Fear of cotton balls sidonglobophobia – Fear of cotton balls, or sidonglobophobia, is a fascinating and sometimes unsettling phobia. This detailed exploration delves into the nature of this unusual fear, examining its triggers, symptoms, potential origins, and even possible treatment approaches. We’ll unpack what makes this specific phobia tick and compare it to other texture- or object-based anxieties.
Understanding sidonglobophobia requires looking at its potential origins, from early childhood experiences to cultural influences. We’ll analyze potential underlying causes and explore how this phobia might develop over time. The following sections will delve into specific examples, comparing it to similar phobias and discussing possible treatment strategies.
Defining Sidonglobophobia
Sidonglobophobia, the fear of cotton balls, is a specific phobia characterized by an intense and irrational dread of these seemingly innocuous objects. While the exact prevalence of this phobia is unknown, it’s important to remember that anxiety disorders, including phobias, can affect individuals across various demographics and backgrounds. Understanding the triggers, symptoms, and potential causes can help in recognizing and addressing this condition.The fear of cotton balls, like any phobia, is rooted in an overblown response to a perceived threat.
This fear response, while not logical or rational, can be deeply distressing for the individual experiencing it. The fear isn’t simply a dislike; it’s an overwhelming anxiety that can disrupt daily life. It’s important to remember that phobias are treatable, and seeking professional help is a crucial step in managing this condition effectively.
Description of Sidonglobophobia
Sidonglobophobia, the fear of cotton balls, is a specific phobia characterized by a persistent and excessive fear response to cotton balls. This fear is often disproportionate to the actual danger posed by the object. The experience can range from mild discomfort to full-blown panic attacks. The fear is not limited to the visual presence of cotton balls; it can extend to tactile experiences, even the thought or imagined presence of cotton balls.
Potential Triggers
Several triggers can activate the fear response in individuals with sidonglobophobia. Direct exposure to cotton balls, whether in their pure form or as part of products like cotton swabs, cotton balls for wounds, or decorative arrangements, can be a significant trigger. The sight or even the smell of cotton balls can elicit a strong anxiety response. The fear might also be associated with a traumatic experience involving cotton balls or a similar textured object, or it may stem from a conditioned response where a neutral stimulus becomes associated with a negative experience.
Common Symptoms and Reactions
Individuals experiencing sidonglobophobia may exhibit a range of symptoms. These symptoms can manifest physically, cognitively, and behaviorally. Physical symptoms might include rapid heartbeat, sweating, trembling, shortness of breath, nausea, or dizziness. Cognitive symptoms may involve overwhelming thoughts and feelings of dread, fear, and panic. Behavioral reactions might include avoidance behaviors, such as refusing to be near cotton balls or any associated items.
Individuals might also experience intense anxiety and distress in the presence of cotton balls, leading to feelings of helplessness and discomfort.
Potential Underlying Causes
The exact causes of sidonglobophobia, as with many phobias, are not fully understood. However, several factors might contribute to its development. These include a history of trauma or negative experiences involving cotton balls or similar textured objects, or a genetic predisposition to anxiety disorders. A learned or conditioned response, where a neutral stimulus becomes associated with a negative experience, can also contribute to the development of this phobia.
Similarities and Differences with Other Texture/Object Phobias
| Phobia | Similarities | Differences |
|---|---|---|
| Sidonglobophobia | Intense fear response, avoidance behaviors, potential for panic attacks. | Specific focus on the texture and appearance of cotton balls. Triggers often linked to cotton balls directly. |
| Textophobia | Fear response associated with textures. | Broader scope, encompassing various textures; not limited to cotton balls. Triggers can be diverse tactile experiences. |
| Trichophobia | Fear response associated with hair or fibers. | Focus on hair, fibers, or strands; cotton balls might trigger this if viewed as a collection of fibers. |
| Globophobia | Fear response associated with balloons. | Focus on balloons; no direct connection to the texture of cotton balls. |
Exploring the Origin and Development
Fear of cotton balls, or sidonglobophobia, is a relatively unexplored phobia. While specific historical roots are difficult to pinpoint, understanding its potential development provides insight into the broader nature of phobias. Examining potential origins, contributing factors, and symptom progression helps to contextualize this specific fear within the realm of anxiety disorders. The complexities of phobias often stem from a combination of environmental and psychological influences, which we will explore further.Understanding the potential origins and developmental trajectory of sidonglobophobia is crucial for developing effective treatment strategies.
