Autism test for adults is a crucial step for understanding and navigating the complexities of autism spectrum disorder (ASD) in adulthood. Accurate diagnosis empowers individuals to access appropriate support and resources, leading to improved well-being and quality of life. However, the process can be challenging, with various assessment methods, considerations for co-occurring conditions, and the need for culturally sensitive practices.
This comprehensive guide explores the intricacies of adult autism testing, from understanding the different assessment types and processes to interpreting results and finding support resources. We’ll also delve into the challenges adults face in seeking testing and the profound impact a diagnosis can have on their lives.
Introduction to Adult Autism Testing
Adult autism spectrum disorder (ASD) is a complex neurodevelopmental condition that can manifest differently in adults than in children. Individuals with ASD often experience challenges with social communication and interaction, repetitive behaviors, and restricted interests. These traits can impact various aspects of adult life, including employment, relationships, and daily routines. Understanding these challenges is crucial for providing appropriate support and resources.Accurate diagnosis of autism in adults is vital for accessing necessary interventions and support services.
A proper diagnosis allows individuals to better understand their strengths and challenges, leading to improved self-awareness and coping strategies. This understanding empowers adults to navigate social situations, manage their behaviors, and participate more fully in their communities.
Importance of Accurate Diagnosis for Adults
An accurate diagnosis empowers adults with ASD to access tailored support services. This includes therapies focused on social skills, communication, and behavioral management. Furthermore, a diagnosis opens doors to accommodations in educational, employment, and social settings, facilitating greater independence and participation.
Challenges of Diagnosing Autism in Adults
Diagnosing autism in adults presents unique challenges compared to diagnosing children. Often, the subtle, nuanced presentation of symptoms can be missed or misattributed to other conditions. Additionally, individuals may have developed coping mechanisms over time that mask the core characteristics of ASD. This can make identification more difficult. Past experiences and societal expectations can also contribute to the challenge of diagnosis, as individuals may not identify themselves as needing support.
Common Reasons Why Adults Seek Testing
Adults seek autism testing for a variety of reasons. They may experience difficulties in social situations, such as struggling to understand social cues or maintain conversations. Some individuals may have repetitive behaviors or routines that cause distress or interfere with daily functioning. Problems with communication, such as difficulty expressing needs or understanding others, can also lead individuals to seek assessment.
Relationship difficulties, occupational challenges, and personal dissatisfaction can also motivate adults to seek an autism evaluation.
Types of Assessments Used for Adults
A variety of assessment tools are used to evaluate autism in adults. These assessments typically involve a comprehensive evaluation of the individual’s social communication, repetitive behaviors, restricted interests, and overall functioning. A clinical interview provides insight into the individual’s history, current challenges, and coping mechanisms. Standardized questionnaires are frequently used to gather detailed information about the individual’s behaviors and experiences.
Observations of the individual’s behavior in a structured setting, such as a clinic or testing environment, are critical to the evaluation process. These various methods provide a more holistic picture of the individual’s presentation, ensuring an accurate diagnosis.
Types of Adult Autism Assessments
Understanding adult autism requires a nuanced approach, going beyond simple checklists. Various assessment methods exist, each with its own strengths and weaknesses. This exploration delves into the diverse landscape of assessments, offering a comparative analysis to help you better understand the process.Different assessment methods cater to different needs and provide varying levels of detail. Choosing the right assessment depends on the specific goals of the evaluation, the individual’s background, and the context of the assessment.
Some methods focus on behavioral observations, while others emphasize self-reported experiences.
Standardized Assessments
Standardized assessments, like the Autism Diagnostic Observation Schedule (ADOS), provide a structured and reliable method for evaluating autistic traits. These assessments use predetermined criteria and scoring systems, ensuring consistency across different examiners and settings. Their structured nature makes them useful for diagnosing autism in various contexts.
