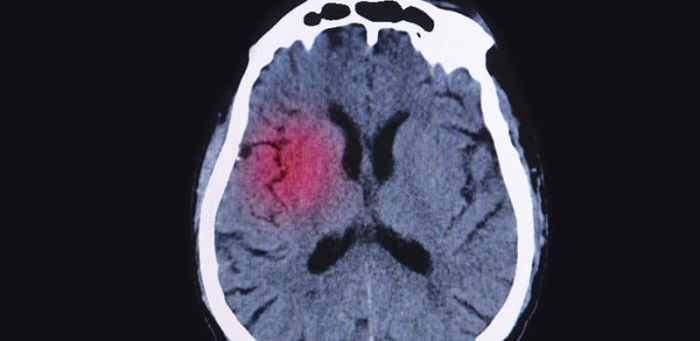
Migraine and multiple sclerosis connection: This exploration delves into the intriguing relationship between these two neurological conditions. Migraines, characterized by debilitating headaches, and multiple sclerosis, a chronic autoimmune disease affecting the central nervous system, often share overlapping symptoms. Understanding this connection is crucial for accurate diagnosis and effective treatment strategies.
The potential overlap in symptoms, triggers, and underlying mechanisms between migraines and multiple sclerosis presents significant challenges for healthcare professionals. This article examines the potential links, highlighting the challenges in diagnosis, and discussing potential treatment strategies and future research avenues. It will provide a clear comparison of symptoms and explore potential mechanisms behind the connection.
Introduction to Migraine and Multiple Sclerosis Connection
Migraine headaches are debilitating neurological disorders characterized by severe, throbbing head pain, often accompanied by nausea, vomiting, and sensitivity to light and sound. Multiple sclerosis (MS) is a chronic autoimmune disease affecting the central nervous system, leading to a wide range of neurological symptoms. While seemingly disparate, there’s growing evidence suggesting a potential connection between these two conditions.
This connection is complex and not fully understood, but research continues to shed light on the potential overlap in their underlying mechanisms and symptoms.Understanding this potential link is crucial for both diagnosis and treatment. Early identification of potential overlapping symptoms can lead to more effective management strategies for individuals experiencing both conditions. The following sections explore the common symptoms and potential shared triggers, as well as the challenges in diagnosis.
Common Symptoms of Migraine and MS
Migraine and MS share some overlapping symptoms, making it challenging to distinguish between the two in some cases. Both conditions can manifest as neurological dysfunction, affecting various parts of the body. Headaches, including migraines, are a frequently reported symptom of MS, while MS can also cause a range of neurological symptoms that mimic those of migraine, such as vision problems, fatigue, and cognitive impairment.
Comparing Migraine and MS Symptoms
The table below highlights the similarities and differences in symptoms, triggers, and diagnosis of migraine and MS.
| Feature | Migraine | Multiple Sclerosis |
|---|---|---|
| Symptoms | Severe, throbbing head pain, often on one side of the head; nausea, vomiting; sensitivity to light and sound; aura (visual disturbances, tingling, numbness) preceding the headache. | Varying symptoms, including numbness, tingling, vision problems, muscle weakness, balance issues, fatigue, cognitive difficulties, and pain. Symptoms can fluctuate and come and go. |
| Triggers | Stress, changes in sleep patterns, certain foods (e.g., aged cheeses, processed meats), caffeine withdrawal, hormonal fluctuations, weather changes. | Exact triggers are not fully understood, but factors like stress, infections, and environmental exposures are suspected. Genetic predisposition plays a role. |
| Diagnosis | Based on a thorough evaluation of headache history, physical examination, and sometimes diagnostic tests (e.g., brain imaging). No single test definitively confirms migraine. | Diagnosis involves a comprehensive evaluation, including neurological examination, medical history review, and often MRI scans of the brain and spinal cord to identify characteristic lesions. No single test definitively confirms MS. |
Potential Mechanisms of the Connection
The link between migraine and multiple sclerosis (MS) remains a complex and fascinating area of research. While the precise mechanisms connecting these two neurological disorders are not fully understood, several potential pathways are being explored. Understanding these potential mechanisms could lead to improved diagnostic tools and targeted therapies for both conditions.Exploring the underlying mechanisms of this connection is crucial to unraveling the shared pathophysiology and developing effective treatment strategies.
This exploration involves looking at the roles of inflammation, neurotransmitters, and the immune system, and the interplay of genetic and environmental factors.