This involves delving into the possible psychological mechanisms and triggers that might lead to the development of such a specific fear. It’s important to recognize that fear responses can vary significantly in intensity and manifestation, highlighting the importance of individualized treatment approaches.
Potential Historical Context
While there’s no documented historical record of a widespread fear of cotton balls, understanding the broader historical context of fear and anxiety can offer some clues. The fear of the unknown, the association of certain textures or objects with negative experiences, and cultural anxieties can all play a role in the development of specific phobias. Historical accounts of similar fears, like a fear of spiders or heights, can shed light on the evolutionary and societal factors contributing to anxiety disorders.
Contributing Factors to Development
Several factors can contribute to the development of sidonglobophobia. These might include:
- Early Childhood Experiences: A traumatic experience involving cotton balls, or a close association with cotton balls and a negative experience, could lead to the development of this phobia. For instance, a child who experienced a painful medical procedure involving cotton balls might develop a strong aversion to them.
- Learned Behavior: Observing others react fearfully to cotton balls, or having negative experiences reported about cotton balls, could lead to the acquisition of this fear through observational learning.
- Generalized Anxiety: An underlying anxiety disorder could predispose a person to developing a specific phobia, including sidonglobophobia. Individuals with pre-existing anxiety are more susceptible to developing specific fears.
Symptom Progression
The progression of symptoms can vary widely depending on the individual and the severity of the phobia. In mild cases, the individual might experience mild discomfort or unease upon encountering cotton balls. In more severe cases, the phobia can manifest as intense anxiety, panic attacks, or avoidance behaviors. The progression of symptoms might also be influenced by exposure to cotton balls, or perceived exposure, and can escalate over time.
Theories Regarding Phobia Development
| Theory | Description |
|---|---|
| Behavioral Conditioning | Learned associations between cotton balls and negative experiences. |
| Evolutionary Predisposition | Potential ancestral responses to perceived threats associated with certain textures or objects. |
| Cognitive Factors | Distorted or negative thoughts and beliefs about cotton balls. |
| Psychodynamic Factors | Unresolved conflicts or past traumas potentially linked to cotton balls. |
Examples of Potential Childhood Experiences
Examples of childhood experiences that could contribute to sidonglobophobia include:
- A child receiving a vaccination or a medical procedure involving cotton balls, which created a negative emotional association.
- A child witnessing a sibling or a friend expressing fear or distress related to cotton balls, leading to the adoption of similar fears.
- A child having a positive association with cotton balls, but the association later becoming negative, perhaps due to a negative experience related to cotton balls, like being stung by a bee wrapped in a cotton ball.
Comparing to Other Phobias
Sidonglobophobia, the fear of cotton balls, while seemingly unique, shares surprising similarities with other specific phobias. Understanding these connections helps us grasp the psychological underpinnings of this seemingly unusual fear. Examining the overlapping symptoms and reactions, as well as the underlying psychological mechanisms, reveals valuable insights into the nature of phobias in general.Analyzing sidonglobophobia in relation to other phobias offers a broader perspective, moving beyond the specifics of cotton balls to understand the common threads that weave through various anxieties.
This comparison allows us to identify patterns and explore the shared psychological mechanisms driving these fears.
Ever heard of sidonglobophobia, the fear of cotton balls? It’s a fascinating quirk, but it might be less surprising when considering the stresses teens face. Recent studies, like the pandemic teen mental health study , highlight the significant impact the pandemic has had on their well-being. Perhaps, some of these anxieties manifest in unusual ways, like a phobia of seemingly innocuous items.
