Hip pain that radiates can be a debilitating condition, causing discomfort and affecting daily life. This comprehensive guide delves into the various aspects of radiating hip pain, from its definition and potential causes to diagnostic considerations, treatment options, and preventative measures. We’ll explore the different types of pain, common characteristics, and the underlying conditions that might be at play.
Understanding the specific sensations, potential origins, and associated symptoms is crucial for effective management. This article provides a detailed overview of the causes and characteristics of radiating hip pain, empowering you with knowledge to discuss this with your doctor.
Defining Hip Pain Radiating
Hip pain that radiates is a complex experience characterized by discomfort originating in the hip region but extending to other areas of the body. This type of pain isn’t simply confined to the hip joint itself; instead, it follows specific pathways along nerves or muscles, often creating a pattern that helps in diagnosis. Understanding the nuances of radiating hip pain, including its sensations, potential causes, and characteristics, is crucial for effective treatment and management.This discomfort isn’t a singular sensation; rather, it presents in various forms, from sharp and stabbing to dull and aching, potentially impacting different parts of the body.
The key to understanding radiating hip pain lies in recognizing these different types of pain and their potential origins.
Experiencing hip pain that radiates can be seriously disruptive to daily life. Understanding how this pain affects your ability to perform everyday tasks is crucial. This is where the functional independence measurement comes in handy. It’s a standardized assessment tool that helps healthcare professionals gauge your independence in activities like dressing, bathing, and eating. This assessment can help determine the best course of action for managing your hip pain that radiates and restoring your functional independence.
Types of Pain Sensations
Different types of pain sensations associated with radiating hip pain offer valuable clues about the underlying cause. Sharp, stabbing pain often indicates nerve irritation, while dull, aching pain might suggest muscle strain or inflammation. Burning or tingling sensations could also be present, depending on the specific source of the radiating pain. These varied sensations help to narrow down the potential causes.
Experiencing hip pain that radiates can be a real pain point, literally! Sometimes, seemingly unrelated issues like ear infections, even those connected to COVID-19, ear infection and covid 19 , can surprisingly affect other areas of the body. While less common, it’s always worth checking in with a doctor to rule out any underlying causes for the radiating hip pain.
Potential Causes of Radiating Hip Pain
Numerous factors can contribute to hip pain that radiates. Muscle strains, ligament sprains, and bursitis in the hip region are common culprits. However, radiating hip pain can also be a symptom of more serious conditions, such as nerve impingement, herniated discs, or even referred pain from other parts of the body. Thorough evaluation by a healthcare professional is essential to identify the precise cause.
Common Characteristics of Radiating Hip Pain
Radiating hip pain often exhibits specific characteristics that can aid in diagnosis. The location of the pain typically follows a defined pathway, either along a nerve or muscle group. The intensity of the pain can vary significantly, ranging from mild discomfort to severe agony. Similarly, the duration of the pain can span from a few hours to several days or even weeks, depending on the underlying cause.
Table of Radiating Hip Pain Types and Origins
| Pain Type | Possible Origin | Location |
|---|---|---|
| Sharp, stabbing | Nerve irritation (e.g., sciatica, piriformis syndrome) | Specific area along the radiating path, often following a nerve route. May be accompanied by numbness or tingling. |
| Dull, aching | Muscle strain/inflammation (e.g., hip flexor strain, gluteal muscle strain), bursitis | Broader area, potentially encompassing the hip joint and surrounding tissues. May be worsened by movement or pressure. |
| Burning, tingling | Nerve compression or irritation | Follows a nerve distribution pattern, often accompanied by numbness or weakness in the affected area. |
| Deep, throbbing | Joint issues (e.g., arthritis, hip dysplasia) | Localized to the hip joint, often aggravated by weight-bearing activities or prolonged periods of inactivity. |
Possible Causes

Hip pain that radiates can be a complex issue, stemming from a variety of sources. Understanding the potential causes is crucial for proper diagnosis and treatment. Pinpointing the origin of the pain often involves a careful evaluation of the patient’s medical history, physical examination, and potentially, diagnostic imaging.The radiating nature of the pain suggests a possible connection between the hip and other areas of the body.
This could be due to the involvement of nerves, muscles, or other structures that extend from the hip region. Commonly, this pain extends along nerve pathways or through areas of shared musculoskeletal connections.
