Is it possible to remove ovarian cyst without surgery – Is it possible to remove ovarian cysts without surgery? This exploration delves into the various treatment options for ovarian cysts, ranging from non-surgical methods to minimally invasive surgical procedures. We’ll examine the factors influencing the decision to remove a cyst, including patient history, imaging results, and potential complications. Understanding the nuances of each approach is crucial for making informed choices about your health.
Ovarian cysts are fluid-filled sacs that can develop on the ovaries. They can vary in size and cause a range of symptoms, from mild discomfort to severe pain. While surgery is sometimes necessary, this article will cover alternative methods and factors to consider before opting for surgical intervention. The potential risks and benefits of both surgical and non-surgical treatments will be detailed, empowering readers with knowledge to make well-informed decisions about their care.
Introduction to Ovarian Cysts
Ovarian cysts are fluid-filled sacs that develop on or within the ovaries. These sacs can vary significantly in size and can often resolve on their own without any intervention. However, in some cases, cysts can cause discomfort or other complications that may necessitate medical attention, potentially including surgery. Understanding the different types, potential causes, and symptoms of ovarian cysts is crucial for appropriate management.Ovarian cysts are a common occurrence, especially during reproductive years.
Their presence can sometimes be asymptomatic, but other times they can lead to noticeable symptoms. The decision regarding treatment, including surgical intervention, is determined by factors such as cyst size, symptoms experienced, and the potential risk of complications.
Types of Ovarian Cysts
Ovarian cysts are broadly categorized into functional and non-functional cysts. Functional cysts, often benign and temporary, are commonly associated with the menstrual cycle. Non-functional cysts, conversely, can have a more complex origin and potential for long-term implications. Further understanding the characteristics of these two categories is essential for determining the best course of action.
Symptoms of Ovarian Cysts
Common symptoms of ovarian cysts include pelvic pain, bloating, and irregular menstrual cycles. The severity of these symptoms can vary greatly depending on the cyst’s size and location. Some individuals may experience no symptoms at all. Other, more severe symptoms may indicate the need for immediate medical attention.
Potential Causes of Ovarian Cysts, Is it possible to remove ovarian cyst without surgery
Several factors can contribute to the development of ovarian cysts. Hormonal imbalances, such as those associated with polycystic ovary syndrome (PCOS), are a frequent cause. Furthermore, certain medications and underlying medical conditions can also play a role. Recognizing the potential causes can help in preventive measures and early detection.
Factors Determining the Need for Surgical Intervention
The decision to perform surgery for an ovarian cyst depends on various factors. These factors include the size and type of cyst, the presence of symptoms, and the risk of complications. A doctor will thoroughly evaluate these factors to determine the most appropriate treatment plan. In some instances, watchful waiting might be an option, but in other situations, surgical intervention is necessary to alleviate symptoms or address potential risks.
Treatment Options for Ovarian Cysts
The treatment approach for ovarian cysts varies depending on the specific characteristics of the cyst. Options may range from watchful waiting to surgical intervention. The optimal treatment choice is tailored to the individual patient’s circumstances.