Semi-Structured Interviews
Semi-structured interviews, such as the Autism Diagnostic Interview-Revised (ADI-R), offer a more flexible approach. These interviews allow for exploration of specific behaviors and experiences related to autism in a more conversational format. They provide valuable insights into the individual’s perspective and can uncover nuanced details that might be missed in standardized assessments.
Behavioral Observation Scales
Behavioral observation scales offer a direct way to observe behaviors associated with autism. These scales focus on observing specific behaviors in a natural setting, such as during play or interaction. These assessments are especially helpful in identifying the impact of autism on daily life and social interactions. They provide a comprehensive picture of the individual’s functional skills and challenges.
Self-Report Questionnaires
Self-report questionnaires, like the AQ-10, are a more self-directed approach. They rely on the individual’s own perception and self-assessment of their experiences and behaviors. While valuable for providing a personal perspective, these questionnaires may be less objective and reliable for individuals with certain cognitive or communication challenges. They can offer a good starting point but should be combined with other assessment methods for a comprehensive evaluation.
Table of Assessment Methods
| Method Name | Target Age Range | Testing Duration | Key Features |
|---|---|---|---|
| Autism Diagnostic Observation Schedule (ADOS) | 18 months – adulthood | Variable, typically 30-60 minutes | Standardized, structured observation of social interaction and communication; multiple modules for varying ages and needs. |
| Autism Diagnostic Interview-Revised (ADI-R) | 5 – 55 years | Variable, typically 1-2 hours | Semi-structured interview focusing on developmental history and specific behaviors. |
| Behavioral Observation Scales (e.g., Social Responsiveness Scale) | 2 – adult | Variable, typically 30-60 minutes | Focus on observable behaviors in natural settings; often used for supporting diagnosis and understanding the impact of autism on daily life. |
| Self-Report Questionnaires (e.g., AQ-10) | 16 – adult | Variable, typically 15-30 minutes | Individual’s self-perception of autistic traits; may require adaptation for individuals with communication or cognitive differences. |
Assessment Process and Procedures

Navigating the world of autism assessments can feel like stepping into a labyrinth. Understanding the steps involved, the roles of various professionals, and the preparation required for both the assessor and the assessed can ease anxiety and ensure a smoother process. This section will demystify the assessment journey, offering clarity and insight into each stage.The assessment process for adult autism is a multifaceted journey, designed to gather comprehensive information about an individual’s strengths, challenges, and experiences.
It’s crucial to remember that every assessment is tailored to the individual, taking into account their unique circumstances and needs. The process is designed to be supportive and informative, aiming to provide a thorough understanding of the individual’s situation.
Pre-Assessment Phase
This initial stage involves crucial preparations to ensure the assessment’s validity and reliability. It’s a period of groundwork, laying the foundation for a productive and meaningful assessment. A comprehensive intake form, interviews, and review of existing documentation form the bedrock of this phase.
- Gathering background information through interviews with the individual and their family/support network. This helps build a complete picture of their history, development, and current functioning.
- Reviewing relevant records, such as medical reports, educational records, and previous assessment reports, if available. This step ensures that the assessment considers the individual’s entire history and any previous diagnoses.
- Establishing clear communication channels and expectations between the assessor, the assessed, and any involved support personnel. Open communication fosters trust and ensures everyone is on the same page regarding the assessment goals.
Assessment Phase
The assessment phase is the core of the process, encompassing a variety of tools and techniques. Different instruments are employed to gauge various aspects of the individual’s functioning.
- Administering standardized assessments to evaluate social communication, repetitive behaviors, and other relevant areas. Examples of these assessments might include the Autism Diagnostic Observation Schedule (ADOS), the Autism Diagnostic Interview-Revised (ADI-R), or other validated tools.
- Conducting clinical interviews to gain insight into the individual’s subjective experiences, perspectives, and personal narratives. This qualitative component complements the quantitative data gathered from standardized tests.