Common Musculoskeletal Issues
Musculoskeletal problems are frequent culprits behind radiating hip pain. Muscle strains, often caused by overuse, improper lifting, or sudden movements, can lead to localized pain that may radiate along the affected muscle groups. Bursitis, inflammation of the fluid-filled sacs (bursae) that cushion joints, can also cause radiating pain, especially if the inflamed bursa is near the hip joint.
Degenerative conditions like osteoarthritis, which involves the breakdown of cartilage within a joint, can also cause pain that radiates from the hip, often accompanied by stiffness and limited movement. The pain is frequently felt in the surrounding area of the affected hip joint.
Underlying Medical Conditions
Certain underlying medical conditions can contribute to radiating hip pain. These conditions might not directly affect the hip joint but can indirectly cause pain that spreads to the hip region. For example, conditions affecting the spine, such as herniated discs or spinal stenosis, can compress nerves, leading to pain that radiates down the leg, sometimes including the hip area.
Conditions affecting the lower abdomen or pelvic area, such as inflammatory bowel disease or endometriosis, can also cause referred pain, which might be perceived as radiating from the hip.
Neurological Problems
Neurological issues can significantly contribute to radiating hip pain. Sciatica, a common condition, involves compression of the sciatic nerve, often stemming from a herniated disc or spinal stenosis. This compression can result in pain that radiates down the leg, often accompanied by numbness and tingling. Less common, but potentially serious, are conditions like spinal tumors or nerve root entrapment, which can cause similar radiating pain patterns.
These conditions require immediate medical attention for accurate diagnosis and appropriate management.
Musculoskeletal Conditions Contributing to Radiating Hip Pain
- Muscle strains: Overuse, improper form during exercise, or sudden movements can strain hip muscles, causing pain that may radiate along the affected muscles.
- Bursitis: Inflammation of the fluid-filled sacs (bursae) that cushion joints, especially around the hip joint, can lead to pain that radiates to surrounding areas.
- Osteoarthritis: Degeneration of cartilage within the hip joint can result in pain that spreads to the surrounding tissues, potentially radiating to adjacent areas.
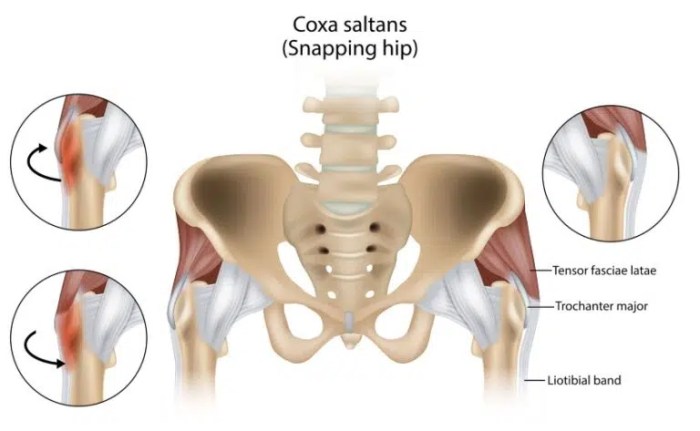
- Trochanteric bursitis: Inflammation of the bursa located on the outer side of the hip can cause pain that radiates along the outer thigh.
- Femoroacetabular impingement (FAI): This condition involves abnormal hip joint mechanics, causing pain that may radiate to the groin or outer thigh.
Comparing Symptoms of Conditions Causing Radiating Hip Pain
| Condition | Symptoms | Possible Radiating Patterns |
|---|---|---|
| Sciatica | Lower back pain, numbness, tingling, weakness in the leg, often following a specific nerve pathway. | Down the leg, possibly hip, buttock, or groin. May be accompanied by shooting or burning pain. |
| Osteoarthritis | Joint pain, stiffness, limited range of motion, often worse with activity. | Around the hip joint, possibly radiating to the groin, buttock, or thigh. May be accompanied by creaking or grinding sounds. |
| Bursitis | Pain, tenderness, and swelling around the affected joint. | Pain can radiate to surrounding areas, depending on the location of the inflamed bursa. |
| Muscle Strain | Localized pain and tenderness, stiffness, difficulty moving the affected area. | Pain may radiate along the affected muscle groups. |
| Herniated Disc | Lower back pain, pain radiating to the buttock and leg, numbness, tingling, weakness in the leg. | Radiating pain often follows the path of the affected nerve root, potentially reaching the hip area. |
Associated Symptoms: Hip Pain That Radiates
Understanding the accompanying symptoms of radiating hip pain is crucial for accurate diagnosis and effective treatment. These additional sensations can significantly impact daily life and provide valuable clues to the underlying cause. The range of symptoms can vary greatly depending on the source of the pain and the affected nerves or structures.The accompanying symptoms of radiating hip pain can provide vital clues to the underlying cause and severity of the problem.