| Cyst Type | Symptoms | Potential Causes | Treatment Options |
|---|---|---|---|
| Functional cysts (e.g., follicular, corpus luteum) | Mild pelvic pain, bloating, irregular periods | Hormonal fluctuations related to the menstrual cycle | Watchful waiting, often resolves spontaneously; surgery if severe symptoms or complications |
| Dermoid cysts | Pelvic pain, pressure, irregular periods; potentially rapid growth | Germ cell tumors | Surgery often recommended |
| Endometriomas | Chronic pelvic pain, heavy bleeding | Endometriosis | Surgery often necessary |
| Cystadenomas | Abdominal bloating, pelvic pain, possible pressure on nearby organs | Various factors including genetic predisposition, hormonal imbalances | Surgery if symptoms are significant or the cyst shows signs of malignancy; Watchful waiting if asymptomatic |
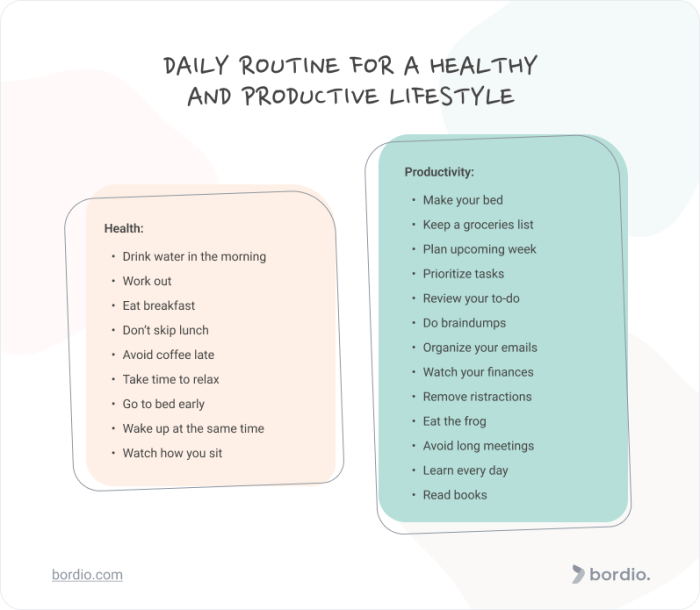
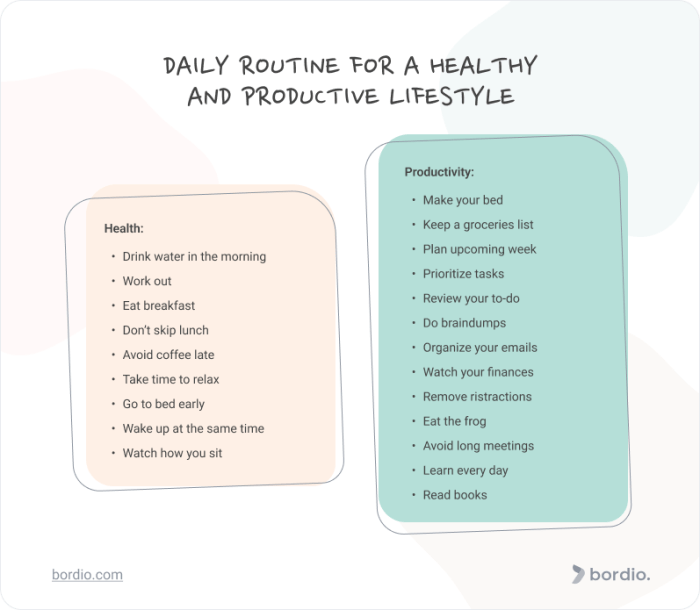
Non-Surgical Treatments for Ovarian Cysts

Many women experience ovarian cysts, which often resolve on their own without intervention. However, when symptoms persist or the cyst is causing discomfort, non-surgical management options can be explored. These methods focus on symptom relief and managing the underlying cause, rather than removing the cyst directly. Careful monitoring and consideration of individual circumstances are crucial when deciding on the best course of action.Non-surgical treatments for ovarian cysts are generally employed when the cyst is benign, asymptomatic, or causing only mild discomfort.
Wondering if ovarian cysts can be removed without surgery? While some smaller cysts might resolve on their own, often, surgical intervention is necessary. However, managing underlying conditions like diabetes and chronic kidney disease diabetes and chronic kidney disease can impact the best approach to cyst removal. Ultimately, the decision on how to handle an ovarian cyst always needs to be discussed with a healthcare professional.
These treatments aim to reduce the size of the cyst, alleviate symptoms, and allow the body to resolve the issue naturally. The effectiveness of these methods can vary depending on the size, type, and specific characteristics of the cyst, as well as the individual’s overall health and response to treatment.
Different Non-Surgical Management Approaches
Various methods can be used to manage ovarian cysts without surgery. These methods often target different aspects of the condition, such as reducing inflammation, regulating hormones, or promoting natural cyst resolution.
Potential Non-Surgical Treatments
Non-surgical treatment options for ovarian cysts include:
- Watchful Waiting: This involves regular monitoring of the cyst’s size and symptoms. This approach is suitable for small, asymptomatic cysts that are not causing significant discomfort. Doctors will typically recommend ultrasound scans at regular intervals to track the cyst’s development. In many cases, cysts resolve spontaneously without any intervention.
- Hormonal Contraceptives: Oral contraceptives, birth control pills, or other hormonal therapies can sometimes help regulate hormonal imbalances that might contribute to cyst formation. This can reduce the size of the cyst and alleviate symptoms. However, their effectiveness varies significantly from patient to patient.
