Best time to take collagen sets the stage for a deep dive into optimizing your collagen supplement routine. Understanding how your body absorbs collagen is key to maximizing its benefits. Factors like meal timing, blood sugar levels, digestive health, and even the specific form of collagen you choose all play a role in how effectively your body utilizes this important protein.
This comprehensive guide explores the science behind collagen absorption, offering practical strategies for finding the optimal time to take your collagen supplements. We’ll delve into the nuances of different collagen types, meal composition, blood sugar management, and the role of digestive enzymes. By understanding these factors, you can unlock the full potential of your collagen regimen and support your overall well-being.
Understanding Collagen Absorption
Collagen, a crucial protein for maintaining healthy skin, joints, and connective tissues, is often taken as a supplement. However, the effectiveness of collagen supplements depends largely on how well the body absorbs it. This in-depth look explores the intricacies of collagen absorption, the factors influencing it, and the differences between various forms of collagen.Collagen absorption in the body is a multi-step process that begins in the digestive tract.
The body breaks down complex collagen molecules into smaller peptides, which are then absorbed into the bloodstream. This process isn’t always straightforward, and various factors can impact its efficiency. The form of collagen plays a key role, as different forms are broken down and absorbed at different rates.
Collagen Forms and Absorption Differences
Different forms of collagen supplements vary in their molecular structure and processing, which directly impacts their absorption rates. Hydrolyzed collagen, for example, is pre-digested, meaning the body has less work to do in breaking it down, leading to faster absorption. Conversely, non-hydrolyzed collagen requires more digestive effort, which can slow down the absorption process.
Factors Influencing Collagen Absorption
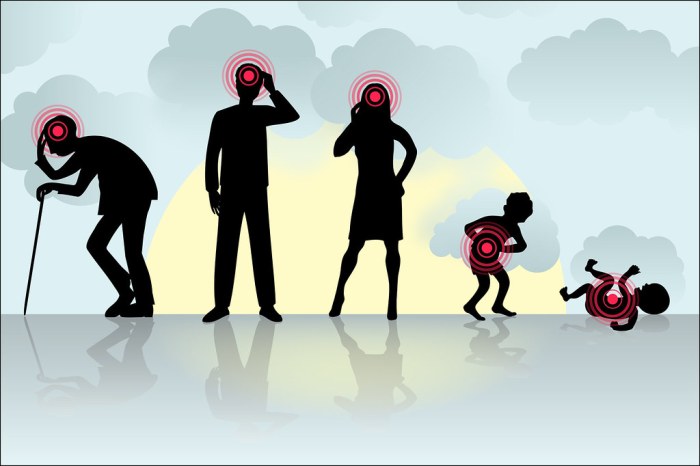
Several factors can influence how well the body absorbs collagen. Digestive health plays a critical role. Individuals with digestive issues, such as irritable bowel syndrome (IBS) or leaky gut syndrome, may experience reduced collagen absorption. Age is another important consideration. As we age, digestive efficiency often decreases, potentially affecting the absorption of collagen supplements.
Additionally, the presence of other nutrients in the diet can impact collagen absorption. For example, consuming collagen supplements with a meal rich in vitamin C might enhance absorption. The presence of other nutrients, such as zinc and vitamin C, can support the absorption of collagen.
Comparison of Collagen Supplement Absorption Rates
| Collagen Type | Processing | Absorption Rate (Estimated) | Comments |
|---|---|---|---|
| Hydrolyzed Collagen | Partially broken down into smaller peptides | High (70-80%) | Faster absorption due to pre-digestion. |
| Gelatin | Collagen protein that has been further processed | Medium (50-70%) | Similar to hydrolyzed collagen, but may vary depending on the specific processing method. |
| Non-hydrolyzed Collagen | Intact collagen molecules | Low (20-40%) | Requires significant digestive effort, potentially leading to lower absorption. |
Note: Absorption rates are estimates and can vary based on individual factors.