These sensations often extend beyond the hip area, following the pathways of nerves and impacting function in various ways. Paying close attention to the pattern and intensity of these symptoms is essential for effective communication with healthcare professionals.
Experiencing hip pain that radiates can be a real pain! It’s often a tricky situation, and sometimes it’s not just the hip itself. Have you noticed any bumps on the back of your tongue? Sometimes, seemingly unrelated issues, like bumps on back of tongue , can be linked to broader health concerns, including hip pain. It’s important to remember that various conditions can cause radiating hip pain, so it’s always a good idea to consult a doctor.
Sensory Symptoms
Sensory symptoms, such as numbness and tingling, are frequently associated with radiating hip pain. These sensations often follow a specific nerve pathway, radiating down the leg or into the foot. Numbness, a loss of sensation, and tingling, a prickling or itching sensation, can be mild or severe, and are often described as “pins and needles.” For example, sciatica, a common cause of radiating hip pain, frequently presents with numbness and tingling in the buttocks, thigh, and leg.
The precise location and distribution of these sensory disturbances can help pinpoint the affected nerve root.
Motor Symptoms, Hip pain that radiates
Motor symptoms, such as weakness or loss of function, can also accompany radiating hip pain. These symptoms typically arise from nerve compression or damage to the muscles controlled by those nerves. Weakness may manifest as difficulty with specific movements, such as walking, climbing stairs, or lifting objects. The affected muscle groups will often show decreased strength or inability to perform specific functions.
For instance, a herniated disc pressing on a nerve root could result in weakness in the leg muscles, making it difficult to lift the foot or walk.
Autonomic Symptoms
While less common, autonomic symptoms, such as changes in bowel or bladder function, can also accompany radiating hip pain. These symptoms often indicate more severe underlying conditions that affect the autonomic nervous system, which controls involuntary functions like digestion, urination, and heart rate. Examples include urinary incontinence or retention, or changes in bowel habits. The presence of autonomic symptoms warrants prompt medical attention.
Symptom Progression Patterns
The progression of symptoms in radiating hip pain can vary considerably. Some individuals experience a gradual onset of pain and numbness, while others experience sudden, severe symptoms. The rate of progression is influenced by the underlying cause and the individual’s response to treatment. For instance, a gradual worsening of numbness and weakness over weeks could suggest a slow-growing tumor or chronic inflammation, while sudden and severe pain radiating down the leg might indicate a herniated disc.
Comparison with Other Conditions
Differentiating radiating hip pain from other conditions, such as arthritis, muscle strains, or vascular problems, can be challenging. Careful consideration of the specific symptoms, their location, and the pattern of progression is vital for accurate diagnosis. While hip arthritis can cause pain, it usually doesn’t radiate in the same way as nerve-related conditions. Likewise, vascular issues might present with numbness and tingling, but often with additional symptoms like coldness or discoloration of the affected limb.
The presence of accompanying symptoms and their specific distribution can significantly aid in distinguishing radiating hip pain from similar conditions.
Potential Symptom Combinations and Causes
| Symptom | Possible Cause | Potential Radiating Pattern |
|---|---|---|
| Numbness | Nerve compression | Along nerve pathways |
| Weakness | Muscle damage/nerve compression | Affected muscle groups |
| Tingling | Nerve irritation | Along nerve pathways |
| Loss of bowel/bladder control | Severe nerve compression | May not be localized |
| Painful muscle spasms | Muscle strain/inflammation | Localized or radiating to surrounding areas |
Diagnostic Considerations
Pinpointing the precise cause of radiating hip pain requires a systematic approach, combining a thorough medical history, physical examination, and appropriate diagnostic imaging. A detailed understanding of the patient’s symptoms, medical history, and lifestyle factors is crucial for identifying the underlying pathology and guiding treatment decisions. This process ensures that the most effective and appropriate diagnostic measures are employed, minimizing the time and effort required for an accurate diagnosis.The diagnostic process for radiating hip pain involves a multi-faceted approach.
Careful consideration of the patient’s symptoms, combined with a comprehensive physical examination and targeted imaging studies, allows healthcare professionals to identify the root cause of the pain and develop a personalized treatment plan.