- Pain Management: Over-the-counter pain relievers, like ibuprofen or naproxen, can help alleviate pain and discomfort associated with ovarian cysts. Prescription medications might be considered for severe pain.
- Dietary Adjustments: A balanced diet rich in fruits, vegetables, and whole grains, coupled with a reduction in processed foods and sugar intake, might contribute to overall hormonal balance. While not a direct treatment for cysts, a healthy diet supports overall well-being, which can be a contributing factor in cyst resolution.
- Lifestyle Modifications: Regular exercise, stress reduction techniques, and adequate sleep can play a crucial role in regulating hormone levels and promoting overall health. These modifications may contribute to the natural resolution of small, asymptomatic cysts.
Conditions for Non-Surgical Treatment
Non-surgical treatments are generally considered appropriate when the following conditions are met:
- The cyst is benign and asymptomatic or causes only mild discomfort.
- The cyst is relatively small in size and shows no signs of rapid growth.
- The patient’s overall health status is good, and there are no other underlying medical conditions that would make surgery necessary.
- The patient is willing to undergo regular monitoring and follow-up appointments.
Effectiveness Comparison and Considerations
It’s important to remember that the effectiveness of non-surgical treatments varies greatly. Some patients may experience significant relief, while others may not see much improvement. Factors like the size and type of cyst, the individual’s hormonal balance, and their response to treatment play a significant role. The approach should be tailored to the individual’s specific needs and circumstances.
Treatment Summary Table
| Treatment Type | Expected Outcome | Potential Side Effects | Duration of Treatment |
|---|---|---|---|
| Watchful Waiting | Cyst resolution without intervention | Potential for cyst growth, pain, or discomfort | Variable, depends on cyst behavior |
| Hormonal Contraceptives | Reduced cyst size, symptom relief | Mood changes, headaches, nausea, breast tenderness | Months to years |
| Pain Management | Temporary pain relief | Potential for stomach upset, allergic reactions | Variable, as needed |
| Dietary Adjustments | Improved hormonal balance | None, or minor digestive adjustments | Months to years |
| Lifestyle Modifications | Improved overall health | None, or minor discomfort initially | Months to years |
Surgical Alternatives to Ovarian Cyst Removal
Choosing the right approach for ovarian cyst removal is crucial, as the best course of action depends on various factors, including the size, type, and location of the cyst. While non-surgical methods are often explored first, surgery remains a vital option for managing certain ovarian cysts. This section delves into the realm of minimally invasive surgical procedures, highlighting the advantages and disadvantages of each technique.Minimally invasive surgical procedures, often performed laparoscopically or robotically, are now common choices for ovarian cyst removal.
These techniques involve smaller incisions, resulting in less pain, scarring, and a faster recovery period compared to traditional open surgery. This approach also helps to minimize blood loss and reduce the risk of complications.
Minimally Invasive Surgical Procedures
Minimally invasive surgical procedures for ovarian cyst removal offer a less invasive alternative to traditional open surgery. These procedures utilize small incisions, specialized instruments, and often, a camera (laparoscope) to visualize the surgical site. This approach allows for precise cyst removal with minimal disruption to surrounding tissues. The most common minimally invasive methods include laparoscopic surgery and robotic surgery.
Laparoscopic Surgery
Laparoscopic surgery for ovarian cyst removal involves inserting a small camera and surgical instruments through several small incisions in the abdomen. The surgeon uses the camera’s view to guide the instruments and remove the cyst. This technique is often preferred due to its less invasive nature and faster recovery time.Advantages of laparoscopic surgery include: reduced pain and scarring, quicker recovery, and less blood loss.
Disadvantages include the potential for complications related to the use of small incisions and the need for specialized surgical equipment and expertise. The recovery process following laparoscopic surgery typically involves several days of rest and gradual return to normal activities. Pain management strategies, such as prescribed medications, are crucial during the initial recovery period.
Robotic Surgery
Robotic surgery, another minimally invasive option, utilizes robotic arms controlled by the surgeon. The surgeon operates the robotic arms from a console, providing a magnified, three-dimensional view of the surgical site. This technique often offers greater precision and dexterity compared to laparoscopic surgery.Advantages of robotic surgery include enhanced visualization, improved precision, and potentially reduced invasiveness. Disadvantages include the higher cost of robotic equipment and the need for specialized training for surgeons.