This highlights how important it is to understand and support young people during difficult times.
Similarities with Texture-Based Phobias
A significant comparison point for sidonglobophobia lies in its connection to other texture-based phobias. These phobias often involve a heightened sensitivity to the tactile experience, leading to intense anxiety and avoidance responses. For instance, trypophobia, the fear of clustered holes or patterns, shares this tactile aspect, triggering a similar aversion and sometimes even physical reactions. The feeling of the texture itself, rather than the object’s inherent properties, becomes the primary source of fear.
This tactile focus highlights a common element in various phobias related to touch.
Overlap in Symptoms and Reactions
The symptoms and reactions associated with sidonglobophobia exhibit considerable overlap with those of other phobias, particularly those related to textures and objects. These shared reactions often include a range of physiological responses, such as increased heart rate, rapid breathing, sweating, and feelings of intense anxiety. Cognitive symptoms, like intrusive thoughts and negative self-assessments, also frequently accompany the experience of fear.
In many cases, individuals with these phobias experience a strong desire to avoid the triggering stimulus, leading to significant disruptions in daily life. For example, someone with a fear of cotton balls might go to great lengths to avoid situations where they might encounter cotton balls.
Psychological Similarities and Differences
The psychological underpinnings of sidonglobophobia and other phobias share a common foundation in learned associations and conditioned responses. While the specific triggers may differ, the core mechanism of fear conditioning—where a neutral stimulus becomes associated with a negative experience—remains consistent. The specific pathways and associated memories driving these responses, however, may differ, leading to individual variations in the intensity and manifestation of fear.
This highlights the complex interplay between environmental factors, personal experiences, and individual vulnerabilities in the development of phobias.
Ever heard of sidonglobophobia, the fear of cotton balls? It’s a fascinating, albeit somewhat unusual, phobia. While dealing with such anxieties can be challenging, it’s important to remember that there are resources available for navigating similar fears. For example, coping with a condition like macular degeneration requires support and strategies for living well, and understanding how to manage such situations can be extremely helpful in facing other challenges like sidonglobophobia.
Finding resources like macular degeneration coping support and living well can provide valuable insight and strategies for navigating difficult situations. Ultimately, the key is finding support and resources to help manage any kind of anxiety, including the unusual but real fear of cotton balls.
Comparison Table, Fear of cotton balls sidonglobophobia
| Phobia | Trigger | Common Symptoms | Psychological Factors |
|---|---|---|---|
| Sidonglobophobia | Cotton balls | Increased heart rate, anxiety, avoidance | Learned associations, tactile sensitivity |
| Trypophobia | Clustered patterns/holes | Disgust, anxiety, skin crawling | Evolutionary, cultural factors |
| Arachnophobia | Spiders | Panic, avoidance, fear | Learned associations, cultural conditioning |
Common Threads in Phobia Development
A recurring theme in the development of various phobias is the role of learned associations. Exposure to negative experiences, whether real or perceived, can create lasting connections between a particular stimulus and feelings of fear. For example, a traumatic experience involving a cotton ball could trigger a conditioned response in which the mere sight or touch of a cotton ball elicits intense anxiety.
Furthermore, cultural influences and individual vulnerabilities play crucial roles in shaping the specific manifestation of fear responses. These factors, combined with the learned associations, contribute to the complex and diverse landscape of phobias.