- Observing the individual in various settings, such as a clinical environment or a natural setting, to gain a richer understanding of their behavior and interaction patterns. Observations provide a dynamic and nuanced perspective on their strengths and challenges.
Post-Assessment Phase
This stage focuses on synthesizing the collected data, providing feedback, and outlining recommendations. It’s a period of interpretation and application.
- Thorough analysis of the assessment data, combining information from various sources and employing clinical judgment. This step is critical in determining the presence or absence of autism spectrum disorder (ASD).
- Developing a comprehensive report that summarizes the findings, including strengths, challenges, and recommendations for support. This report is a crucial document that informs the individual’s care plan and treatment.
- Providing feedback to the individual and their support system, clearly explaining the assessment results and recommendations. Open communication is vital for understanding the implications of the findings and for developing a supportive plan.
Roles of Professionals
Different professionals play vital roles in the assessment process. Each brings unique expertise to the table, ensuring a comprehensive understanding of the individual.
- Psychiatrists, psychologists, and other mental health professionals are crucial in the diagnostic process. Their expertise is invaluable in assessing and interpreting the results.
- Occupational therapists, speech-language pathologists, and other specialists contribute to a comprehensive understanding of the individual’s needs and support requirements.
- Caregivers and family members provide valuable insights into the individual’s daily life, behaviors, and experiences. Their perspective is critical in the assessment process.
Preparations for the Assessment
Preparation is key for both the assessor and the assessed. Clear expectations and appropriate strategies can make the process more manageable.
- For the Assessed: Relaxation techniques, clear communication with the assessment team, and a supportive environment are important. Preparation can involve familiarizing themselves with the assessment process and practicing relaxation techniques.
- For the Assessor: Thorough preparation includes reviewing relevant literature, familiarizing themselves with assessment tools, and creating a comfortable and supportive environment. This ensures a well-structured and productive assessment.
Assessment Stages and Tasks
| Stage | Tasks |
|---|---|
| Pre-Assessment | Gathering background information, reviewing records, establishing communication channels |
| Assessment | Administering standardized assessments, conducting clinical interviews, observing behaviors |
| Post-Assessment | Analyzing data, developing a report, providing feedback |
Interpreting Assessment Results
Understanding the results of an autism assessment for adults is a crucial step in providing appropriate support and interventions. It’s not simply about identifying the presence or absence of autism; the interpretation delves into the nuances of the individual’s strengths, challenges, and specific needs. A thorough interpretation considers not only the test scores but also the individual’s life history, experiences, and overall functioning.The process of interpreting results goes beyond a simple numerical score.
It requires a skilled professional to synthesize the data, evaluate the context, and consider the person as a whole. The goal is to develop a comprehensive understanding of the individual’s profile, which will inform personalized strategies for success.
Common Test Results and Their Implications
Interpreting test results involves looking at patterns of responses across different tasks. A high score on a specific area, like social communication, might suggest relative strengths in that domain. Conversely, a low score might point towards challenges and specific areas where support is needed. For example, consistently lower scores on tasks related to understanding nonverbal cues might suggest difficulties in social interactions.
Considering Various Factors in Interpretation
Interpreting assessment results isn’t just about the numbers; it’s about considering the individual’s whole story. Factors such as cultural background, learning style, and previous life experiences can influence performance on the assessment. A person’s current emotional state and motivation also play a significant role. This comprehensive perspective ensures a more accurate and personalized understanding of the individual’s profile.
Co-occurring Conditions and Considerations
Many individuals with autism spectrum disorder (ASD) also experience co-occurring conditions like anxiety, depression, or learning disabilities. These conditions can significantly impact test results and should be considered in the interpretation. For instance, anxiety might lead to test-taking difficulties, affecting performance on tasks requiring social interaction or rapid responses. A thorough evaluation considers these potential influences to create a more accurate and complete picture.