Impact of Meal Timing on Collagen Effectiveness
Collagen supplementation is gaining popularity, but understanding how to maximize its absorption and utilization is crucial for achieving desired results. One critical factor often overlooked is the impact of meal timing. The presence of food in your digestive system can significantly affect how your body processes and utilizes collagen peptides. This influence extends beyond simple digestion, impacting overall bioavailability and subsequent cellular uptake.Consuming collagen alongside a meal can alter its absorption rate compared to taking it on an empty stomach.
Figuring out the best time to take collagen supplements can be tricky, but it’s generally recommended to take it alongside a meal. This helps your body absorb it more efficiently. However, understanding how conditions like geographic atrophy are diagnosed, such as through detailed eye exams and OCT scans, can be equally important. how geographic atrophy is diagnosed is crucial for proactive health management, and this applies equally to maintaining optimal collagen absorption.
Ultimately, finding the best time to take collagen depends on your individual needs and lifestyle.
This interaction is complex, influenced by factors like the type of food consumed, the overall macronutrient profile of the meal, and individual digestive processes. Understanding these intricacies can help you optimize your collagen supplementation routine for better outcomes.
Meal Composition and Collagen Absorption
The composition of your meal directly influences collagen absorption. Meals high in protein, for example, may lead to a different absorption rate compared to meals with lower protein content. This is because the digestive system prioritizes the breakdown of protein-rich foods, potentially impacting the efficiency of collagen peptide uptake.
Impact of Protein Content on Collagen Absorption
Protein-rich meals can create a competitive environment in the digestive tract, potentially hindering the absorption of collagen peptides. Conversely, meals low in protein might allow for more efficient collagen absorption, as there’s less competition for digestive resources.
Optimal Meal Times for Collagen Supplementation
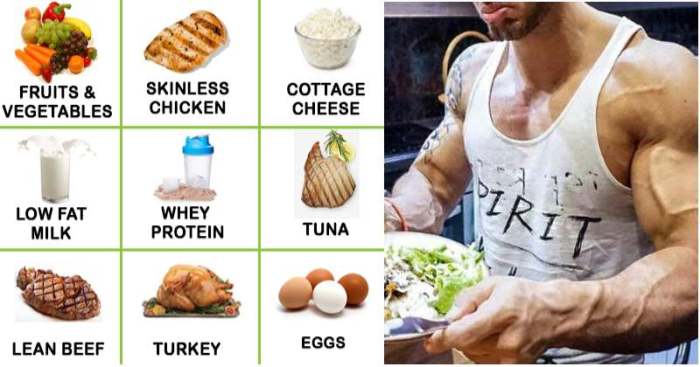
Determining the optimal meal time for collagen supplementation depends on individual factors, such as dietary habits, digestion, and overall health. A general guideline is to consider taking collagen peptides with a meal that contains moderate protein, avoiding both extremely high-protein and very low-protein meals. This allows for a balanced uptake without excessive competition or insufficient digestive support. For example, a meal containing lean protein (chicken, fish, or beans) and healthy carbohydrates (fruits, vegetables) could be a good choice.
Avoid taking collagen supplements right before or after consuming very high-fat meals as fat can slow down digestion.
Illustrative Table of Meal Composition Effects on Collagen Absorption
| Meal Composition | Protein Content | Potential Impact on Collagen Absorption |
|---|---|---|
| High-protein meal (e.g., steak with potatoes) | High | Potentially reduced absorption due to competition with other proteins |
| Moderate-protein meal (e.g., chicken breast with brown rice) | Moderate | Potentially optimal absorption, as competition is not overly high |
| Low-protein meal (e.g., salad with vinaigrette) | Low | Potentially increased absorption, as competition is minimal |
Relationship Between Blood Sugar and Collagen Absorption
Collagen, a vital protein for healthy skin, hair, and joints, is often supplemented to support these functions. However, the body’s ability to absorb and utilize collagen can be influenced by various factors, including blood sugar levels. Understanding this connection can help optimize collagen supplementation and maximize its benefits.Blood sugar levels, particularly fluctuating blood sugar, can significantly impact the absorption and effectiveness of collagen.