Medical History and Physical Examination
A detailed medical history is essential in understanding the context of the radiating hip pain. This includes the onset, duration, location, and intensity of the pain, along with any associated symptoms. The physician will inquire about the patient’s medical history, including any prior injuries, surgeries, or existing medical conditions that might contribute to the pain. Factors such as lifestyle, recent activities, and medications are also considered.
A thorough physical examination is critical for assessing the patient’s range of motion, muscle strength, and neurological function in the affected area. This examination helps to identify potential sources of the pain, such as muscle strains, joint inflammation, or nerve impingement.
Diagnostic Imaging Methods
Various imaging techniques can provide valuable information about the underlying cause of radiating hip pain.
- X-rays: X-rays are useful for evaluating the bony structures of the hip joint, pelvis, and spine. They can reveal fractures, dislocations, or other bony abnormalities. X-rays are generally a first-line imaging modality for suspected skeletal issues. They provide a relatively quick and cost-effective way to assess for bone-related problems that might be contributing to the pain.
- Magnetic Resonance Imaging (MRI): MRI scans provide detailed images of soft tissues, including muscles, ligaments, tendons, and nerves. This is particularly valuable in identifying soft tissue injuries, herniated discs, or inflammatory conditions affecting the hip and surrounding areas. MRI scans are often used to evaluate suspected muscle tears, ligament sprains, or nerve impingements. The high resolution of MRI allows for precise visualization of the structures within the hip region, improving the accuracy of diagnosis.
- Computed Tomography (CT) Scans: CT scans provide detailed cross-sectional images of the hip and surrounding structures. They can be useful in identifying bone abnormalities, tumors, or other structural problems that might be contributing to the pain. CT scans are especially helpful in cases where the cause of the radiating hip pain might be related to bone lesions or tumors. The ability to reconstruct images in different planes allows for a comprehensive assessment of the affected area.
Neurological Assessment
Neurological assessments are crucial for evaluating the potential involvement of nerves in radiating hip pain. These assessments may include evaluating reflexes, sensation, and muscle strength. Neurological tests help identify nerve compression or damage, which can be a source of radiating pain. For example, nerve root impingement from a herniated disc can cause radiating pain down the leg.
Assessing for sensory deficits, muscle weakness, or changes in reflexes is essential for a comprehensive neurological evaluation.
Questions a Doctor Might Ask
A doctor will ask a variety of questions to gather information about the patient’s history, including:
- When did the pain start?
- Where does the pain radiate?
- What makes the pain worse or better?
- What activities exacerbate the pain?
- Are there any other symptoms, such as numbness, tingling, or weakness?
- What is the patient’s medical history?
- Does the patient have any pre-existing conditions that might be contributing to the pain?
Diagnostic Process Steps
The diagnostic process typically involves the following steps:
- Patient history and physical examination: The doctor gathers information about the patient’s symptoms and performs a physical examination to assess the affected area.
- Initial imaging studies: Depending on the initial assessment, X-rays might be ordered to rule out fractures or other bony abnormalities. This is often followed by an MRI or CT scan to assess soft tissues and potentially identify the source of the pain.
- Neurological assessment: If nerve involvement is suspected, specific neurological tests are performed to evaluate nerve function.
- Further testing: If the initial imaging or neurological tests are inconclusive, further tests such as blood tests or specialized imaging studies might be necessary.
Interpreting Diagnostic Imaging Reports
Diagnostic imaging reports, such as X-rays, MRIs, and CT scans, provide visual representations of the anatomical structures within the hip and surrounding regions. Radiologists analyze these images to identify any abnormalities or pathologies. The interpretation of these reports is crucial in determining the underlying cause of the radiating hip pain. For example, an MRI report might highlight a herniated disc, a torn labrum, or a bone spur.
Treatment Options
Navigating the path to recovery from radiating hip pain requires a personalized approach, considering the underlying cause and individual factors. Treatment options range from conservative, non-invasive methods to more intensive surgical interventions. Understanding the potential benefits, risks, and costs associated with each approach is crucial for informed decision-making.Effective treatment plans often involve a combination of therapies, tailored to address the specific needs of the patient.
The goal is to alleviate pain, restore function, and improve overall quality of life.
Conservative Treatment Approaches
Conservative treatments aim to manage symptoms and improve function without surgery. These methods often focus on addressing the root cause of the pain and promoting healing. Physical therapy plays a vital role in this process.