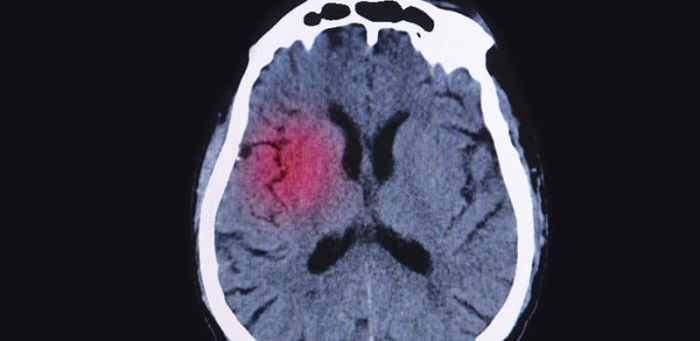
Finding an autism test for adults can be tricky, but understanding potential neurological connections is key. For example, some research suggests overlaps between neurological conditions like autism and conditions such as migraine and multiple sclerosis. Exploring the fascinating migraine and multiple sclerosis connection might offer clues, ultimately helping us better understand the complexities of autism testing and diagnosis in adults.
Example of a Sample Test Result Summary
| Category | Score | Interpretation |
|---|---|---|
| Social Communication | 75 | Moderate difficulty with social communication skills, potentially requiring targeted support. |
| Repetitive Behaviors | 90 | Relatively low levels of repetitive behaviors. |
| Sensory Sensitivity | 88 | Moderate sensory sensitivity, requiring accommodations in the environment. |
| Executive Functioning | 65 | Significant challenges with executive functioning, impacting planning and organization. |
This table presents a simplified example. A complete assessment report would include detailed descriptions and explanations for each category, providing a nuanced understanding of the individual’s strengths and challenges. It’s crucial to remember that these are just examples, and actual results and interpretations should always be reviewed and discussed with a qualified professional.
Resources and Support for Adults with Autism

Navigating the world with autism can be challenging, but it’s also incredibly rewarding. Having access to the right resources and support is crucial for adults with autism to thrive. This section Artikels the various avenues of support available, from finding supportive communities to understanding the therapeutic options that can help.
Support Groups and Organizations
Understanding and connecting with others who share similar experiences is invaluable. Support groups and organizations dedicated to autism provide a safe space for adults to connect, share their stories, and learn from one another. These groups offer practical advice, emotional support, and a sense of belonging.
Taking an autism test for adults can be a really insightful journey, but it’s important to remember that it’s not just about ticking boxes. Sometimes, navigating the complexities of personal health choices, like choosing non hormonal birth control options, can be a part of that process. Ultimately, understanding your unique needs and circumstances is key when considering an autism test for adults, especially since many factors contribute to a thorough and accurate diagnosis.
- National Autistic Society (UK): This organization offers a wide range of support services, including online forums, local support groups, and publications. They are a valuable resource for navigating the complexities of autism and accessing appropriate support services.
- Autism Speaks (USA): A prominent organization dedicated to autism research, advocacy, and support. Autism Speaks provides resources for families and individuals, including support groups, educational materials, and information on current research.
- Autistic Self Advocacy Network (ASAN): ASAN is a grassroots organization led by autistic adults. They advocate for the rights and needs of autistic individuals, promoting self-advocacy and inclusion.
Therapy Options
Various therapeutic approaches can be highly beneficial for adults with autism. The right therapy can help individuals develop coping mechanisms, improve social skills, and enhance overall well-being.
- Applied Behavior Analysis (ABA): ABA therapy focuses on changing behaviors through positive reinforcement and structured learning. It can be particularly effective in improving communication, social interaction, and daily living skills. ABA therapy often involves intensive, one-on-one sessions with a trained therapist. For example, an individual with autism may struggle with initiating conversations; ABA therapy could focus on teaching them specific prompts and strategies for initiating and maintaining conversations.
- Cognitive Behavioral Therapy (CBT): CBT helps individuals identify and change negative thought patterns and behaviors. It can be valuable for managing anxiety, depression, and other mental health challenges that are often associated with autism. For example, a person with autism might experience social anxiety; CBT can help them develop strategies for managing those anxieties and building social confidence.