Inflammation
Inflammation plays a significant role in both migraine and MS. Chronic inflammation in the central nervous system (CNS) is a hallmark of MS, and similar inflammatory processes have been observed in migraineurs. Studies suggest that the inflammatory response in the brain may trigger or exacerbate migraine attacks. This inflammatory response can involve the activation of immune cells, the release of pro-inflammatory cytokines, and the disruption of the blood-brain barrier.
Neurotransmitters
Neurotransmitters are chemical messengers in the nervous system that regulate various functions, including pain perception. Imbalances in neurotransmitter systems, such as serotonin, glutamate, and calcitonin gene-related peptide (CGRP), have been implicated in both migraine and MS. Disruptions in these systems may contribute to the development and progression of both conditions. For example, altered levels of serotonin have been observed in both migraine patients and those with MS, suggesting a potential shared pathway.
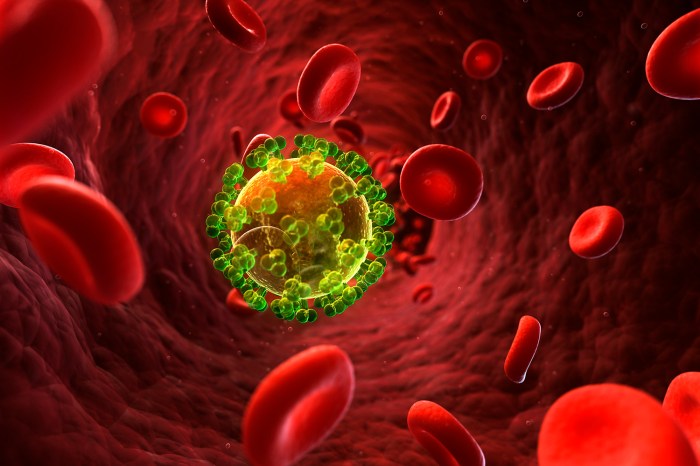
Immune System
The immune system plays a central role in MS, where the body’s own immune cells attack the myelin sheath surrounding nerve fibers. Some research suggests a possible link between immune system dysfunction and migraine, although the specific mechanisms are not fully understood. Immune system dysregulation could lead to the release of inflammatory molecules that contribute to migraine attacks.
This link is an active area of research, focusing on identifying specific immune pathways that may be involved.
Genetic and Environmental Factors
Genetic predisposition and environmental factors likely interact to influence the development of both migraine and MS. Individuals with a family history of either condition may be more susceptible. Environmental factors, such as infections, stress, and lifestyle choices, might also contribute to the onset or exacerbation of these disorders. The interplay of these factors is complex and warrants further investigation.
Table of Theories Explaining the Connection
| Theory | Mechanism | Evidence |
|---|---|---|
| Shared Inflammatory Pathways | Chronic inflammation in the CNS, potentially triggered by similar factors in both conditions, leading to migraine attacks. | Studies showing increased inflammatory markers in both migraine and MS patients; observed overlap in immune cell activation. |
| Neurotransmitter Imbalances | Disruptions in neurotransmitter systems (e.g., serotonin, glutamate, CGRP) in both conditions, leading to pain perception and other symptoms. | Observed altered levels of neurotransmitters in migraine and MS patients; studies demonstrating the role of these neurotransmitters in migraine mechanisms. |
| Immune System Dysregulation | Possible link between immune system dysfunction and migraine, potentially involving the release of inflammatory molecules. | Studies exploring the role of immune cells and cytokines in both conditions; need for further investigation to elucidate specific pathways. |
| Genetic Predisposition and Environmental Factors | Genetic predisposition combined with environmental factors (infections, stress, lifestyle) might contribute to the development of both conditions. | Family history studies showing increased risk of both conditions; observations of environmental triggers for both migraine and MS. |
Symptoms and Diagnosis Challenges
Navigating the complexities of migraine and multiple sclerosis (MS) presents a significant diagnostic hurdle. The overlapping symptoms between these conditions can lead to misdiagnosis or delayed treatment, impacting the quality of life for those affected. Understanding these overlaps is crucial for healthcare professionals to ensure accurate diagnoses and appropriate management strategies.The intricate interplay of neurological symptoms in migraine and MS can make distinguishing one from the other challenging.
The connection between migraines and multiple sclerosis is fascinating, but often poorly understood. While the exact mechanisms are still being researched, some theories suggest a role for the nucleus pulposus, the gelatinous center of the intervertebral discs. Understanding this structure, as detailed in this resource on what is the nucleus pulposus , could potentially shed light on the pain pathways involved in both conditions.
Ultimately, further research into these intricate connections is crucial for developing more effective treatments for both migraines and multiple sclerosis.