High or low blood sugar can disrupt the delicate metabolic processes that are necessary for optimal collagen utilization. Insulin, a key hormone involved in regulating blood sugar, plays a critical role in collagen metabolism, and imbalances in insulin response can lead to changes in collagen absorption and overall health.
Impact of Blood Sugar Spikes on Collagen Absorption
Blood sugar spikes, often associated with consuming sugary or processed foods, trigger a surge in insulin production. While insulin is essential for transporting glucose into cells, excessive insulin can potentially interfere with the absorption of other nutrients, including collagen. This interference can result in reduced collagen bioavailability, meaning the body is less able to utilize the collagen supplement for its intended purposes.
The body may preferentially use glucose for energy, potentially diverting resources away from collagen synthesis and absorption. For instance, individuals with poor glycemic control might find their collagen supplements less effective in promoting skin elasticity or joint health compared to those with stable blood sugar levels.
Impact of Blood Sugar Dips on Collagen Absorption
Conversely, prolonged or severe blood sugar dips can also negatively affect collagen absorption. When blood sugar levels drop significantly, the body might prioritize glucose utilization over other processes, including collagen synthesis. This can lead to a reduced ability to utilize collagen effectively. Furthermore, hypoglycemia, or low blood sugar, can trigger a release of stress hormones, potentially affecting collagen metabolism in an undesirable way.
This effect is less studied compared to the effects of high blood sugar, but is still worth noting.
Role of Insulin in Collagen Metabolism
Insulin, a crucial hormone in carbohydrate metabolism, plays a vital role in collagen metabolism. Insulin regulates glucose uptake, influencing cellular processes necessary for collagen synthesis. While insulin’s primary role is glucose management, its involvement in other metabolic pathways, including collagen metabolism, is worth further investigation. Imbalances in insulin response can disrupt the delicate balance of these processes, affecting the overall absorption and utilization of collagen.
Figuring out the best time to take collagen can be tricky, but it’s important for overall health. While there’s no single “perfect” time, optimizing your routine can make a real difference. This is especially true when considering how your collagen intake might interact with other aspects of your health, like access to type 2 diabetes care. Ultimately, discussing your specific needs with a healthcare professional is key to finding the best collagen-taking schedule for you.
Remember, consistency is key when it comes to seeing results, regardless of the time of day you choose to take your collagen supplement.
Maintaining healthy blood sugar levels is essential to ensure that collagen supplements are utilized effectively.
Potential Effects of Different Blood Sugar Levels on Collagen Absorption
| Blood Sugar Level | Potential Effect on Collagen Absorption | Example |
|---|---|---|
| High (Hyperglycemia) | Reduced absorption due to interference with nutrient utilization, possible diversion of resources away from collagen synthesis. | A person with uncontrolled diabetes might experience less benefit from collagen supplements compared to someone with stable blood sugar. |
| Low (Hypoglycemia) | Potentially reduced absorption due to the body prioritizing glucose utilization, and possible stress hormone influence on collagen metabolism. | A person with frequent episodes of hypoglycemia may experience less collagen utilization. |
| Stable (Normal) | Optimal absorption and utilization of collagen supplements, allowing for effective metabolic processes for collagen utilization. | A person with healthy blood sugar levels is more likely to experience the full benefits of collagen supplements. |
Collagen Absorption and Digestive Enzymes

Collagen, a crucial protein for skin health, hair growth, and joint function, needs to be broken down by the body to be absorbed and utilized effectively. This process is significantly influenced by digestive enzymes, specialized proteins that facilitate the breakdown of large molecules into smaller, absorbable components. Understanding the interplay between collagen and digestive enzymes is vital for maximizing the benefits of collagen supplementation.The body’s digestive system plays a vital role in breaking down collagen into smaller peptides and amino acids, which can then be absorbed into the bloodstream.
Digestive enzymes are the catalysts that initiate this breakdown process. Without sufficient enzyme activity, collagen may not be fully broken down, leading to reduced absorption and diminished effectiveness. This is particularly relevant for those with compromised digestive function or those taking collagen supplements in an effort to address specific health concerns.