The recovery process is generally similar to laparoscopic surgery, with a focus on gradual return to normal activities and pain management.
Surgical Techniques for Removing Ovarian Cysts
Surgical techniques for ovarian cyst removal vary based on the type and location of the cyst. Some cysts can be removed through a simple excision, while others may require more complex procedures, such as partial or complete removal of the ovary.
Recovery Process After Each Surgical Procedure
The recovery process after minimally invasive surgery for ovarian cyst removal typically involves a few days of rest and gradual return to normal activities. Patients are usually discharged within 24-48 hours and can expect mild to moderate pain. Adherence to post-operative instructions is crucial for a smooth recovery. It’s essential to follow a balanced diet and maintain adequate hydration.
Comparison of Minimally Invasive Surgical Procedures
| Procedure Name | Recovery Time (Approximate) | Potential Risks | Cost Comparison |
|---|---|---|---|
| Laparoscopic Surgery | 1-2 weeks | Infection, bleeding, injury to surrounding organs, or recurrence | Moderate |
| Robotic Surgery | 1-2 weeks | Infection, bleeding, injury to surrounding organs, or recurrence, and potential damage to nearby structures | High |
Note: Recovery times and costs can vary depending on individual factors and specific circumstances. Consult with your healthcare provider for personalized guidance.
Factors Influencing the Decision to Remove an Ovarian Cyst: Is It Possible To Remove Ovarian Cyst Without Surgery
Deciding whether to remove an ovarian cyst involves careful consideration of various factors. A thorough evaluation, incorporating patient history, physical examination, and imaging results, is crucial to determine the appropriate course of action. The goal is to balance the potential risks and benefits of surgery with the patient’s overall health and well-being.The decision to surgically remove an ovarian cyst is not always straightforward.
Several factors contribute to the complexity of this medical judgment. Understanding these factors is vital for both patients and healthcare providers to make informed choices. Ultimately, the best course of action depends on the individual circumstances of each patient.
Patient History and Physical Examination
Patient history plays a significant role in evaluating the need for ovarian cyst removal. A detailed medical history, including past surgeries, family history of ovarian cancer, and any associated symptoms (such as pain, bloating, or irregular periods), provides valuable context. Physical examination, including a pelvic exam, helps assess the size, location, and characteristics of the cyst. This information, combined with the patient’s overall health, helps determine the potential risks and benefits of different treatment options.
While some ovarian cysts might resolve on their own, it’s often not a simple answer to whether they can be removed without surgery. Recent research into weight loss medications, like the potential for wegovy hair loss risk , highlights the complexities of unintended side effects. Ultimately, the best approach for managing ovarian cysts always involves a consultation with a healthcare professional.
Role of Imaging Techniques
Imaging techniques like ultrasound, CT scan, and MRI are essential tools in assessing ovarian cysts. Ultrasound is often the first-line imaging modality due to its accessibility and safety. It helps determine the size, location, and characteristics of the cyst, including whether it is solid or cystic. CT scans provide detailed images of the cyst and surrounding structures, aiding in evaluating its relationship with other organs.
MRI scans offer the most detailed visualization of soft tissues and can help differentiate between benign and malignant lesions. The results of these imaging studies help determine the cyst’s nature and guide the decision-making process.
Factors Considered in Determining the Appropriate Treatment Approach
Several factors influence the choice of treatment for an ovarian cyst. These factors include the cyst’s size, location, and characteristics (as determined by imaging), the patient’s age and overall health, the presence of symptoms, and the potential risks and benefits of each treatment option. The likelihood of the cyst being benign or malignant also plays a crucial role in the decision.
Ultimately, the goal is to select the treatment that minimizes risks while maximizing the chance of a positive outcome.