Both conditions can manifest with similar symptoms, creating a diagnostic puzzle for healthcare providers. A thorough neurological evaluation, coupled with a detailed patient history, is paramount to correctly identifying the underlying condition.
Mimicking Symptoms and Overlap
Migraine and MS share a range of neurological symptoms, which can lead to diagnostic confusion. Headaches, visual disturbances, numbness, tingling, and weakness are common to both conditions. The episodic nature of migraine attacks can mimic the unpredictable presentation of MS symptoms, further complicating diagnosis.
Diagnostic Challenges in MS Patients with Migraine
Identifying migraine in individuals with MS is particularly challenging due to the overlapping symptoms. The episodic nature of migraine headaches can be mistaken for exacerbations of MS, potentially delaying or misdirecting appropriate treatment for the migraine. Furthermore, the neurological symptoms of MS, such as sensory disturbances and motor weakness, can obscure the presence of a migraine attack. For instance, a patient experiencing a migraine aura with visual disturbances might be misdiagnosed with an MS attack.
Diagnostic Scenarios
The following table highlights some common diagnostic scenarios where both conditions are present, emphasizing the importance of a comprehensive neurological evaluation:
| Scenario | Symptoms | Potential Misdiagnosis |
|---|---|---|
| Patient with MS experiencing frequent headaches, accompanied by nausea and photophobia. | Headaches, nausea, photophobia, neurological symptoms associated with MS. | Migraine might be overlooked, leading to a focus solely on MS management. |
| Patient with a history of MS experiencing a sudden onset of severe headache with visual disturbances. | Severe headache, visual disturbances, neurological symptoms associated with MS. | The visual disturbances could be misinterpreted as an MS attack, potentially delaying treatment for migraine. |
| Patient presenting with MS symptoms and episodic headaches that worsen with stress or lack of sleep. | MS symptoms, episodic headaches worsening with stress or sleep deprivation. | MS symptoms could overshadow the potential migraine component. |
Importance of Thorough Neurological Evaluation
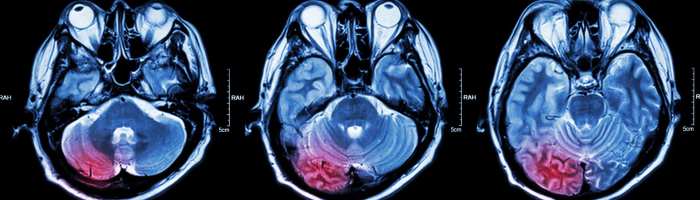
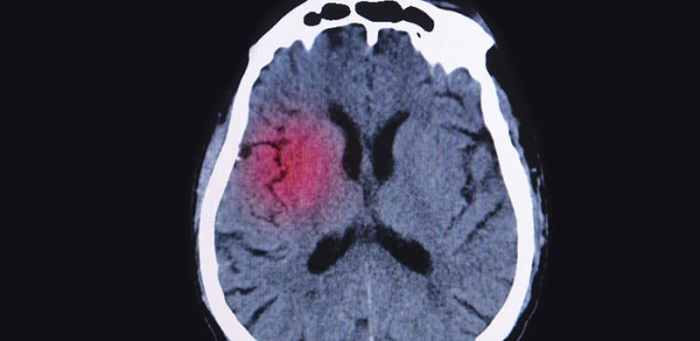
A thorough neurological evaluation is crucial in differentiating migraine from MS. This evaluation should include a detailed patient history, a comprehensive neurological examination, and appropriate diagnostic tests. Neuroimaging, such as MRI scans, can help rule out other neurological conditions and identify potential structural abnormalities. Electroencephalography (EEG) can help assess brain activity, which may offer further insights into the nature of the symptoms.
Neurological testing focusing on specific neurological functions like vision and motor skills can also be helpful.
While the connection between migraines and multiple sclerosis is still being researched, some sufferers experience both conditions. Finding effective treatments for skin issues like facial eczema can be challenging, and fortunately, there are resources available to help. For example, learning about eczema on face treatment strategies can improve overall well-being. Ultimately, understanding the potential overlap between these conditions is crucial for comprehensive care.
A detailed patient history, comprehensive neurological examination, and appropriate diagnostic tests are essential in differentiating migraine from MS.
Ever wondered about the connection between migraines and multiple sclerosis? It’s a complex area, but research is ongoing. Interestingly, some folks with chronic pain conditions, like fibromyalgia, find that using mobility aids can significantly improve their quality of life. For instance, exploring options like mobility aids with fibromyalgia could help manage symptoms and allow for greater independence.