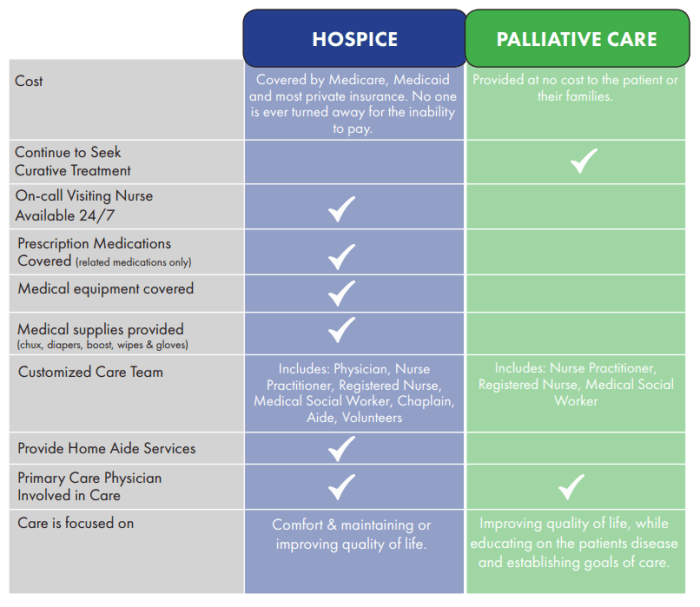
Potential Treatment Approaches
Treating sidonglobophobia, like any phobia, involves addressing both the behavioral and emotional aspects of the fear response. Successful treatment often combines various therapeutic techniques, tailored to the individual’s specific needs and the severity of their phobia. A multi-faceted approach often yields the best results.Understanding the root causes of the fear, whether learned or developed over time, is crucial in creating an effective treatment plan.
This involves exploring the individual’s past experiences, identifying triggers, and understanding the associated anxieties and emotional responses. Therapists work to help patients develop coping mechanisms and strategies for managing their fear in real-world situations.
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a widely recognized and effective approach for treating phobias. CBT focuses on identifying and challenging negative thought patterns and behaviors that contribute to the fear response. This approach helps patients understand the connection between their thoughts, feelings, and behaviors. Through CBT, patients can learn to reframe their thoughts about cotton balls and develop healthier coping mechanisms.
Exposure Therapy
Exposure therapy is a cornerstone of treating phobias. It involves gradually exposing the patient to the feared stimulus, cotton balls, in a controlled and safe environment. This gradual exposure helps to reduce the anxiety response over time. The therapy aims to desensitize the patient to the feared object, ultimately reducing the intensity of their fear response. Exposure therapy can be conducted in various settings, from the therapist’s office to real-life situations.
Example Exposure Therapy Techniques
- Imaginal Exposure: Patients visualize cotton balls in increasing levels of proximity and interaction. This technique helps them process the fear response in a safe environment before confronting the actual object. For example, starting with a picture of a cotton ball, then moving to a video of someone handling a cotton ball, and finally to imagining themselves holding a cotton ball.
- In Vivo Exposure: This involves direct exposure to the feared stimulus. A therapist might start by having the patient look at a cotton ball from a distance, then gradually increase the proximity. For example, starting by holding a picture of a cotton ball, to holding a small cotton ball, and then moving to a large cotton ball.
Other Therapeutic Approaches
Other therapeutic approaches may also be used in conjunction with CBT and exposure therapy. These may include:
- Relaxation techniques: These techniques, such as deep breathing exercises and progressive muscle relaxation, help manage anxiety and promote a sense of calm. These can be used to reduce the physiological response to the feared stimulus.
- Mindfulness-based therapies: Mindfulness practices can help patients become more aware of their thoughts and feelings without judgment. This can help them manage anxiety and develop a more balanced perspective on their fear.
- Acceptance and Commitment Therapy (ACT): This therapy focuses on accepting difficult emotions and thoughts rather than trying to change them. It helps patients develop a sense of self-compassion and resilience.
Success Rates and Considerations
| Therapeutic Approach | Potential Success Rate (estimated) | Considerations |
|---|---|---|
| Cognitive Behavioral Therapy (CBT) | 70-90% | Requires active participation and commitment from the patient. |
| Exposure Therapy | 60-80% | Requires careful planning and gradual exposure to prevent overwhelming the patient. |
| Relaxation Techniques | 40-70% | Can be helpful as an adjunct to other therapies but not a primary treatment. |
| Mindfulness-based Therapies | 50-80% | May not be suitable for all individuals, especially those with severe phobias. |
Note: Success rates are estimates and can vary depending on individual factors, the severity of the phobia, and the therapist’s expertise.