Relationship Between Digestive Enzymes and Collagen Absorption
Digestive enzymes are essential for the hydrolysis of collagen, a complex protein. Hydrolysis involves the breakdown of collagen’s peptide bonds, making its constituent amino acids accessible for absorption. Enzymes like pepsin, trypsin, and chymotrypsin, produced naturally in the stomach and small intestine, play a crucial role in this process. These enzymes target specific sequences within the collagen molecule, promoting its degradation into absorbable fragments.
This efficient breakdown allows the body to effectively utilize the collagen for its intended purposes.
Importance of Digestive Enzymes in Collagen Breakdown
Adequate digestive enzyme activity is critical for efficient collagen absorption. Without sufficient enzymes, the collagen molecule may not be adequately broken down, resulting in incomplete absorption. This incomplete absorption can lead to a decreased bioavailability of collagen, limiting its potential benefits. In cases where digestive enzyme production is reduced due to age or certain health conditions, supplementing with digestive enzymes may enhance collagen absorption and maximize its effectiveness.
Role of Different Types of Digestive Enzymes
Various types of digestive enzymes contribute to the overall process of collagen breakdown. Proteases, a broad category of enzymes that break down proteins, are especially important in this context. Specific proteases like pepsin, trypsin, and chymotrypsin are crucial for hydrolyzing collagen. These enzymes work in conjunction to ensure the efficient breakdown of the collagen molecule. Other enzymes, such as lactase and lipase, aid in the overall digestive process and may indirectly affect collagen absorption by creating a favorable environment for optimal protease function.
Comparison of Digestive Enzyme Supplements on Collagen Absorption, Best time to take collagen
| Enzyme Supplement | Mechanism of Action | Potential Effectiveness on Collagen Absorption | Considerations |
|---|---|---|---|
| Pepsin | Breaks down proteins in the stomach | High potential for early stage collagen breakdown | Effectiveness may vary depending on individual stomach acid production |
| Trypsin | Breaks down proteins in the small intestine | High potential for further collagen breakdown | Effectiveness is dependent on sufficient pancreatic enzyme production |
| Chymotrypsin | Breaks down specific protein sequences | High potential for targeted collagen breakdown | May be less effective than trypsin in certain situations |
| Broad-spectrum protease blend | Combines multiple protease types | Potentially high effectiveness due to combined action | Effectiveness depends on the specific enzymes included and their concentrations |
The effectiveness of digestive enzyme supplements on collagen absorption can vary significantly depending on factors such as the specific enzymes included, the dosage, and individual digestive health. More research is needed to definitively quantify the impact of various enzyme supplements on collagen absorption.
Influence of Other Nutrients on Collagen Absorption
Collagen synthesis and absorption aren’t isolated events; they’re intricately linked to the availability and interplay of other nutrients in the body. Understanding these relationships is crucial for maximizing the benefits of collagen supplementation. Optimizing the absorption of collagen often involves considering the broader nutritional landscape.The effectiveness of collagen absorption isn’t solely determined by the collagen supplement itself. Other nutrients play a vital role in supporting the body’s ability to utilize collagen effectively.
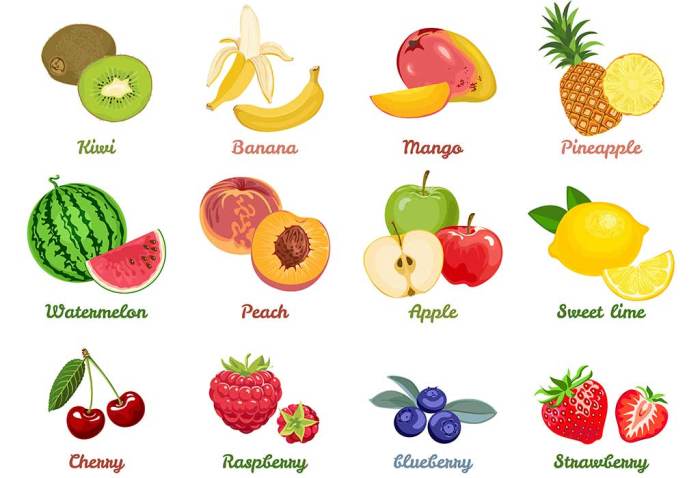
These nutrients can either enhance or hinder the absorption process, depending on their presence and interaction within the body. For instance, adequate vitamin C is essential for collagen synthesis, directly influencing the body’s ability to process and utilize collagen.