Table of Factors Influencing Ovarian Cyst Removal Decision
| Patient Factors | Imaging Results | Potential Complications | Treatment Recommendation |
|---|---|---|---|
| History of ovarian cysts, family history of ovarian cancer, severe pain | Large, complex cyst with solid components, suspicious appearance on ultrasound | Infection, bleeding, damage to surrounding organs | Surgical removal |
| Young age, asymptomatic, small cyst with clear imaging | Simple cyst, less than 5cm in diameter, no worrisome features | Minimal, mostly related to potential recurrence | Observation, follow-up imaging |
| Patient with multiple comorbidities, high surgical risk | Small cyst, well-defined margins, benign appearance on MRI | Anesthesia complications, blood clots, infection | Observation, regular monitoring |
| Patient with severe pain, significant impact on daily life | Rapidly growing cyst, significant distortion of surrounding organs | Pain relief, prevention of further complications | Surgical removal |
Post-Surgical Considerations
Navigating the post-operative period after ovarian cyst removal surgery requires careful attention to recovery and potential complications. This phase is crucial for ensuring a smooth return to health and well-being. Understanding the typical post-operative care, potential complications, and importance of follow-up appointments is vital for successful recovery.
Wondering if ovarian cysts can be removed without surgery? It really depends on the size and type of cyst, and a qualified healthcare provider, like a gynecologist or general practitioner, is crucial in determining the best course of action. What is a provider and how they assess your situation will greatly influence whether or not surgery is necessary.
Ultimately, a thorough examination and personalized treatment plan are key to managing any potential health concerns.
Typical Post-Operative Care
Post-operative care focuses on managing pain, promoting healing, and preventing complications. Patients are typically monitored closely for the first few hours after surgery. This includes vital sign monitoring, pain management, and assessment of the surgical site. Depending on the extent of the surgery and the patient’s overall health, discharge instructions may include medication regimens, dietary restrictions, and activity limitations.
Strict adherence to these instructions is essential for a successful recovery.
Common Post-Surgical Complications
While ovarian cyst removal surgery is generally safe, some complications can occur. These may include infection at the surgical site, bleeding, blood clots, and adverse reactions to medications. Less common but still possible complications may involve damage to surrounding organs or nerves. Prompt medical attention is crucial if any of these complications arise.
Importance of Follow-Up Appointments
Regular follow-up appointments are essential for monitoring healing and detecting any potential long-term issues. These appointments allow the healthcare provider to assess the surgical site, evaluate overall health, and address any concerns the patient may have. Follow-up appointments are also crucial for addressing any persistent symptoms or complications that may arise.
Potential Long-Term Effects of Surgery
The long-term effects of ovarian cyst removal surgery are generally minimal. In some cases, patients might experience slight changes in their menstrual cycle or experience mild discomfort in the pelvic area. However, in rare instances, some women might experience more significant issues, such as infertility or hormonal imbalances. The long-term outcomes vary based on individual circumstances and the extent of the surgical procedure.
Post-Surgical Care Summary
| Post-Surgical Aspect | Potential Complications | Monitoring Schedule | Recovery Timeline |
|---|---|---|---|
| Pain Management | Post-operative pain, persistent discomfort | Regular pain assessment, medication adjustments | Generally, pain subsides within a few days to a week, but individual experiences vary. |
| Surgical Site Healing | Infection, excessive bleeding, hematoma formation | Regular wound checks, temperature monitoring | Healing time varies, but most patients recover within 4-6 weeks, with full recovery taking several months. |
| Medications | Adverse reactions to medications, drug interactions | Monitoring of medication effectiveness and side effects | Medication regimen may be adjusted based on the patient’s response and recovery progress. |
| Activity Restrictions | Increased pain, delayed healing, complications from strenuous activities | Gradual increase in activity level, avoiding strenuous activities | Activity levels gradually increase as the patient’s condition improves. |
Risk Factors and Complications
Ovarian cysts, while often benign, can pose potential risks and complications. Understanding these factors is crucial for proactive management and informed decision-making. Proper awareness of the risks and complications associated with both surgical and non-surgical approaches can help patients and healthcare providers make the best choices.
Potential Risk Factors
Several factors can increase the likelihood of developing ovarian cysts. Age, hormonal imbalances, and certain medical conditions play a significant role. Genetics can also influence the risk. For example, women with a family history of ovarian cysts or related conditions might be predisposed to developing them. Lifestyle factors, such as diet and exercise, can also indirectly impact the risk.
Furthermore, certain medications or medical treatments might increase the likelihood of developing ovarian cysts.