- Occupational Therapy (OT): OT addresses practical challenges related to daily living, such as sensory processing issues, motor skills, and organization. An OT can help individuals develop strategies to improve their daily routines and adapt to different environments.
Support Services for the Diagnostic Process
Navigating the diagnostic process for autism can be daunting. There are resources available to support adults throughout this journey.
- Advocacy groups, such as those mentioned above, can provide guidance and support in understanding the process and in finding appropriate professionals. They can often offer recommendations and information about potential diagnostic assessments and testing facilities.
- Support groups for individuals undergoing autism assessments can provide valuable encouragement and reassurance. The shared experiences within these groups can help lessen the stress and anxiety often associated with this process.
Individualized Support Plans
Recognizing the diverse needs of adults with autism is paramount. Individualized support plans are crucial for tailoring interventions and resources to meet each person’s unique requirements.
- These plans should consider the individual’s strengths, weaknesses, and preferences. They should incorporate specific goals and objectives, along with strategies for achieving them. For example, one person might focus on improving communication skills, while another might concentrate on developing organizational strategies.
- The plan should be flexible and adaptable to accommodate changing needs and circumstances. Regular review and adjustments are essential to ensure the plan remains relevant and effective. This can involve collaborating with therapists, family members, and support workers to continuously monitor and adapt the support plan as needed.
Potential Support Organizations
- Autism Self Advocacy Network (ASAN)
- National Autistic Society (UK)
- Autism Speaks (USA)
- Local autism support groups
- University-based autism research centers
Challenges and Considerations
Navigating the path to an autism diagnosis can be fraught with challenges, particularly for adults. Understanding these obstacles is crucial for creating a supportive and effective assessment process. Adults may face unique barriers, such as a lack of awareness of autism traits in themselves, a history of misdiagnosis or dismissal, or simply a lack of access to appropriate resources.
Furthermore, societal and cultural factors can significantly influence the experience of seeking and receiving an autism diagnosis.The journey toward an autism diagnosis can be complicated by various factors. It is essential to acknowledge the multifaceted nature of these challenges to create a more inclusive and accurate assessment framework.
Common Challenges Faced by Adults Seeking Testing
Adults seeking autism testing may encounter various hurdles. These might include a lack of self-awareness of autistic traits, a history of misdiagnosis or invalidation, or the difficulty in recognizing and expressing their needs within the assessment process. Financial constraints, geographical limitations, and the time commitment required can also present significant obstacles. Furthermore, some adults may be hesitant to undergo testing due to potential emotional distress or social stigma associated with a diagnosis.
Social and Cultural Factors Influencing Diagnosis
Societal and cultural norms profoundly impact how autism is perceived and diagnosed. Cultural expectations regarding behavior and emotional expression can influence how individuals present themselves, potentially masking or exacerbating autistic traits. Differences in communication styles and social cues across cultures can also lead to misinterpretations during assessment. Furthermore, a lack of awareness and acceptance of autism within certain cultural contexts can discourage individuals from seeking testing or lead to delayed diagnosis.
Potential Biases in Assessment Methods
Assessment methods for autism may contain implicit biases that can affect the accuracy of the diagnosis. These biases can stem from the cultural background of the assessor, their own personal experiences, or preconceived notions about autism. Furthermore, assessment tools may not be equally effective or appropriate for individuals from diverse cultural backgrounds. A lack of cultural sensitivity in the assessment process can lead to inaccurate diagnoses or a failure to identify the unique needs of individuals from diverse backgrounds.
For instance, a test relying heavily on verbal communication might not be suitable for individuals with non-verbal or less verbal communication styles.