Vitamins Supporting Collagen Absorption
Vitamin C is a key player in collagen synthesis. It’s a crucial cofactor in the enzymatic processes that build collagen fibers. Without sufficient vitamin C, collagen synthesis slows down, affecting the body’s overall ability to absorb and utilize collagen effectively. Other vitamins, such as Vitamin K and Vitamin A, also contribute to healthy connective tissues, supporting the overall process of collagen absorption and utilization.
Adequate levels of these vitamins are important for optimal collagen synthesis.
Minerals and Collagen Absorption
Minerals such as zinc and copper are vital for collagen synthesis. These minerals are involved in the enzymatic reactions that create and maintain collagen. A deficiency in these minerals can impede the collagen production process, ultimately affecting the body’s capacity to absorb collagen. Adequate intake of these minerals can improve collagen absorption.
Protein’s Impact on Collagen Absorption
Protein plays a crucial role in collagen absorption. Sufficient protein intake provides the building blocks necessary for collagen synthesis. Without adequate protein, the body might struggle to utilize collagen effectively, impacting absorption. A balanced protein intake, alongside collagen supplements, could potentially enhance the effectiveness of the supplement.
Impact of Nutrient Deficiencies
Nutrient deficiencies can significantly hinder collagen absorption. For instance, a lack of vitamin C can lead to weakened connective tissues and impaired collagen synthesis. Similarly, insufficient protein or minerals like zinc and copper can disrupt the process, reducing the effectiveness of collagen supplements. Understanding these deficiencies is important to ensure adequate intake of supporting nutrients.
Combining Nutrients for Enhanced Absorption
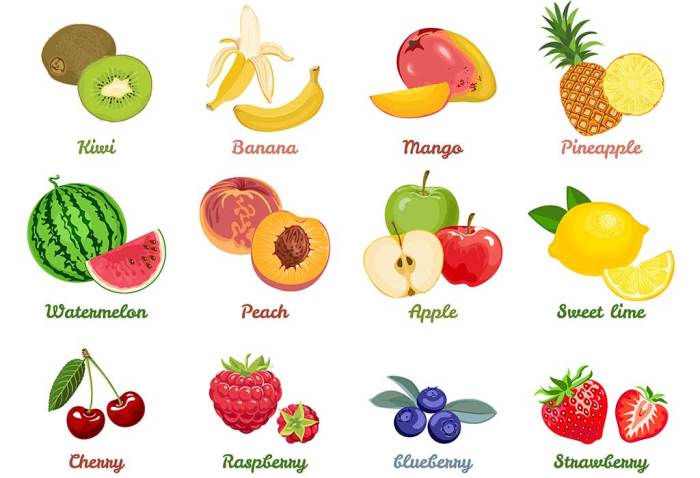
Combining collagen supplements with other supporting nutrients can potentially improve absorption. For example, consuming collagen supplements with foods rich in vitamin C (like citrus fruits) or with a protein-rich meal can enhance the body’s ability to utilize the collagen effectively. This approach helps to optimize the absorption process.
Example of Supplementation Strategy
| Nutrient | Source | Benefit |
|---|---|---|
| Vitamin C | Citrus fruits, berries | Essential cofactor in collagen synthesis |
| Protein | Lean meats, poultry, fish, eggs | Provides building blocks for collagen synthesis |
| Zinc | Oysters, beef, pumpkin seeds | Supports enzymatic reactions in collagen synthesis |
A well-balanced diet that includes a variety of nutrient-rich foods, alongside a collagen supplement, can contribute to optimal collagen absorption and overall health.
