Treatments for HER2 positive breast cancer are a multifaceted approach, encompassing targeted therapies, chemotherapy, endocrine therapies, immunotherapy, and combination strategies. This guide dives deep into each of these treatment modalities, exploring their mechanisms of action, potential side effects, and efficacy in the context of HER2-positive breast cancer. Understanding these approaches is crucial for patients and their caregivers to make informed decisions regarding their treatment plan.
The journey through breast cancer can be challenging, but this comprehensive overview aims to provide clarity and empower those facing this diagnosis.
This in-depth look at treatment options for HER2-positive breast cancer covers the spectrum of available strategies, from established therapies to innovative approaches currently under research. It details the role of HER2 testing in diagnosis, highlighting the importance of personalized treatment plans. We’ll also touch on patient support and resources available to those navigating this complex medical journey.
Overview of HER2-Positive Breast Cancer
HER2-positive breast cancer is a subtype of breast cancer characterized by the overexpression or amplification of the HER2 protein on the cancer cells’ surface. This protein plays a crucial role in cell growth and division, and its abnormal presence in high amounts can lead to rapid cancer development and progression. Understanding this subtype is essential for effective diagnosis and treatment planning.The HER2 protein acts like a “growth accelerator” for cells.
Normally, the HER2 protein helps cells grow and divide in a controlled manner. However, in HER2-positive breast cancer, there are too many HER2 protein receptors on the surface of the cancer cells. This leads to uncontrolled cell growth, division, and the formation of tumors. This excessive stimulation of cell growth is a key factor in the aggressive nature of this subtype.
HER2 Protein and Cancer Development, Treatments for her2 positive breast cancer
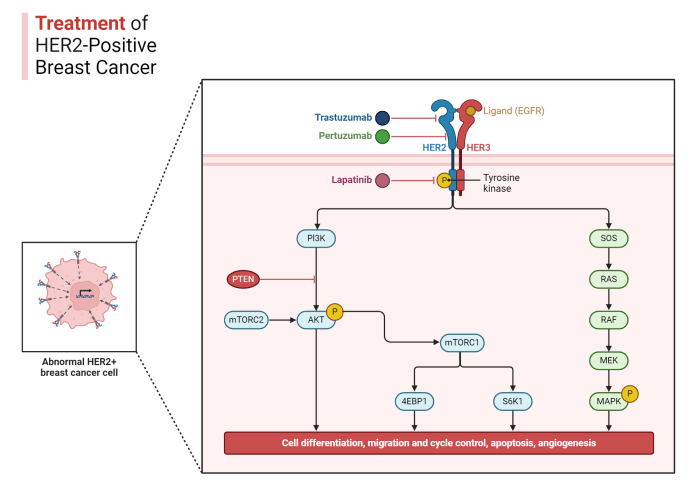
The HER2 protein is part of a family of growth-signaling proteins called receptor tyrosine kinases. These proteins typically play a role in regulating cell growth and division. In HER2-positive breast cancer, the HER2 protein is either overproduced or duplicated (amplified) on the cell surface. This leads to excessive signaling that triggers rapid cell division, ultimately contributing to tumor growth.
The exact mechanisms are still under investigation, but the result is clear: unchecked cell proliferation.
Prevalence of HER2-Positive Breast Cancer
HER2-positive breast cancer accounts for approximately 15-20% of all breast cancers diagnosed. This means that it’s a significant subtype to consider. Its prevalence varies slightly across different populations and geographic regions, but the overall percentage remains relatively consistent. Early detection and appropriate treatment strategies are critical for managing this subtype effectively.