Ultimately, understanding these connections can help in better managing the symptoms associated with both migraine and multiple sclerosis.
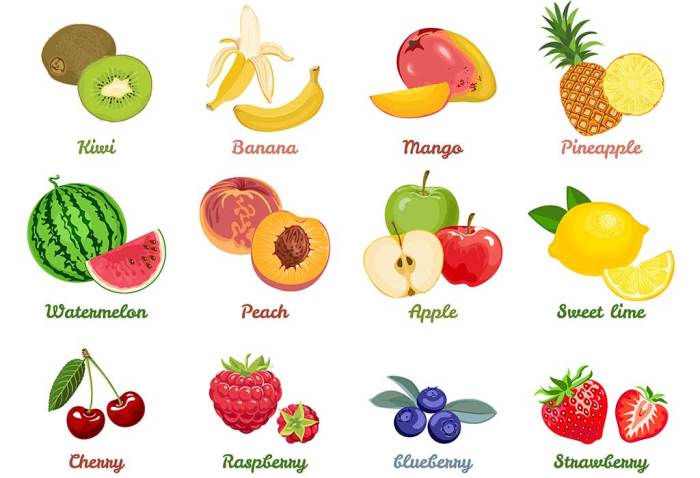
Treatment Strategies and Management: Migraine And Multiple Sclerosis Connection
Managing migraine alongside multiple sclerosis (MS) presents unique challenges. The overlapping symptoms and potential for drug interactions require a meticulous and personalized approach. Treatment plans must consider both conditions, aiming for effective migraine relief without exacerbating MS symptoms or increasing the risk of adverse effects. This necessitates a collaborative effort between neurologists specializing in both conditions to develop the most suitable strategy.Treatment approaches for migraine in individuals with MS often involve a combination of therapies.
This approach aims to address the underlying causes of migraine while minimizing potential interactions with MS medications. A crucial aspect of this process is careful monitoring of both conditions to ensure treatment effectiveness and safety.
Comparison of Treatment Approaches
Migraine treatments for individuals without MS often include over-the-counter pain relievers, triptans, and preventive medications. For those with MS, these options are often considered, but with extra caution due to potential drug interactions. Sometimes, alternative or complementary therapies are incorporated to provide a holistic approach, which might include acupuncture, biofeedback, or dietary modifications. Tailored treatment plans are essential to account for the specific needs and sensitivities of each patient.
Potential Drug Interactions
Careful consideration of drug interactions is paramount. Triptans, frequently used for migraine attacks, can interact with medications used to treat MS. For example, some MS medications may influence the metabolism of triptans, potentially altering their effectiveness or increasing the risk of side effects. Similarly, some preventive migraine medications may have interactions with immunosuppressants or disease-modifying therapies used in MS management.
Open communication between the neurologist and the patient about all medications is essential to avoid potential problems.
Table of Common Migraine Treatments and Potential Effects on MS Symptoms, Migraine and multiple sclerosis connection
| Treatment | Migraine Impact | MS Impact |
|---|---|---|
| Over-the-counter pain relievers (e.g., ibuprofen, naproxen) | Effective for mild to moderate migraines; may cause gastrointestinal upset. | Generally well-tolerated; can cause stomach issues in some individuals. No significant interactions with common MS medications are reported. |
| Triptans (e.g., sumatriptan) | Effective in aborting acute migraine attacks; potential for vasoconstriction; contraindicated in individuals with cardiovascular conditions. | May interact with certain MS medications, potentially affecting their effectiveness or increasing the risk of side effects; close monitoring is essential. |
| Preventive medications (e.g., beta-blockers, anti-epileptics) | Can reduce migraine frequency and severity; may have side effects such as fatigue or dizziness. | Some preventive migraine medications may interact with MS medications, potentially affecting their effectiveness or increasing the risk of side effects; close monitoring is essential. |
| Botox | Effective for chronic migraine; may cause localized muscle weakness. | Generally safe; requires careful consideration of potential interactions with MS medications, especially those that affect muscle function. |
Importance of Lifestyle Modifications
Managing both migraine and MS effectively often requires lifestyle modifications beyond medication. Maintaining a consistent sleep schedule, managing stress levels, and adhering to a healthy diet can significantly impact both conditions. These lifestyle adjustments can contribute to reducing the frequency and intensity of migraine attacks and potentially alleviate some MS symptoms. Recognizing triggers and implementing strategies to avoid them is crucial.