Types of Ovarian Cysts and Their Risks
Different types of ovarian cysts carry varying degrees of risk. Functional cysts, which often resolve spontaneously, generally pose less risk than other types. However, even functional cysts can cause discomfort or pain, and in some cases, they may require intervention. Dermoid cysts, on the other hand, have a higher potential for complications due to their composition and possible growth.
They may necessitate surgical removal due to the potential for torsion or rupture. Cysts associated with endometriosis can also cause significant discomfort and potential adhesions, increasing the complexity of surgical procedures.
Complications Associated with Ovarian Cysts
Ovarian cysts can lead to a range of complications, both surgical and non-surgical. Non-surgical complications include pain, bloating, and irregular periods. In severe cases, ovarian cysts can rupture, leading to internal bleeding and severe abdominal pain. Surgical complications from cyst removal procedures, while rare, can include infection, bleeding, and damage to surrounding organs.
Minimizing Risks and Complications
Preventive measures can help reduce the risk of complications. Maintaining a healthy weight, managing stress, and adopting a balanced diet rich in fruits and vegetables can contribute to overall well-being and potentially lower the risk of developing ovarian cysts. Regular checkups with a healthcare provider are essential for early detection and management of potential problems. Furthermore, understanding one’s family history of reproductive health conditions can provide valuable insights into personal risk factors.
Comparison of Risk Factors and Complications for Different Cyst Types
| Risk Factors | Potential Complications | Prevention Strategies | Management Strategies |
|---|---|---|---|
| Age, hormonal fluctuations, family history, lifestyle factors | Pain, bloating, irregular periods, rupture, internal bleeding, potential torsion, adhesions | Healthy lifestyle, regular checkups, stress management | Close monitoring, pain management, surgical intervention (if necessary) |
| Rapid growth, composition (e.g., dermoid cyst), endometriosis | Severe pain, torsion (twisting of the ovary), potential for rupture, complications during surgery | Early detection, regular monitoring, appropriate screening | Surgical removal, pain management, follow-up care |
| Associated medical conditions (e.g., PCOS), certain medications | Increased risk of cyst recurrence, potential for complications from associated conditions | Management of underlying conditions, appropriate medication choices | Collaborative care with specialists, targeted treatment |
Case Studies

Understanding the nuances of ovarian cyst management often hinges on real-world examples. These case studies offer a glimpse into the decision-making process, highlighting the factors influencing the choice between non-surgical and surgical interventions. They illustrate the importance of considering individual patient characteristics, cyst type, size, and symptoms when developing a personalized treatment strategy.
Illustrative Cases of Ovarian Cyst Management
These case studies depict different scenarios, each emphasizing the complexity of ovarian cyst treatment. Careful consideration of individual factors like age, overall health, and potential complications is crucial for determining the optimal course of action.
Case Study 1: Functional Cyst in a Young Woman
A 25-year-old woman presented with mild pelvic pain and a small, simple functional cyst. The cyst was monitored with ultrasound scans every few months. The cyst’s size remained stable and symptoms subsided without intervention. This case demonstrates how some functional cysts resolve spontaneously, making close monitoring a viable option.
Case Study 2: Complex Cyst in a Perimenopausal Woman
A 48-year-old woman with a history of irregular periods experienced persistent lower abdominal pain and a complex cyst. The cyst showed signs of possible malignancy on imaging. The decision was made to surgically remove the cyst. The subsequent pathology report confirmed the cyst to be benign, but the surgical approach was deemed necessary given the high risk of malignancy in complex cysts.
Case Study 3: Large Endometrioma in a Woman with Severe Pain
A 35-year-old woman with endometriosis experienced severe pelvic pain and a large endometrioma. Non-surgical treatments, such as pain management and hormonal therapy, were initially attempted. However, these proved insufficient to alleviate her pain. Surgical removal of the endometrioma was performed, resulting in significant pain reduction and improved quality of life.
Case Study 4: Small Dermoid Cyst in a Teenager
A 16-year-old girl presented with a small dermoid cyst discovered during a routine pelvic examination. The cyst was non-tender and did not cause significant symptoms. Given its size and benign nature, a wait-and-see approach was adopted, with follow-up scans to monitor its growth. This example highlights the importance of the size and benign nature of the cyst in choosing the treatment approach.