HER2 Testing in Diagnosis
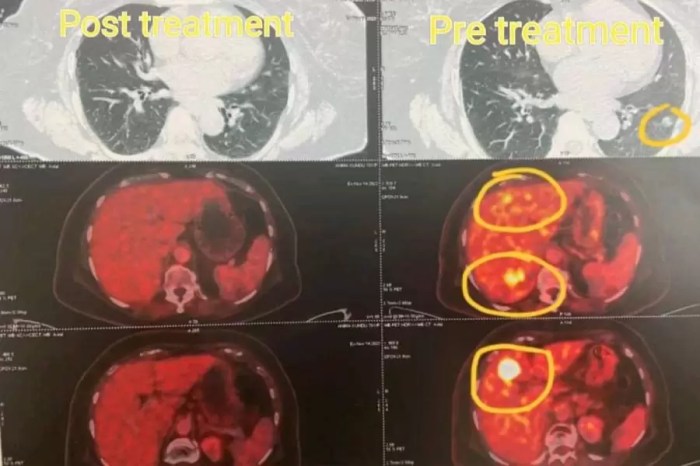
HER2 testing is a crucial diagnostic tool in identifying HER2-positive breast cancer. It’s performed on breast tissue samples obtained during a biopsy. The test can detect the overexpression or amplification of the HER2 protein. This information is vital in determining the most effective treatment strategies. It helps tailor therapy to the specific characteristics of the cancer, ensuring that patients receive targeted interventions.
Common Symptoms of HER2-Positive Breast Cancer
Symptoms of HER2-positive breast cancer are similar to those of other breast cancers. They can include a lump or thickening in the breast, skin changes such as dimpling or redness, nipple discharge, or pain. It’s crucial to remember that these symptoms can also be caused by other conditions. Therefore, it’s essential to consult a healthcare professional for a proper diagnosis.
Regular breast self-exams and mammograms are vital for early detection.
HER2-Positive Breast Cancer Stages and Treatment Approaches
| Stage | Common Symptoms | Typical Treatment Approaches ||—|—|—|| Stage I | Often asymptomatic or with a small, non-palpable tumor. May include mild breast pain or tenderness. | Surgery (lumpectomy or mastectomy) often combined with radiation therapy. Targeted therapies such as Herceptin may be considered. || Stage II | A palpable tumor, possibly with some skin changes or nipple discharge.
| Surgery (lumpectomy or mastectomy) often combined with radiation therapy and chemotherapy. Targeted therapies such as Herceptin are often included. || Stage III | More advanced tumor size, possible lymph node involvement, and/or spread to other areas. Symptoms may include more noticeable pain, swelling, or skin irritation. | Combination of chemotherapy, surgery, radiation therapy, and targeted therapies like Herceptin.
The specific treatment plan depends on the extent of the disease. || Stage IV | Metastatic disease, with the cancer having spread to other parts of the body. Symptoms vary widely depending on the location of the metastases. Common examples include bone pain, lung problems, or brain involvement. | Chemotherapy, targeted therapies (like Herceptin), hormone therapy, and palliative care to manage symptoms and improve quality of life.
|
Targeted Therapies
Targeted therapies are a crucial aspect of treating HER2-positive breast cancer. These therapies specifically target the HER2 protein, which is overexpressed in these cancers, hindering its uncontrolled growth and spread. They represent a significant advancement in cancer treatment, often offering more precise and effective approaches compared to traditional chemotherapy.
Mechanism of Action
Targeted therapies for HER2-positive breast cancer work by interfering with the HER2 protein’s function. This protein plays a key role in cell growth and division. When HER2 is overexpressed, cells grow and divide uncontrollably, leading to tumor formation. Targeted therapies block the HER2 protein’s ability to signal cell growth, thus inhibiting tumor development and spread. This disruption can be achieved through various mechanisms, such as blocking the HER2 protein itself, or preventing its interaction with other proteins involved in the signaling cascade.
Available Targeted Therapies
A range of targeted therapies are available for HER2-positive breast cancer, each with its own specific mechanism of action. These drugs often work in combination with other treatments, further enhancing their efficacy.
- Trastuzumab (Herceptin): This monoclonal antibody directly binds to the HER2 protein, preventing it from activating signaling pathways that promote cell growth. It is one of the most common and established targeted therapies.
- Pertuzumab (Perjeta): This monoclonal antibody targets a different site on the HER2 protein than trastuzumab, further inhibiting its function and blocking the formation of signaling complexes. Pertuzumab is often used in combination with trastuzumab.
- Lapatinib (Tykerb): This tyrosine kinase inhibitor inhibits the activity of HER2 and another related protein, EGFR, thus preventing signaling pathways that contribute to uncontrolled cell growth. It’s sometimes used in combination with trastuzumab, particularly in cases of resistance or relapse.
- Neratinib (Nerlynx): This drug inhibits HER2 activity by blocking the tyrosine kinase domain, thereby interfering with signaling and growth. It’s frequently used in later-stage or metastatic disease.