Illustrative Cases and Scenarios: Fear Of Cotton Balls Sidonglobophobia

Sidonglobophobia, the fear of cotton balls, manifests in a range of intensities and triggers. Understanding these varied reactions is crucial for developing effective treatment strategies. This section delves into fictional case studies, illustrating the diverse ways this phobia can impact individuals’ lives.
Fictional Case Studies
These case studies are fictional representations designed to illustrate the spectrum of sidonglobophobia. They highlight the psychological and physiological responses individuals may experience when confronted with cotton balls.
- Case Study 1: Mild Phobia. Amelia, a 28-year-old graphic designer, experiences a mild but noticeable unease when encountering cotton balls. She feels a slight sense of anxiety and a rapid heartbeat when seeing a pile of cotton balls. The discomfort is manageable, and she can typically avoid direct contact. This illustrates the less intense side of the phobia, where avoidance strategies might be sufficient for managing the anxiety.
- Case Study 2: Moderate Phobia. David, a 35-year-old construction worker, experiences a heightened sense of anxiety when exposed to cotton balls. He finds himself overwhelmed by a sense of dread and experiences nausea and dizziness. The sight of cotton balls triggers a fear of suffocation and a panic attack, which can significantly impact his daily activities and require professional intervention. This case exemplifies a moderate level of sidonglobophobia, requiring more intensive therapeutic approaches.
Ever heard of sidonglobophobia? It’s the fear of cotton balls, which, admittedly, seems a bit unusual. While I’m no expert on treating anxiety disorders, I’ve been doing some research, and it seems like managing nerve pain can sometimes be a similar mental hurdle. For instance, figuring out how long to take gabapentin for nerve pain how long to take gabapentin for nerve pain can be tricky, and finding the right approach to managing the discomfort can be just as daunting as facing a mountain of cotton balls.
Maybe that’s why both situations can trigger anxiety in some people. It’s all about finding what works best for you, and hopefully, with a little understanding, we can all conquer our fears, even the fear of cotton balls.
- Case Study 3: Severe Phobia. Sophia, a 19-year-old college student, experiences a severe phobia of cotton balls. The mere presence of cotton balls, even in an indirect way like a picture in a magazine, causes an immediate and overwhelming panic attack. She experiences intense fear, difficulty breathing, sweating profusely, and feels a sense of impending doom. This case demonstrates a severe phobia, where the individual may require intensive therapy, including exposure therapy and medication, to manage the debilitating effects of the phobia.
Scenario: Triggering Event
Imagine a scenario where a person with sidonglobophobia is in a medical office. A doctor places a small, seemingly innocuous wad of cotton balls on a tray beside the patient. The patient’s initial reaction is one of discomfort, and the feeling intensifies as the doctor proceeds to use the cotton balls to swab their throat. The sight and proximity of the cotton balls triggers a physiological response.
Physiological and Psychological Responses
The physiological responses to the trigger in the scenario above could include a rapid heartbeat, sweating, shortness of breath, nausea, and dizziness. Psychologically, the individual might experience intense fear, feelings of helplessness, and a desire to escape the situation. These reactions vary depending on the individual’s level of phobia.
Fictional Accounts of Successful Treatment
- Case Study 1 Outcome. Amelia, in Case Study 1, successfully managed her phobia through cognitive behavioral therapy (CBT). CBT techniques helped her identify and challenge negative thoughts associated with cotton balls. Gradual exposure to cotton balls, in a controlled environment, helped her desensitize to the stimulus. This illustrates the effectiveness of CBT in treating milder forms of sidonglobophobia.