Need for Culturally Sensitive Assessment Practices
Culturally sensitive assessment practices are essential for accurate and equitable diagnosis. These practices should consider the individual’s cultural background, values, and beliefs to ensure that the assessment process is relevant and meaningful. This includes using culturally appropriate communication styles, ensuring that the assessment environment is comfortable and respectful, and utilizing assessment tools that reflect the diversity of human experiences.
Furthermore, culturally competent assessors can better understand and interpret the unique expressions of autism within different cultural contexts.
Cultural Considerations in Autism Assessment
“Cultural sensitivity in autism assessment necessitates a deep understanding of the diverse ways in which individuals express autistic traits within various cultural contexts. Assessment tools should be adaptable to diverse communication styles, social norms, and behavioral expectations. Moreover, assessors must be aware of their own potential biases and actively work to mitigate their impact on the diagnostic process.”
Impact of a Diagnosis
The news of an autism diagnosis can be profound, triggering a whirlwind of emotions and questions. Understanding the potential impacts, both positive and negative, is crucial for navigating this new chapter. This section explores how an autism diagnosis can affect self-perception, relationships, and opportunities, emphasizing the importance of support and resources for adults facing this journey.The experience of receiving an autism diagnosis is highly personal.
While the process can be challenging, it also presents opportunities for self-discovery and growth. The key is to acknowledge the emotional complexities and utilize available support to effectively navigate the changes. Ultimately, a diagnosis is a tool for understanding, not a defining label.
Potential Positive Impacts of an Autism Diagnosis
Receiving an autism diagnosis can unlock a wealth of self-understanding and acceptance. This newfound understanding can lead to a more authentic self-perception, enabling individuals to embrace their unique strengths and perspectives. It can also pave the way for personalized strategies to optimize their abilities and overcome challenges. This understanding can also help individuals to better communicate their needs and expectations in relationships.
Potential Negative Impacts of an Autism Diagnosis
Unfortunately, the diagnostic journey isn’t always smooth. Initial reactions can range from confusion and frustration to feelings of isolation and anxiety. The diagnosis may impact self-esteem and confidence, especially if there’s a perceived stigma associated with autism. Some individuals may experience social isolation or difficulty in navigating social situations. These challenges underscore the importance of supportive environments and resources.
Impact on Self-Perception, Relationships, and Opportunities
An autism diagnosis can profoundly alter self-perception. Individuals may grapple with feelings of difference or inadequacy. However, a diagnosis can also lead to a stronger sense of self, allowing individuals to appreciate their unique talents and perspectives. Relationships can also be affected. Some individuals may experience misunderstandings or challenges in communication.
However, a diagnosis can also foster deeper connections with others who understand their needs and communication styles. Opportunities can be impacted. Individuals may face barriers to employment or educational pursuits due to societal biases. Conversely, a diagnosis can lead to opportunities for accommodations and support that enhance their chances for success.
Finding an autism test for adults can be a journey, but it’s important to remember that managing potential physical symptoms alongside the diagnostic process is crucial. For example, if you’re experiencing skin irritation and diarrhea, it’s a good idea to check out some helpful tips for treating these issues here. These symptoms can sometimes be linked to underlying conditions, which is why thorough assessment is key when exploring autism testing options for adults.
Importance of Support and Resources After Diagnosis, Autism test for adults
Comprehensive support and resources are critical after an autism diagnosis. This includes access to therapists, counselors, support groups, and educational programs. These resources provide a safe space for individuals to process their emotions, develop coping strategies, and connect with others who share similar experiences. These supports can greatly impact the journey of self-acceptance and enable individuals to develop strategies to overcome challenges.
Potential Benefits and Challenges of Receiving an Autism Diagnosis
Receiving an autism diagnosis can offer numerous benefits. Individuals can gain valuable insights into their strengths and challenges, leading to improved self-awareness and self-acceptance. They can also access tailored interventions and support systems, ultimately leading to increased well-being and improved quality of life. Challenges can arise from social stigma and misconceptions about autism. However, these challenges can be mitigated through increased awareness, education, and inclusive environments.