- Adcetris (brentuximab vedotin): This antibody-drug conjugate targets CD30, a protein expressed on certain immune cells and some types of lymphoma cells. Although not directly targeting HER2, it may be used in combination with other therapies, especially when HER2-positive breast cancer has spread to other parts of the body.
Potential Side Effects
Targeted therapies, while effective, can have various side effects, which often vary depending on the specific drug and the individual patient. These side effects can range from mild to severe and can include:
- Cardiotoxicity: Damage to the heart muscle is a potential side effect, particularly with trastuzumab and other HER2-targeted therapies. Regular cardiac monitoring is crucial to detect and manage any cardiac issues.
- Fatigue: Many patients experience fatigue as a side effect, which can vary in severity and impact daily life.
- Skin rash or irritation: Some patients experience skin rashes or other skin reactions as a side effect.
- Nausea and vomiting: These gastrointestinal side effects are also possible.
- Diarrhea: Diarrhea can occur as a side effect in some patients.
- Liver problems: Some patients may experience liver problems as a side effect.
Comparison of Targeted Therapies
Different targeted therapies for HER2-positive breast cancer exhibit varying efficacy and safety profiles. Factors like the stage of the disease, the patient’s overall health, and potential drug interactions influence the choice of therapy.
| Drug Name | Mechanism of Action | Common Side Effects | Typical Dosage |
|---|---|---|---|
| Trastuzumab | Binds to HER2 protein, inhibiting its function | Cardiotoxicity, fatigue, nausea, skin rash | Typically administered intravenously every 3 weeks |
| Pertuzumab | Targets a different site on HER2, further inhibiting its function | Fatigue, diarrhea, skin rash, joint pain | Typically administered intravenously every 3 weeks |
| Lapatinib | Inhibits HER2 and EGFR tyrosine kinase activity | Diarrhea, rash, skin irritation, liver problems | Typically administered orally twice daily |
Chemotherapy Regimens
Chemotherapy plays a crucial role in the treatment of HER2-positive breast cancer, often used in combination with targeted therapies like Herceptin. It aims to shrink or destroy cancer cells, particularly when the cancer has spread beyond the initial site. Understanding the different chemotherapy regimens and their potential side effects is essential for informed decision-making during treatment.
Common Chemotherapy Regimens
Various chemotherapy regimens are employed in the treatment of HER2-positive breast cancer, each with specific combinations of drugs and dosages. These regimens are tailored to individual patient needs, considering factors like the stage of the cancer, overall health, and other concurrent treatments.
Role of Chemotherapy in HER2-Positive Breast Cancer
Chemotherapy, when used in conjunction with other treatments, often aims to reduce the tumor burden before surgery or radiation therapy, making the subsequent treatments more effective. It can also be administered after surgery to kill any remaining cancer cells and prevent recurrence. In advanced cases, chemotherapy may be the primary treatment to shrink tumors and alleviate symptoms.
Potential Side Effects of Chemotherapy Regimens
Chemotherapy drugs work by targeting rapidly dividing cells, which unfortunately also includes healthy cells in the body. This can lead to various side effects, ranging from mild to severe. Common side effects include nausea, vomiting, fatigue, hair loss, and mouth sores. More serious side effects can involve damage to the bone marrow, leading to anemia or infections. Careful monitoring and supportive care are essential during chemotherapy treatment to manage and mitigate these side effects.
Duration and Frequency of Chemotherapy Treatments
The duration and frequency of chemotherapy treatments vary based on the specific regimen and individual patient response. Treatment cycles typically consist of several weeks of chemotherapy followed by a period of rest. The total treatment duration can range from a few months to several years, depending on the cancer’s stage and the patient’s overall health. Regular blood tests and assessments are crucial to monitor treatment effectiveness and adjust the regimen as needed.
Navigating treatments for HER2-positive breast cancer can feel overwhelming, but it’s important to remember there are various options. While some treatments focus on targeted therapies, others involve a holistic approach. For instance, exploring natural treatments for conditions like ankylosing spondylitis can offer valuable insights into holistic well-being and alternative therapies, which can sometimes be beneficial in managing various health challenges.