Optimal Time of Day for Collagen Intake
Collagen supplementation has gained popularity for its potential benefits in maintaining healthy skin, joints, and overall well-being. However, the optimal time for taking collagen isn’t universally agreed upon. Factors like individual metabolism, dietary habits, and even circadian rhythms can play a role in how effectively your body absorbs and utilizes collagen. Understanding these nuances can help you maximize the benefits of your collagen regimen.The absorption of collagen, like other nutrients, is influenced by several factors, including the presence of other nutrients in your meal, digestive enzyme activity, and the overall state of your digestive system.
The timing of collagen intake in relation to other meals and activities can impact its bioavailability.
Factors Influencing Optimal Intake Time
Several factors can influence the best time to take collagen supplements. These factors include your individual metabolism, current health status, and even the specific type of collagen you’re using. Some forms of collagen are more readily absorbed than others.
Relationship Between Circadian Rhythms and Collagen Absorption
Our bodies operate on a natural 24-hour cycle known as the circadian rhythm. This internal clock affects various physiological processes, including digestion, nutrient absorption, and cellular repair. Research suggests that certain times of day may be more conducive to collagen absorption due to the interplay between these circadian rhythms and digestive processes. For example, peak digestive enzyme activity might coincide with specific meal times, potentially influencing collagen absorption.
Examples of Optimal Times for Collagen Intake Based on Individual Needs
Determining the ideal time for collagen intake requires considering individual needs and preferences. Someone who prioritizes morning skin care might find that taking collagen in the morning supports their skincare routine. Alternatively, an individual focused on joint health might find that taking collagen with their evening meal aids in supporting their joints during sleep. Generally, taking collagen with a meal that includes protein and other essential nutrients can improve absorption.
Table: Potential Effects of Different Times of Day on Collagen Absorption and Utilization
| Time of Day | Potential Effects on Absorption and Utilization | Considerations |
|---|---|---|
| Morning (with breakfast) | Enhanced absorption due to increased digestive enzyme activity. May support morning skin care routines. | May be ideal for individuals who prioritize skin health. |
| Afternoon (with lunch) | Good absorption, aligning with a midday meal. May support general well-being. | A suitable option for individuals who want to integrate collagen into their lunch routine. |
| Evening (with dinner) | Potential for enhanced absorption with a balanced dinner, aiding joint health and overall well-being. May be less disruptive to sleep if taken with a meal. | May be beneficial for individuals who want to support joint health while aiding sleep. |
| Between meals | May be less effective as absorption might be lower without a meal to facilitate it. | Consider combining with a small snack if taken between meals. |
Individual Variations in Collagen Absorption

Collagen, a crucial protein for skin elasticity, joint health, and overall well-being, isn’t absorbed uniformly by everyone. Several individual factors play a significant role in how effectively your body processes and utilizes collagen supplements. Understanding these factors is key to optimizing collagen intake and achieving desired results.Individual differences in collagen absorption are multifaceted, influenced by a range of factors beyond just the timing of intake.
Age, genetics, underlying health conditions, and even lifestyle choices can all impact how well your body assimilates collagen. Adjusting your approach to collagen supplementation based on these individual needs can significantly enhance its effectiveness.
Impact of Age on Collagen Absorption
Age-related changes in digestive function and overall metabolic rate can affect collagen absorption. Younger individuals generally exhibit more efficient nutrient absorption, including collagen. As we age, the efficiency of the digestive system may decline, potentially leading to reduced collagen absorption. This is not an absolute rule, but it’s a consideration when adjusting your intake strategy. For example, a 20-year-old might see quicker results from a lower daily dose compared to a 60-year-old who might require a slightly higher dose to achieve the same benefits.
Influence of Genetics on Collagen Absorption
Genetic variations in nutrient metabolism can influence how your body processes collagen. Some individuals might have a genetic predisposition to more efficient collagen absorption, while others might not. This genetic component can impact how much collagen is absorbed and utilized by the body, affecting the overall response to supplementation. There is ongoing research exploring the genetic basis of collagen metabolism, which could provide further insights in the future.