Comparative Analysis of Treatment Outcomes
The outcomes of these case studies varied based on several factors, including the cyst’s type, size, location, and the patient’s overall health. In cases of functional cysts, close monitoring often led to spontaneous resolution. Complex cysts, particularly those exhibiting suspicious characteristics, necessitated surgical intervention for definitive diagnosis and treatment. Pain management and hormonal therapy proved effective for certain types of cysts, but surgical removal was ultimately required for others.
Table of Case Studies
| Case ID | Cyst Characteristics | Treatment Plan | Outcome |
|---|---|---|---|
| 1 | Small, simple functional cyst | Ultrasound monitoring | Cyst resolved spontaneously |
| 2 | Complex cyst, suspicious imaging | Surgical removal | Benign cyst, successful removal |
| 3 | Large endometrioma, severe pain | Initial non-surgical, then surgical removal | Significant pain reduction, improved quality of life |
| 4 | Small dermoid cyst, asymptomatic | Observation, follow-up scans | No intervention required |
Illustrations for Ovarian Cyst Anatomy and Procedures
Understanding ovarian cysts requires visualizing their location and structure within the female reproductive system. Visual aids are crucial for comprehending the complexities of both normal ovarian function and the various types of cysts that can develop. Illustrations can effectively demonstrate the potential impact of cysts on surrounding organs and guide clinicians in selecting the most appropriate treatment strategy.
Ovarian Anatomy and a Typical Cyst
The ovary, shaped like an almond, is located on either side of the uterus. Crucially, it houses the follicles, where eggs mature. A typical ovarian cyst forms when a follicle develops abnormally, either failing to release an egg or becoming filled with fluid. The illustration would depict a healthy ovary alongside an ovary containing a simple functional cyst.
The cyst would be shown as a fluid-filled sac of varying sizes, clearly distinct from the surrounding ovarian tissue. Illustrating the position of the ovary relative to other pelvic organs, such as the fallopian tubes and uterus, provides context for potential pressure or adhesion issues. This visual representation helps understand the impact of a cyst’s presence.
Surgical Procedures for Ovarian Cyst Removal
Visualizing surgical procedures aids in understanding the different approaches to removing ovarian cysts. Illustrations depicting laparoscopic ovarian cystectomy, a minimally invasive technique, should show the surgeon’s instruments entering the abdomen through small incisions. The illustration should also depict the use of specialized instruments for cyst dissection and removal. A comparison with open surgery, involving a larger incision, could also be presented, highlighting the differences in approach and recovery time.
Cyst Types and Impact on Surrounding Structures
Different types of ovarian cysts have varying characteristics and potential impacts on surrounding tissues. Illustrations should differentiate between functional cysts, like follicular cysts, and more complex types such as endometriomas. Illustrating the potential for an endometrioma to cause adhesions between the ovary and surrounding organs, such as the fallopian tubes or bowel, will emphasize the importance of precise surgical intervention.
Visual representations of these adhesions would aid in understanding the possible complications during cyst removal.
Steps Involved in Surgical Procedures
The detailed steps of each surgical procedure are essential for understanding the process. A series of illustrations would depict the surgical steps, from initial incision to cyst removal and closure. For example, the laparoscopic procedure might show a step-by-step process:
- Visualization of the cyst using a camera inserted through a small incision.
- Use of specialized instruments to isolate and dissect the cyst from surrounding tissues.
- Removal of the cyst and examination of its contents.
- Closure of the incisions.
This visual sequence clarifies the precision and care involved in each surgical step.
Minimally Invasive Procedure Stages
A sequence of illustrations showcasing the stages of a minimally invasive procedure, such as laparoscopic cystectomy, would be highly informative. The illustrations should depict:
- The initial setup, showing the small incisions and the placement of surgical instruments.
- The use of specialized instruments for cyst dissection and removal, emphasizing the precision of the procedure.
- The retrieval of the cyst and the confirmation of its complete removal.
- The final steps of wound closure.
This visual representation provides a clear understanding of the procedure’s complexity and the surgeon’s ability to perform the operation with minimal disruption to surrounding tissues.
Conclusion
In conclusion, the decision regarding ovarian cyst removal is multifaceted and depends on several factors. This article has explored the spectrum of options, from non-surgical treatments to minimally invasive surgery. Ultimately, the choice of treatment should be made in consultation with a healthcare professional. By understanding the various approaches, patients can actively participate in their care plan and work towards optimal health outcomes.