Ultimately, the best approach to HER2-positive breast cancer treatment often involves a combination of conventional and complementary therapies, including research into ankylosing spondylitis natural treatment , tailored to individual needs and preferences. The goal is to find what works best for you, balancing your physical and emotional needs.
Chemotherapy Regimens Table
| Regimen | Active Ingredients | Common Side Effects | Typical Treatment Duration |
|---|---|---|---|
| AC | Adriamycin (doxorubicin) and Cyclophosphamide | Nausea, vomiting, hair loss, fatigue, mouth sores, possible heart damage with Adriamycin | Typically 4-6 cycles |
| TC | Taxol (paclitaxel) and Carboplatin | Nausea, vomiting, fatigue, hair loss, peripheral neuropathy (nerve damage) | Typically 6-8 cycles |
| FEC | Fluorouracil, Epirubicin, and Cyclophosphamide | Nausea, vomiting, fatigue, hair loss, mouth sores | Typically 4-6 cycles |
| CMF | Cyclophosphamide, Methotrexate, and Fluorouracil | Nausea, vomiting, fatigue, hair loss, mouth sores | Typically 6-12 cycles |
| TCHP | Docetaxel, Carboplatin, Cisplatin, and Hydroxyurea | Nausea, vomiting, fatigue, hair loss, potential for kidney and nerve damage | Variable, depending on the specific use |
Note: This table provides a general overview. Specific regimens and durations may vary based on individual patient needs and cancer characteristics. Always consult with your oncologist for personalized treatment plans.
Endocrine Therapies
Endocrine therapies, also known as hormonal therapies, play a significant role in the treatment of HER2-positive breast cancer, particularly in cases where the cancer cells are fueled by hormones. These therapies aim to reduce the amount of hormones available to the cancer cells, thus slowing or stopping their growth. Understanding their mechanisms, potential side effects, and combination strategies is crucial for effective management of the disease.
Role of Endocrine Therapies in HER2-Positive Breast Cancer
Endocrine therapies are often used in HER2-positive breast cancer, particularly in postmenopausal women. While not a primary treatment for HER2-positive breast cancer, they can be crucial in reducing recurrence risk and managing symptoms. These therapies target hormone receptors that may be present on some HER2-positive tumors. For instance, some HER2-positive cancers may also express hormone receptors, and in these cases, endocrine therapies can be highly effective.
Mechanism of Action of Common Endocrine Therapies
Endocrine therapies work by interfering with the production, release, or action of hormones in the body. Common types include aromatase inhibitors, which block the production of estrogen in postmenopausal women, and tamoxifen, which blocks estrogen’s ability to bind to its receptors. Another class, such as fulvestrant, works by blocking estrogen receptors, thus preventing the hormone from binding to the receptors.
These therapies disrupt the hormonal pathways that fuel the growth of certain breast cancer cells.
Potential Side Effects of Endocrine Therapies
Endocrine therapies can cause a range of side effects, varying in severity and frequency. Common side effects include hot flashes, vaginal dryness, mood changes, and joint pain. Some individuals may experience more severe side effects, such as osteoporosis, and a heightened risk of blood clots. Careful monitoring and management of these side effects are essential.
Navigating treatments for HER2-positive breast cancer can feel overwhelming. Fortunately, there are many effective options available, but sometimes dealing with the side effects can be tough. It’s like battling acne, except instead of zits, it’s the body’s response to the treatment. Learning how to manage skin breakouts is key, and checking out how to get rid of pimples might offer some helpful tips that translate to managing these side effects.
Ultimately, staying informed and working closely with your doctor is crucial for successful treatment of HER2-positive breast cancer.
Use of Endocrine Therapies in Combination with Other Treatments
Combining endocrine therapies with other treatments, such as chemotherapy or targeted therapies, can enhance their effectiveness and reduce the risk of recurrence. For example, a combination of an aromatase inhibitor with chemotherapy might be used to treat a specific subtype of HER2-positive breast cancer. This approach can provide a more comprehensive strategy to target the cancer cells.