Effect of Health Conditions on Collagen Absorption
Certain health conditions can directly impact nutrient absorption, including collagen. For instance, individuals with digestive disorders like Crohn’s disease or celiac disease may experience reduced absorption of collagen, as well as other nutrients. Similarly, individuals with impaired gut health, often characterized by leaky gut syndrome, may also have difficulty absorbing collagen. In such cases, consulting a healthcare professional is crucial to determine the best course of action.
Lifestyle Factors and Collagen Absorption
Lifestyle choices, such as diet and exercise, can also influence collagen absorption. A diet lacking essential nutrients, such as vitamin C, can hinder collagen synthesis and absorption. Consistent exercise, on the other hand, can promote overall health and potentially enhance the absorption of collagen.
Table Summarizing Potential Impact of Individual Factors on Collagen Absorption
| Individual Factor | Potential Impact on Collagen Absorption |
|---|---|
| Age | Absorption efficiency may decrease with age due to changes in digestive function and metabolic rate. |
| Genetics | Genetic variations in nutrient metabolism may influence how well collagen is processed. |
| Health Conditions (e.g., digestive disorders) | Certain conditions can impede nutrient absorption, including collagen. |
| Lifestyle Factors (e.g., diet, exercise) | A nutrient-deficient diet can hinder collagen absorption. Exercise may enhance overall absorption. |
Comparing Different Collagen Supplement Forms
Choosing the right collagen supplement can be tricky, as different forms offer varying advantages and disadvantages. The form of your supplement, whether powder, capsules, or gummies, can impact its absorption rate and overall effectiveness. This section will explore the distinct characteristics of each form, helping you understand which might be the best fit for your needs.The absorption rate of collagen, while generally good, can be influenced by various factors, including the form of the supplement.
Figuring out the best time to take collagen supplements can be tricky, but it’s a good idea to consider your overall health goals. While focusing on optimal collagen intake is important, understanding the severity of illnesses like the flu is equally crucial. Recent studies suggest that the flu can be surprisingly dangerous, especially for vulnerable populations. How deadly is the flu depends on several factors, so always consult your doctor.
Ultimately, consistency with a healthy routine, including the proper timing for your collagen supplements, is key to long-term well-being.
Different forms present unique challenges and benefits in terms of digestion and bioavailability. Understanding these differences can help you select the most suitable collagen supplement to support your individual needs and goals.
Powder Form
Collagen powder is a popular choice due to its versatility and typically lower cost. It’s easily mixed into various beverages or foods, allowing for convenient consumption.
- Pros: Powdered collagen is often the most cost-effective form. It’s highly customizable, allowing you to control the dosage and mix it with your preferred beverages or foods. Many find the taste neutral, making it easy to incorporate into their daily routine.
- Cons: Powdered collagen can be messy to measure and mix, potentially leading to inaccurate dosing. It may require more effort to consume compared to capsules or gummies, and some individuals may experience a slight gritty texture in their drinks. Absorption can also vary depending on the specific preparation and the individual’s digestive system.
Capsule Form
Collagen capsules offer a convenient, measured dose, minimizing the preparation time associated with powders.
- Pros: Capsules are convenient and easy to swallow, eliminating the need for mixing and ensuring a consistent dosage. They are often more discreet compared to powders. The gelatin capsules themselves may be a source of collagen, enhancing overall intake.
- Cons: Capsules may contain fillers or additives that could affect absorption or cause digestive discomfort in some individuals. The absorption rate of collagen in capsules might be slightly lower compared to powdered collagen. The cost per serving may be higher than powder.
Gummy Form
Collagen gummies are a palatable option, especially for individuals who find traditional supplement forms less appealing.
- Pros: Gummies are a tasty and appealing way to consume collagen, potentially making it easier for individuals to maintain a consistent intake. They can be particularly helpful for children or those who struggle to swallow pills.