- Case Study 2 Outcome. David, in Case Study 2, found that a combination of CBT and medication, specifically anti-anxiety medication, proved effective. Medication helped manage his panic attacks, while CBT techniques addressed the underlying anxieties. This case exemplifies the importance of a multifaceted approach for moderate to severe cases.
- Case Study 3 Outcome. Sophia, in Case Study 3, benefited from intensive therapy involving a combination of exposure therapy, medication, and relaxation techniques. Exposure therapy involved gradually exposing Sophia to cotton balls in a safe and controlled environment. This prolonged process, combined with other therapeutic strategies, ultimately led to significant improvements in her ability to cope with the phobia. This underscores the necessity of intensive and multifaceted treatment for severe cases.
Scenarios Table
| Case Study | Trigger | Physiological Response | Psychological Response | Treatment Approach |
|---|---|---|---|---|
| Case Study 1 | Direct sight of cotton balls | Slight unease, rapid heartbeat | Anxiety, discomfort | CBT, gradual exposure |
| Case Study 2 | Presence of cotton balls | Panic attack, nausea, dizziness | Dread, fear of suffocation | CBT, medication |
| Case Study 3 | Sight or even indirect mention of cotton balls | Panic attack, difficulty breathing, sweating | Impending doom, intense fear | Intensive therapy, exposure therapy, medication, relaxation techniques |
Social and Cultural Aspects
Sidonglobophobia, like other phobias, isn’t isolated within the individual. Social and cultural contexts play a significant role in how this fear develops, is perceived, and is expressed. Cultural norms and societal expectations can both reinforce and mitigate the experience of this fear, impacting its manifestation and the potential for seeking help.Cultural norms significantly shape how individuals experience and express their fears.
Some cultures might emphasize stoicism and discourage open displays of anxiety, potentially leading individuals with sidonglobophobia to internalize their fear and avoid seeking help. Conversely, other cultures might encourage emotional expression, making it easier for individuals to acknowledge and address their anxieties.
Cultural Influences on Phobia Development
Cultural values surrounding emotional vulnerability and the expression of fear can greatly impact how sidonglobophobia develops. In collectivist cultures, where maintaining social harmony is paramount, individuals might suppress feelings of fear to avoid disrupting the group dynamic. This suppression could potentially contribute to the internalization of the fear and the delay in seeking help. Conversely, in individualistic cultures, where personal expression is more encouraged, individuals might be more likely to seek help for their fears, including sidonglobophobia, if they feel comfortable doing so.
Societal Expectations and Phobia Experience
Societal expectations concerning appropriate behaviors and responses to anxiety can also influence the experience of sidonglobophobia. If societal norms portray fear as a weakness or something to be ashamed of, individuals experiencing this fear might struggle to acknowledge or address it. Conversely, if society acknowledges and normalizes fear as a part of the human experience, individuals might be more likely to seek help and support.
Comparison of Cultural Perspectives on Phobias
| Culture | General Attitude Towards Phobias | Expression of Phobia | Seeking Help |
|---|---|---|---|
| Collectivist Cultures (e.g., some Asian cultures) | Emphasis on social harmony, potentially discouraging open expression of fear | Internalized fear, avoidance of social situations | Seeking help might be delayed or discouraged due to societal stigma |
| Individualistic Cultures (e.g., Western cultures) | More open discussion of personal struggles, potentially leading to more awareness and acceptance of phobias | Fear might be more openly expressed | More likely to seek professional help if perceived as necessary |
| Cultures with Strong Religious or Spiritual Beliefs | May attribute phobias to supernatural causes, affecting understanding and treatment | Fear might be interpreted through a spiritual lens | Seeking help might involve religious or spiritual practices |
Evolution of Societal Attitudes Towards Phobias
Societal attitudes towards phobias have evolved significantly over time. In the past, phobias were often viewed as a sign of weakness or a personal failing. Individuals with phobias were sometimes ostracized or treated with disdain. However, with increased understanding of mental health conditions, societies are increasingly recognizing phobias as legitimate experiences requiring support and treatment. Increased awareness campaigns and the work of mental health professionals have played a crucial role in changing perceptions.