Table of Endocrine Therapies
| Therapy | Mechanism of Action | Common Side Effects | Typical Duration of Treatment |
|---|---|---|---|
| Aromatase Inhibitors (e.g., Anastrozole, Letrozole, Exemestane) | Block the production of estrogen in postmenopausal women. | Hot flashes, vaginal dryness, joint pain, mood changes, bone loss, risk of blood clots. | Typically years, often continued until recurrence risk is significantly reduced. |
| Tamoxifen | Blocks estrogen from binding to its receptors. | Hot flashes, vaginal dryness, mood changes, blood clots, uterine cancer risk. | Usually 5 years, but duration can vary depending on individual circumstances. |
| Fulvestrant | Binds to and blocks estrogen receptors, thus preventing estrogen from activating them. | Hot flashes, vaginal dryness, fatigue, nausea, weight gain, loss of bone density, blood clots, liver problems. | Typically years, continued until recurrence risk is significantly reduced. |
Immunotherapy Approaches: Treatments For Her2 Positive Breast Cancer
Harnessing the body’s own immune system to fight cancer is a promising frontier in oncology. Immunotherapy, in the context of HER2-positive breast cancer, aims to stimulate the immune response to target and destroy cancer cells, often in conjunction with other therapies. This approach holds the potential to improve outcomes, especially for patients who haven’t responded well to conventional treatments.
Immunotherapy in HER2-Positive Breast Cancer
Immunotherapy strategies for HER2-positive breast cancer are still under active research and development. These strategies are often designed to work in concert with other treatments, such as chemotherapy or targeted therapies. The idea is to enhance the body’s natural defenses against the cancer cells.
Examples of Immunotherapies
Several immunotherapies are being explored for their potential in HER2-positive breast cancer. One key example is checkpoint inhibitors, which block the proteins that normally keep the immune system from attacking cancer cells. Other avenues of investigation include cancer vaccines, designed to teach the immune system to recognize and destroy cancer cells.
Mechanism of Action
The mechanism of action varies depending on the specific immunotherapy. Checkpoint inhibitors, for example, work by releasing the brakes on the immune system, allowing T cells (a type of immune cell) to identify and destroy cancer cells. Cancer vaccines, on the other hand, aim to train the immune system to recognize unique proteins found on the surface of cancer cells, triggering an immune response.
Potential Benefits and Limitations
Immunotherapies show promise in enhancing treatment outcomes for HER2-positive breast cancer, potentially leading to longer survival and reduced recurrence. However, they are not without limitations. One potential limitation is the risk of side effects, as the immune system is being activated. Additionally, not all patients respond to immunotherapy, and predicting which patients will benefit most remains a challenge.
Table of Immunotherapy Approaches
| Immunotherapy Approach | Mechanism of Action | Potential Benefits | Limitations |
|---|---|---|---|
| Checkpoint Inhibitors | Block proteins that normally suppress the immune response, allowing T cells to attack cancer cells. | Potentially improved survival rates, reduced recurrence, and enhanced response to other treatments. | Potential for significant side effects, including immune-related adverse events, and not all patients respond. |
| Cancer Vaccines | Train the immune system to recognize and destroy cancer cells by exposing it to cancer-specific proteins. | Potential for long-lasting immunity and reduced recurrence, particularly when used in conjunction with other therapies. | Limited efficacy in some cases, need for further development, and potential for side effects. |
| Adoptive Cell Therapy | Infuse immune cells, such as T cells, that have been engineered to target cancer cells, into the patient. | Potentially potent and long-lasting anti-cancer effects, potentially effective for those who haven’t responded to other therapies. | Requires careful selection of patients, complex procedures, potential for severe side effects, and high cost. |
Combination Therapies
Combining different treatment approaches is a common strategy in battling HER2-positive breast cancer. This multifaceted approach often leads to improved outcomes by targeting multiple pathways of cancer growth and reducing the chance of resistance. The rationale behind these combinations stems from the complex nature of cancer and the potential for each therapy to enhance the effectiveness of others.The rationale for combining treatments in HER2-positive breast cancer is rooted in the idea that cancer cells are not monolithic.
They possess multiple vulnerabilities, and different therapies can exploit these vulnerabilities in various ways. By simultaneously targeting different aspects of the cancer’s biology, combination therapies aim to achieve a more comprehensive and potent anti-cancer effect, minimizing the chance of the cancer developing resistance to a single treatment modality.
Rationale Behind Combining Therapies
Combining therapies for HER2-positive breast cancer is driven by the complexity of the disease. Cancer cells are not uniformly susceptible to a single treatment. Different therapies target different aspects of the disease, such as hormone production, cell growth, and immune response. By combining therapies, doctors aim to attack cancer cells from multiple angles, leading to greater efficacy and potentially lower risk of resistance.