- Cons: Gummies typically have a higher sugar content compared to powder or capsules, which could be a concern for those with dietary restrictions or blood sugar concerns. The dosage accuracy might not be as precise as with capsules or powders, and the cost per serving is usually higher than powder.
Form Influence on Timing
The chosen form of collagen can slightly influence the best time to take it. For example, if using a powdered form, mixing it into a morning smoothie might be convenient. If capsules are preferred, taking them with a meal might help with absorption. The presence of digestive enzymes or other nutrients can also play a role.
Examples of Form Suitability
A busy professional might find capsules convenient for on-the-go consumption, whereas an athlete aiming for a precise daily dose might prefer the customizability of powder. Individuals with specific dietary restrictions might find the gummy form less suitable due to the higher sugar content.
Comparison Table
| Form | Pros | Cons |
|---|---|---|
| Powder | Cost-effective, customizable, often neutral taste | Messy to measure, potential for inaccurate dosing, slightly gritty texture |
| Capsule | Convenient, easy to swallow, measured dose | Potential fillers/additives, potentially lower absorption, higher cost per serving |
| Gummy | Palatable, easy for children/those who dislike pills | Higher sugar content, less precise dosage, higher cost per serving |
Scientific Evidence on Best Time to Take Collagen
While anecdotal evidence abounds about the best time to take collagen supplements, scientific research provides a more nuanced understanding. Numerous factors influence collagen absorption, making a one-size-fits-all approach problematic. This section delves into the scientific studies investigating collagen absorption and timing, outlining key findings and limitations.Understanding the limitations of existing studies is crucial to interpreting their results effectively.
These studies often have small sample sizes, use different collagen types and formulations, and may not account for individual variations in digestion and metabolism. This means the results may not universally apply to everyone, and further research is needed to confirm these findings and address the limitations.
Collagen Absorption and Meal Timing Studies
Research on collagen absorption and meal timing is ongoing, with mixed results. Some studies suggest that taking collagen with a meal might enhance absorption, while others show no significant difference in absorption whether taken with or without food. The impact of meal timing on collagen effectiveness remains an area of active investigation.
- One study observed improved collagen absorption when taken with a meal rich in vitamin C. This is likely due to vitamin C’s role in collagen synthesis. This indicates that specific dietary components can influence the absorption of collagen, but the optimal meal type needs further exploration.
- Another study found no significant difference in collagen bioavailability between taking it before or after meals. This suggests that the time of day for collagen supplementation might not be as crucial as other factors, like the overall dietary intake.
Relationship Between Blood Sugar and Collagen Absorption
The interplay between blood sugar levels and collagen absorption is an area of ongoing research. High blood sugar levels might potentially affect the body’s ability to utilize collagen effectively.
- Studies examining the effect of blood sugar on collagen absorption are still limited. However, some evidence suggests that maintaining stable blood sugar levels through a balanced diet might be beneficial for optimizing collagen absorption.
Summary of Findings
| Study Focus | Key Findings | Limitations |
|---|---|---|
| Collagen absorption with meals | Some studies show enhanced absorption with meals, others show no significant difference. | Varied collagen types, formulations, and sample sizes. |
| Blood sugar and collagen absorption | Limited research, but evidence suggests stable blood sugar might be beneficial. | Small sample sizes and need for more extensive studies. |
Application to the General Population
The current scientific evidence on the optimal time to take collagen is still developing. While some studies hint at potential benefits of taking collagen with meals or maintaining stable blood sugar, definitive conclusions remain elusive. Individuals should consult with healthcare professionals before making significant dietary changes, especially if they have underlying health conditions.
Epilogue: Best Time To Take Collagen
In conclusion, optimizing collagen absorption is a personalized journey. While the ideal time for taking collagen may vary based on individual factors, the key takeaway is to tailor your approach to your body’s unique needs. By considering factors like meal timing, blood sugar levels, and digestive health, you can maximize the effectiveness of your collagen supplement routine. This personalized approach ensures that you’re getting the most out of your collagen investment and supporting your body’s natural collagen production.