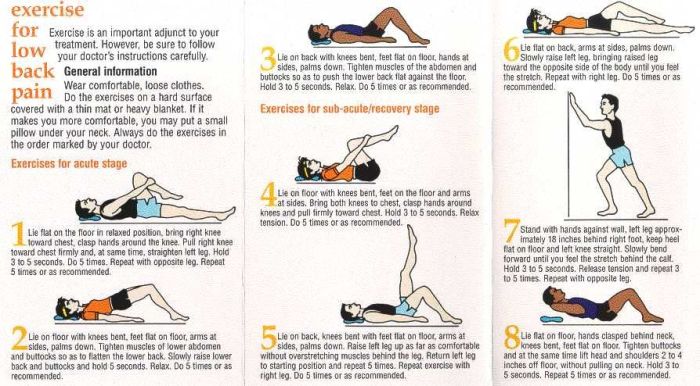
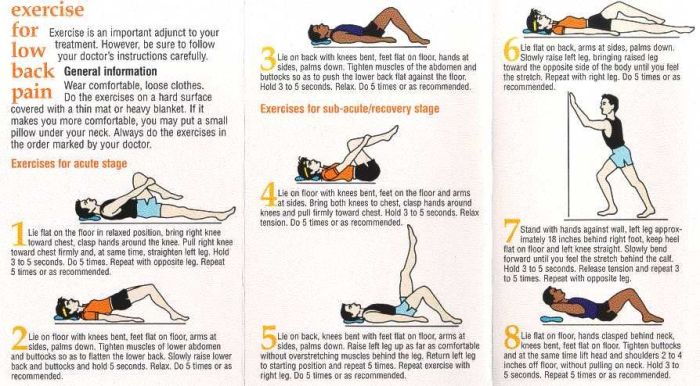
- Physical Therapy: A structured exercise program, guided by a physical therapist, can significantly improve hip mobility, strength, and flexibility. Specific exercises target muscle imbalances, improve posture, and promote proper joint mechanics. This approach can also educate patients on proper body mechanics to prevent future episodes of pain. For example, a patient with piriformis syndrome might benefit from stretching and strengthening exercises to alleviate pressure on the sciatic nerve.
Properly executed exercises can yield substantial improvements in pain management and functional recovery.
- Medication: Pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help reduce inflammation and alleviate pain. Over-the-counter options like ibuprofen or naproxen can be effective for mild to moderate pain. In more severe cases, prescription medications, including stronger pain relievers or corticosteroids, might be necessary. However, long-term use of certain medications may have potential side effects, such as gastrointestinal issues or kidney problems, thus necessitating careful monitoring by a healthcare professional.
- Lifestyle Modifications: Simple changes to daily activities can have a positive impact on hip pain. Maintaining a healthy weight, avoiding prolonged periods of sitting or standing, and incorporating regular low-impact exercise can all contribute to pain management. Examples include incorporating more movement throughout the day, using ergonomic chairs, or modifying workspaces to minimize strain.
Surgical Interventions
Surgical interventions are typically reserved for cases where conservative treatments have failed to provide adequate relief or where the underlying condition necessitates surgical correction. Surgical procedures vary depending on the specific cause of radiating hip pain.
- Arthroscopy: Minimally invasive surgical technique used to diagnose and treat conditions affecting the hip joint. This approach involves small incisions and specialized instruments, potentially leading to faster recovery times. For instance, arthroscopy can be used to repair a torn labrum or remove loose bodies within the joint.
- Hip Replacement: A more extensive surgical procedure where the damaged hip joint is replaced with an artificial implant. This option is considered for severe cases of hip arthritis or other conditions causing significant pain and functional limitations. Careful consideration is needed, as this procedure carries more significant risks and recovery time compared to less invasive options.
Treatment Comparison
| Treatment | Benefits | Risks | Cost |
|---|---|---|---|
| Physical Therapy | Improved mobility, pain relief, improved posture | Requires patient commitment, potential for temporary discomfort | Moderate |
| Medication | Pain relief, inflammation reduction | Side effects possible, potential for dependence | Variable |
| Arthroscopy | Diagnosis and treatment of specific conditions, minimal invasiveness | Risk of infection, bleeding, nerve damage | High |
| Hip Replacement | Significant pain relief, restoration of function | Longer recovery time, potential complications, significant cost | Very High |
Successful Treatment Examples
Individual responses to treatment vary. A successful treatment plan depends on accurate diagnosis, patient compliance, and the chosen course of action. For instance, a patient diagnosed with a herniated disc causing radiating hip pain might benefit from a combination of physical therapy, medication, and lifestyle modifications to manage pain and restore function. Another patient with hip osteoarthritis might require a staged approach, initially focusing on conservative methods and progressing to a hip replacement if necessary.