Successful Combination Therapy Approaches
A range of successful combination therapy approaches have emerged, demonstrating the efficacy of combining various treatment modalities. These strategies aim to maximize efficacy while mitigating side effects. Some of the most commonly used approaches include combining targeted therapies (like HER2-targeted therapies) with chemotherapy regimens, or combining targeted therapies with endocrine therapies to reduce recurrence and improve overall survival.
Examples of Successful Combination Approaches
Examples of successful combination therapies in HER2-positive breast cancer include:
- Targeted Therapy + Chemotherapy: Combining HER2-targeted therapies (e.g., trastuzumab, pertuzumab) with chemotherapy regimens (e.g., anthracyclines, taxanes) has been shown to improve outcomes compared to either therapy alone. This combination often leads to higher response rates and longer disease-free intervals.
- Targeted Therapy + Endocrine Therapy: In cases where the cancer is hormone receptor-positive, combining HER2-targeted therapies with endocrine therapies (e.g., tamoxifen, aromatase inhibitors) can further enhance the effectiveness of treatment. This approach is particularly relevant in pre-menopausal women with hormone receptor-positive tumors.
- Targeted Therapy + Immunotherapy: Recent research is exploring the potential of combining HER2-targeted therapies with immunotherapy approaches (e.g., checkpoint inhibitors). This approach aims to harness the body’s immune system to further attack cancer cells.
Combination Therapy Approaches: A Summary
| Combination Therapy Approach | Components | Potential Benefits | Potential Side Effects |
|---|---|---|---|
| HER2-Targeted Therapy + Chemotherapy | Trastuzumab, Pertuzumab, Docetaxel, Paclitaxel | Improved response rates, longer disease-free intervals, and increased overall survival | Cardiotoxicity, neutropenia, peripheral neuropathy, fatigue |
| HER2-Targeted Therapy + Endocrine Therapy | Trastuzumab, Tamoxifen, or Aromatase inhibitors | Reduced recurrence risk, improved survival, particularly in hormone receptor-positive cases | Hot flashes, vaginal dryness, joint pain, possible bone loss |
| HER2-Targeted Therapy + Immunotherapy | Trastuzumab, Checkpoint inhibitors | Enhanced anti-tumor immune response, potentially improved outcomes | Immune-related adverse events, such as colitis, pneumonitis, and skin reactions |
Novel Treatments and Emerging Research
The landscape of HER2-positive breast cancer treatment is constantly evolving, driven by relentless research and innovation. New targeted therapies and immunotherapies are showing promise in improving outcomes and reducing side effects. This dynamic environment demands a keen understanding of emerging research to optimize patient care.
Emerging Targeted Therapies
Recent advancements in targeted therapy focus on inhibiting specific molecular pathways crucial for HER2-positive cancer growth. These therapies often target different aspects of the HER2 signaling cascade, providing alternative approaches to traditional therapies like trastuzumab. For instance, some therapies are designed to block downstream signaling pathways, preventing the cancer cells from receiving growth signals even if HER2 is activated.
Others are focused on inhibiting the mechanisms that allow cancer cells to develop resistance to existing therapies.
Immunotherapy Approaches
Immunotherapy, which harnesses the body’s own immune system to fight cancer, is gaining significant traction in HER2-positive breast cancer treatment. Researchers are exploring various strategies to enhance the immune response against HER2-positive tumor cells. These strategies include checkpoint inhibitors, which release the brakes on the immune system, and adoptive cell therapies, which use patients’ own immune cells to target the tumor.
Early clinical trials have shown encouraging results, suggesting the potential for improved outcomes and reduced toxicity compared to conventional chemotherapy regimens.
Clinical Trials: Driving Innovation
Clinical trials are essential in translating research findings into practical treatment options. They provide a structured framework for evaluating the safety and efficacy of new therapies, allowing researchers to understand the potential benefits and risks of novel approaches. Participating in clinical trials is a critical component of advancing treatment options for HER2-positive breast cancer.