Lifestyle Factors Exacerbating Migraine in MS
Several lifestyle factors can exacerbate migraine attacks in individuals with MS. These include:
- Poor sleep quality or inconsistent sleep schedule: Disrupted sleep patterns are known triggers for migraine in general and are often worsened in MS patients. Maintaining a regular sleep schedule is important for both conditions.
- Stress and anxiety: Stress can trigger both migraine attacks and MS symptoms. Strategies for stress reduction, such as meditation, yoga, or mindfulness exercises, can be beneficial.
- Dehydration: Dehydration can trigger migraine headaches. Staying well-hydrated is important for overall health, including migraine management.
- Changes in weather patterns: Fluctuations in barometric pressure and temperature can sometimes act as migraine triggers. Understanding these patterns can help individuals with MS anticipate potential attacks.
- Dietary triggers: Certain foods and drinks, such as aged cheeses, processed meats, and caffeine, can trigger migraine attacks. Identifying individual sensitivities through careful dietary tracking is essential.
Research and Future Directions
Unraveling the complex relationship between migraine and multiple sclerosis (MS) requires dedicated research efforts. Current studies are exploring potential mechanisms, identifying biomarkers, and developing targeted therapies. The potential for improved diagnostics and more effective treatments hinges on advancing our understanding of this often-overlooked connection.Understanding the underlying biological mechanisms linking migraine and MS is crucial. Future research should aim to identify shared genetic predispositions, common immune system dysregulation, and potential neural pathways that contribute to both conditions.
This knowledge will pave the way for more precise diagnostic tools and potentially novel therapeutic strategies.
Current Research Areas
Research into the migraine-MS connection is multifaceted, encompassing various disciplines. Studies are investigating the role of inflammation, immune system dysfunction, and neurotransmitter imbalances in the development and exacerbation of both conditions. Genetic studies are exploring shared genetic vulnerabilities, while neuroimaging techniques are mapping potential structural and functional brain changes.
Potential Avenues for Future Research
Future research should focus on developing innovative approaches to investigate the underlying mechanisms. This includes leveraging large-scale biobanks to identify specific biomarkers associated with migraine in MS patients. Further exploration of the role of gut microbiota and its potential interaction with the immune system in both conditions is a promising area of investigation.
Importance of Clinical Trials and Observational Studies
Ongoing clinical trials are essential to evaluate the efficacy and safety of novel treatments targeting both migraine and MS. Observational studies tracking long-term outcomes in patients with both conditions will provide invaluable insights into the progression of the diseases and the impact of potential treatments. This data will be crucial for informing clinical practice guidelines.
Recent Research Findings
Recent studies have highlighted the potential for shared genetic factors in migraine and MS. Research also indicates a possible correlation between certain immune responses and the frequency and severity of migraine attacks in individuals with MS. These findings underscore the need for further investigation into the underlying mechanisms.
Key Research Questions and Potential Future Studies
| Research Question | Methodology | Expected Outcome |
|---|---|---|
| Are specific genetic variants associated with increased susceptibility to both migraine and MS? | Genome-wide association studies (GWAS) on large cohorts of individuals with both conditions. Gene expression profiling of immune cells in both conditions. | Identification of potential susceptibility genes and pathways, leading to the development of targeted therapies. |
| Does gut microbiome dysbiosis play a role in migraine exacerbation in MS patients? | Comparative analysis of gut microbiome composition in migraine-prone MS patients versus those without migraine. Investigate the impact of probiotics and prebiotics on migraine frequency and severity. | Understanding the potential link between gut health and neurological symptoms in MS, potentially identifying new therapeutic targets. |
| Can neuroimaging techniques identify specific brain structural or functional changes associated with migraine in MS patients? | Advanced MRI techniques, including diffusion tensor imaging (DTI) and functional MRI (fMRI), on MS patients with and without migraine. | Potential identification of specific brain regions or pathways that contribute to migraine symptoms in MS, aiding in improved diagnostic tools. |
| Do specific immune cells or inflammatory markers contribute to the exacerbation of migraine in MS patients? | Detailed analysis of immune cell populations and inflammatory markers in blood and cerebrospinal fluid samples from MS patients with and without migraine. | Identification of specific inflammatory pathways and biomarkers that can be targeted for treatment development. |
End of Discussion
In conclusion, the connection between migraine and multiple sclerosis is complex and multifaceted. While research continues to unravel the intricacies of this link, a deeper understanding of the shared symptoms, underlying mechanisms, and diagnostic challenges is crucial for improving patient outcomes. By acknowledging the complexities and the potential for misdiagnosis, we can work towards more effective treatment and management strategies for individuals affected by both conditions.
Further research is vital to unlock the full potential of personalized care and tailored interventions.