The goal is to tailor a plan that best addresses the specific needs of each patient.
Prevention and Self-Care
Radiating hip pain can be a debilitating condition, impacting daily life and overall well-being. Proactive measures, coupled with proper self-care, play a crucial role in mitigating the pain and its impact. Understanding how to prevent the condition and effectively manage it at home can significantly improve quality of life.Maintaining a healthy lifestyle is paramount in preventing radiating hip pain.
This involves a multifaceted approach that encompasses posture, exercise, and weight management. Adopting and consistently adhering to these strategies can substantially reduce the risk of developing or exacerbating hip pain.
Strategies for Preventing Radiating Hip Pain
Proper posture is essential for maintaining healthy spinal alignment and reducing strain on the hip joints. Maintaining an upright posture, avoiding slouching, and ensuring proper seating ergonomics, particularly when sitting for prolonged periods, can contribute significantly to preventing hip pain. Using supportive cushions and adjusting chairs to accommodate your body’s natural curvature can also play a vital role in preventing pain.Regular exercise strengthens the muscles supporting the hips, knees, and lower back, thereby enhancing stability and reducing the risk of injury.
Incorporating activities like walking, swimming, and cycling into your routine can promote overall fitness and contribute to hip health. Specific exercises targeting the hip flexors, glutes, and core muscles are also highly beneficial.Weight management is crucial in preventing radiating hip pain. Excess weight puts additional stress on the hip joints, increasing the risk of pain and injury.
Maintaining a healthy weight through a balanced diet and regular exercise can substantially reduce this risk. Even a moderate reduction in weight can significantly lessen the strain on the hip joints.
Importance of Maintaining a Healthy Lifestyle
Maintaining a healthy lifestyle encompasses more than just physical activity. A balanced diet rich in essential nutrients, adequate hydration, and sufficient sleep contribute significantly to overall well-being and can lessen the risk of hip pain. Prioritizing these factors creates a foundation for maintaining healthy joints and minimizing pain.
Practical Advice for Managing Radiating Hip Pain at Home
Managing radiating hip pain at home often involves employing conservative measures like rest, ice, and over-the-counter pain relievers. Resting the affected area can significantly reduce inflammation and pain. Applying ice packs to the affected area for 15-20 minutes at a time, several times a day, can help to reduce swelling and pain. Over-the-counter pain relievers, such as ibuprofen or naproxen, can help manage pain and inflammation.
Do’s and Don’ts for Patients Experiencing Radiating Hip Pain
- Do engage in gentle exercises, such as walking or swimming, to improve flexibility and circulation.
- Do maintain good posture and use supportive cushions when sitting for extended periods.
- Do apply ice packs to the affected area for 15-20 minutes at a time, several times a day.
- Do use over-the-counter pain relievers as directed to manage pain and inflammation.
- Do seek medical advice if pain persists or worsens.
- Don’t engage in strenuous activities that aggravate the pain.
- Don’t ignore the pain and continue activities that exacerbate it.
- Don’t abruptly stop taking medications without consulting your physician.
The above list provides guidelines to help manage radiating hip pain effectively. Following these recommendations can alleviate discomfort and promote healing.
Examples of Exercises and Stretches for Alleviating Radiating Hip Pain
Gentle stretches and exercises can help improve flexibility and reduce pain in the affected area. These should be performed slowly and with caution, avoiding any movement that aggravates the pain.
- Hip Flexor Stretch: Gently pull one knee towards your chest while keeping your back straight. Hold for 15-30 seconds.
- Glute Bridge: Lie on your back with knees bent and feet flat on the floor. Lift your hips off the floor until your body forms a straight line from knees to shoulders. Hold for a few seconds, then lower slowly.
- Knee to Chest Stretch: Lie on your back and gently pull one knee towards your chest. Hold for 15-30 seconds.
These exercises are examples, and it is essential to consult with a healthcare professional to determine the best exercises for your specific condition.
Final Summary
In conclusion, radiating hip pain, while often concerning, can be effectively managed with a combination of self-care, medical attention, and a thorough understanding of the underlying causes. By recognizing the various symptoms, potential origins, and diagnostic considerations, individuals can work collaboratively with healthcare professionals to develop personalized treatment plans. Remember, early diagnosis and proactive management are key to alleviating discomfort and improving overall well-being.