Navigating treatments for HER2-positive breast cancer can be overwhelming. While focusing on medical approaches, it’s also important to consider your overall well-being. For example, knowing which fruits are rich in magnesium, like the ones listed in this helpful article about what fruit has magnesium , can contribute to a healthier lifestyle. This support can play a crucial role in your journey alongside your chosen cancer treatments.
Designing a Summary Table
A table summarizing emerging treatments should include columns for the treatment name, the mechanism of action, potential benefits (improved efficacy, reduced side effects, etc.), and limitations (potential side effects, resistance development, etc.). A separate column could also highlight the stage of development (e.g., phase I, phase II, phase III). This comprehensive overview allows healthcare professionals and patients to make informed decisions based on the latest evidence.
For example, a table could compare different antibody-drug conjugates, detailing their unique mechanisms and potential side effects.
Example Table Structure (Illustrative)
| Treatment Name | Mechanism of Action | Potential Benefits | Limitations | Stage of Development |
|---|---|---|---|---|
| New Antibody-Drug Conjugate | Targets HER2 and delivers cytotoxic drugs directly to tumor cells. | Potentially higher efficacy, reduced systemic toxicity. | Potential for immune-related adverse events, drug resistance. | Phase II |
| Immunotherapy Combination | Combines checkpoint inhibitor with adoptive cell therapy. | Enhanced anti-tumor immune response. | Potential for severe immune-related side effects. | Phase I/II |
Patient Support and Resources
Navigating a breast cancer diagnosis, especially one as complex as HER2-positive, can be overwhelming. Beyond the medical treatments, emotional support and access to reliable information are crucial for patients and their loved ones. This section Artikels vital resources and strategies for coping.Facing a cancer diagnosis often triggers a range of emotions, from fear and anxiety to anger and sadness.
Building a strong support system, whether through family, friends, or support groups, is essential for managing these feelings. Understanding the disease, its treatment, and potential side effects empowers patients to make informed decisions.
Support Groups and Communities
Support groups offer a safe space for patients to connect with others facing similar experiences. Sharing stories, advice, and coping mechanisms can be incredibly helpful in reducing feelings of isolation and fostering a sense of community. These groups provide emotional support and practical advice, helping individuals feel less alone in their journey. Many support groups are facilitated by trained professionals or experienced cancer survivors.
Emotional Support and Coping Mechanisms
Developing healthy coping mechanisms is essential for managing the emotional challenges associated with cancer treatment. Techniques such as meditation, mindfulness, and deep breathing exercises can help reduce stress and anxiety. Seeking professional counseling or therapy can also provide valuable support and guidance. Support from friends, family, and a strong support network can also significantly impact emotional well-being.
Remembering to prioritize self-care, such as getting enough rest, eating nutritious meals, and engaging in activities that bring joy, is vital.
Accessing Information and Support
Reliable information about HER2-positive breast cancer is essential for patients to make informed decisions about their treatment options. Many organizations and websites offer detailed information, support resources, and guidance for patients and their families. Utilizing these resources effectively can alleviate anxiety and empower individuals to take an active role in their care.
Resources for HER2-Positive Breast Cancer Patients
- National Breast Cancer Foundation (NBCF): Provides comprehensive information about breast cancer, including HER2-positive subtypes. They offer support groups, educational materials, and resources for patients and their families.
- American Cancer Society (ACS): A well-respected organization offering extensive information on breast cancer, including HER2-positive, covering diagnosis, treatment, and support services.
- Susan G. Komen for the Cure: A prominent organization dedicated to breast cancer research and support. They offer resources for patients and their families, including information about HER2-positive breast cancer and support group connections.
- The National Comprehensive Cancer Network (NCCN): Provides clinical practice guidelines and resources for various cancers, including HER2-positive breast cancer, enabling access to information about evidence-based treatment approaches.
- Look beyond these major players. Local cancer centers and hospitals often have support groups, educational programs, and dedicated patient navigators who can provide personalized guidance and assistance.
Closure
In conclusion, treatments for HER2-positive breast cancer are dynamic and evolving. The journey often involves a combination of therapies tailored to the individual patient’s specific needs and characteristics. This comprehensive guide provides a foundational understanding of the available treatments, their potential benefits and drawbacks, and the importance of ongoing research and support for patients. The future of HER2-positive breast cancer treatment is bright, with new and innovative approaches constantly emerging, promising better outcomes and improved quality of life for those affected.