The development of evidence-based treatments, such as cognitive behavioral therapy (CBT), has further contributed to this shift. This shift reflects a greater acceptance of mental health conditions and a recognition of the importance of addressing them effectively.
Public Perception and Misconceptions
Public perception often plays a significant role in shaping the experience of individuals with phobias. Misconceptions surrounding mental health conditions, including phobias, can lead to stigma, isolation, and a lack of understanding. This can negatively impact those experiencing the phobia, hindering their ability to seek help and manage their condition effectively. Understanding these perceptions is crucial for fostering empathy and promoting accurate information.Common misconceptions about phobias often stem from a lack of awareness about the debilitating nature of these conditions.
People may incorrectly assume that phobias are simply a matter of choice or overreaction, overlooking the physiological and psychological factors that contribute to the fear response. This lack of understanding can contribute to judgment and prejudice, leading to a less supportive environment for those affected.
Common Misconceptions About Phobias
Misconceptions about phobias, in general, often stem from a lack of understanding about the complexities of anxiety disorders. These misunderstandings can lead to negative perceptions and stigmatization of individuals who experience these conditions.
- Phobias are simply irrational fears.
- People with phobias can simply “get over it” by choosing to not be afraid.
- Phobias are a sign of weakness or a lack of character.
- People with phobias are simply exaggerating their fear or attention-seeking.
- Phobias are not a serious mental health condition.
How People Perceive Sidonglobophobia
Understanding how sidonglobophobia is perceived is crucial to addressing the stigma surrounding it. While the exact public perception is difficult to quantify, it’s likely that the unusual nature of the phobia – fear of cotton balls – could lead to misunderstandings and potentially even ridicule. The uncommon nature of the trigger could be misinterpreted as a lack of seriousness or a trivialization of the condition.
Potential Impact of Misconceptions on Sidonglobophobia Sufferers
The negative impact of misconceptions on those experiencing sidonglobophobia can be substantial. Feeling misunderstood, judged, or stigmatized can lead to significant distress and social isolation. Fear of judgment can prevent individuals from seeking help, delaying or preventing effective treatment.
Common Stereotypes and Prejudices
Stereotypes and prejudices related to sidonglobophobia may stem from the uncommon nature of the phobia. There may be a tendency to dismiss the fear as insignificant or even humorous, overlooking the real distress and impairment it causes. Such attitudes can contribute to a sense of alienation and reinforce feelings of inadequacy for those affected.
Table of Common Misconceptions and Explanations
| Misconception | Explanation |
|---|---|
| Phobias are simply irrational fears. | Phobias involve a significant physiological and psychological response. The fear is not simply a matter of choice but a complex interaction of brain chemistry, learned associations, and genetic predisposition. |
| People with phobias can simply “get over it.” | Phobias are not easily overcome through willpower alone. They require professional help and targeted interventions to address the underlying causes and learned responses. |
| Phobias are a sign of weakness. | Phobias are a genuine mental health condition that impacts individuals’ lives significantly. It is crucial to understand that they are not a sign of weakness but a symptom that requires professional support. |
| People with phobias are attention-seeking. | Phobias cause real suffering and impairment. The fear response is not a conscious attempt to gain attention but a genuine struggle with an anxiety disorder. |
| Phobias are not a serious mental health condition. | Phobias can significantly impact daily life, leading to avoidance behaviors, social isolation, and decreased quality of life. They are recognized as legitimate mental health conditions requiring appropriate treatment. |
Final Conclusion
In conclusion, sidonglobophobia, while seemingly unusual, highlights the complexity of phobias. Its triggers, symptoms, and potential origins provide insight into the human experience of fear. By exploring the potential treatment approaches, we can better understand the journey towards overcoming such anxieties. Ultimately, this exploration aims to shed light on the human psyche and the importance of understanding and addressing these unique fears.