Table: Impact of Autism Diagnosis
| Impact | Positive/Negative effect | Example Scenarios |
|---|---|---|
| Self-Perception | Positive | Recognizing unique strengths, embracing differences, developing self-acceptance. |
| Self-Perception | Negative | Experiencing feelings of inadequacy, struggling with self-esteem, questioning personal worth. |
| Relationships | Positive | Connecting with others who understand their communication style, forming supportive relationships with empathy. |
| Relationships | Negative | Facing misunderstandings or challenges in communication, experiencing social isolation, difficulties in navigating social situations. |
| Opportunities | Positive | Accessing accommodations and support that enhance opportunities in education and employment, pursuing careers that align with strengths. |
| Opportunities | Negative | Facing barriers to employment or educational pursuits due to societal biases, experiencing discrimination or lack of understanding. |
Finding a Qualified Professional
Navigating the world of adult autism testing can feel overwhelming. One crucial step is finding a qualified professional who can accurately assess your needs and provide appropriate support. This process requires careful consideration and research to ensure you receive the best possible care.Finding the right professional is an important investment in your well-being. A qualified assessment can lead to a clearer understanding of your strengths and challenges, empowering you to develop personalized strategies for success.
This, in turn, can pave the way for accessing vital resources and support systems tailored to your unique needs.
Researching Professionals’ Experience and Qualifications
Thorough research is paramount. A qualified professional should possess a strong understanding of autism spectrum disorder (ASD) in adults. Look for professionals with experience working with adults on the spectrum. This includes not only experience with diagnosis but also experience in providing support and intervention strategies. Checking their credentials, such as relevant certifications and licenses, is essential to ensure they meet professional standards.
Look for evidence of continuing education to ensure they are up-to-date on the latest research and best practices in autism assessment and support.
Different Methods for Finding Qualified Professionals
Several avenues can help you locate qualified professionals. Consulting with your primary care physician is a good starting point. They can provide referrals to specialists with experience in diagnosing and supporting individuals with ASD. Online databases and directories dedicated to autism resources can offer a comprehensive list of qualified professionals. Networking with other individuals who have been through the assessment process can provide valuable insights and recommendations.
Word-of-mouth referrals from trusted sources are also highly valuable, as they often reflect positive experiences. Exploring professional organizations and associations dedicated to autism research and treatment is also an effective method.
Choosing the Right Professional for Individual Needs
Consider your specific needs and preferences when selecting a professional. Do you prefer a specific approach to therapy? Consider the professional’s therapeutic style. A professional’s approach to assessment and treatment should align with your personal preferences and goals. Take the time to discuss your expectations and concerns with potential professionals.
A good professional will listen attentively and address your questions openly and honestly. Understanding their approach to assessment and their experience working with individuals with similar needs is vital.
Example Table: Potential Professionals
| Qualification | Experience | Contact Information |
|---|---|---|
| Licensed Psychologist with a specialization in ASD | 10+ years experience assessing and supporting adults with ASD; experience in developing individualized treatment plans. | Dr. Emily Carter, Ph.D. | (123) 456-7890 | [email protected] |
| Certified Autism Specialist (CAS) with a background in social work | 5+ years experience providing support to adults with ASD; proficient in evidence-based interventions. | Sarah Chen, CAS | (987) 654-3210 | [email protected] |
| Occupational Therapist specializing in sensory processing disorders | 7+ years experience working with adults with ASD and sensory processing challenges; skilled in developing sensory-based interventions. | Maria Rodriguez, OTR/L | (555) 123-4567 | [email protected] |
Last Recap: Autism Test For Adults
In conclusion, navigating the world of autism testing for adults requires careful consideration, thorough research, and a compassionate approach. This guide provides a roadmap for understanding the process, from choosing a qualified professional to interpreting results and accessing vital support. Remember, accurate diagnosis is the first step towards a more fulfilling and supportive life for individuals on the autism spectrum.