Can you live without your pancreas? This comprehensive guide delves into the fascinating world of pancreatic function, the medical considerations for removal, lifestyle adjustments, long-term effects, and ethical considerations. We’ll explore the vital role the pancreas plays in digestion and hormone regulation, examining the necessary dietary changes and medical procedures involved in managing life without this crucial organ.
From the intricate processes of enzyme production to the complexities of blood sugar control, this exploration will uncover the challenges and triumphs of living with a missing pancreas. We’ll analyze the necessary lifestyle adjustments, including dietary restrictions, medication management, and the importance of emotional well-being. Illustrative case studies and insights into alternative treatment options will round out this detailed examination of a life-altering condition.
Pancreatic Function and Role: Can You Live Without Your Pancreas

The pancreas, a vital organ nestled behind the stomach, plays a crucial dual role in the body’s digestive and endocrine systems. It acts as a crucial intermediary between nutrient intake and energy regulation. This multifaceted function is essential for maintaining overall health and well-being.The pancreas performs both exocrine and endocrine functions. Exocrine secretions aid digestion, while endocrine secretions regulate blood sugar levels.
Understanding these functions helps us appreciate the complexity and importance of this often-overlooked organ.
Pancreatic Digestive Enzymes
The pancreas produces a potent cocktail of enzymes crucial for breaking down the macronutrients (carbohydrates, proteins, and fats) we consume. These enzymes are released into the small intestine, where they complete the digestive process initiated in the mouth and stomach. Without these pancreatic enzymes, complete digestion would be significantly impaired.
- Amylase breaks down complex carbohydrates into simpler sugars like maltose.
- Lipase breaks down fats into fatty acids and glycerol, enabling their absorption.
- Proteases, including trypsin and chymotrypsin, break down proteins into amino acids, the building blocks of new proteins.
Pancreatic Hormones and Blood Sugar Regulation, Can you live without your pancreas
The pancreas also acts as an endocrine gland, producing hormones that regulate blood sugar levels. These hormones, crucial for maintaining energy balance, are vital for preventing dangerous fluctuations in blood glucose.
- Insulin is released when blood sugar levels are high. It facilitates the uptake of glucose by cells, lowering blood sugar levels.
- Glucagon is released when blood sugar levels are low. It stimulates the liver to release stored glucose into the bloodstream, raising blood sugar levels.
Comparison with Other Digestive Organs
The pancreas works in concert with other digestive organs, each contributing unique functions to the overall process. The stomach, for instance, initiates protein digestion, while the liver produces bile for fat emulsification. The pancreas plays a key role in finalizing the breakdown of macronutrients.
| Hormone | Function | Target Organ | Effect |
|---|---|---|---|
| Insulin | Lowers blood glucose | Muscle, liver, adipose tissue | Facilitates glucose uptake, reducing blood sugar levels |
| Glucagon | Raises blood glucose | Liver | Stimulates glycogenolysis (breakdown of glycogen) to release glucose |
| Amylase | Digests carbohydrates | Small intestine | Breaks down starches and glycogen into simpler sugars |
| Lipase | Digests fats | Small intestine | Breaks down triglycerides into fatty acids and glycerol |
| Proteases (Trypsin, Chymotrypsin) | Digests proteins | Small intestine | Breaks down proteins into amino acids |
Living Without a Pancreas
A healthy pancreas is crucial for digestion and blood sugar regulation. Unfortunately, certain medical conditions or injuries may necessitate its removal. This necessitates a comprehensive understanding of the medical implications and lifestyle adjustments required for a fulfilling life after pancreatic removal.
Medical Procedures for Pancreatic Removal
Pancreatic removal, or pancreatectomy, is a complex surgical procedure. The type of pancreatectomy performed depends on the specific reason for removal and the extent of the affected tissue. Laparoscopic pancreatectomies, utilizing small incisions, are increasingly common, offering potential benefits like reduced pain and faster recovery times. Open pancreatectomies, involving larger incisions, are still sometimes necessary, particularly for more extensive procedures or complex cases.
The surgical approach involves meticulous dissection of the pancreas from surrounding structures, ensuring the preservation of critical blood vessels and nerves. Post-operative care is crucial to manage potential complications and promote healing.
Potential Complications of Pancreatic Absence
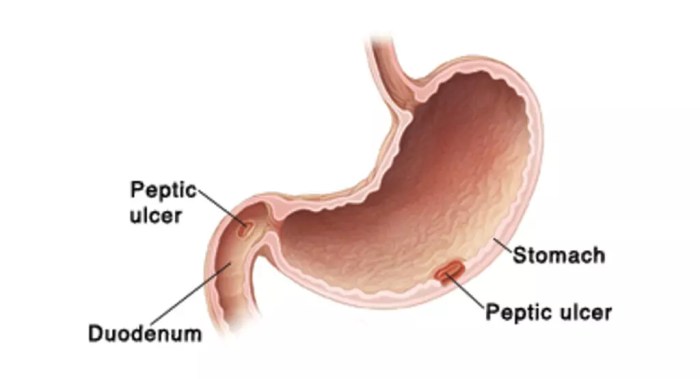
Living without a pancreas can lead to various complications. The most significant concern is the loss of the pancreas’ exocrine and endocrine functions. Exocrine function is vital for digestion, and without it, the body struggles to absorb nutrients from food. Endocrine function, responsible for insulin production, necessitates lifelong management of diabetes. Other potential complications include pancreatitis, infections, bleeding, and problems with bile ducts.
Close monitoring and proactive management are essential to minimize these risks and ensure optimal health outcomes.
Dietary Changes Required for Individuals Without a Pancreas
Individuals without a pancreas require a drastically modified diet. The absence of pancreatic enzymes means that the body struggles to break down fats, proteins, and carbohydrates. A well-structured, easily digestible diet is crucial. Frequent, smaller meals, rather than large ones, are often recommended. Carefully managing carbohydrate intake is also critical to regulate blood sugar levels.
Alternative Methods for Pancreatic Enzyme Replacement
Pancreatic enzyme replacement therapy (PERT) is crucial for individuals without a pancreas. Pancreatic enzyme capsules containing digestive enzymes are taken with meals. These enzymes help to break down nutrients. Alternative methods, such as enzyme replacement via liquid form or via a pancreatic enzyme powder, might be explored. The specific method is tailored to the individual’s needs and preferences.
Dietary Restrictions and Suitable Alternatives
| Restricted Food | Suitable Alternatives |
|---|---|
| High-fat foods (e.g., fried foods, fatty meats) | Lean meats, fish, low-fat dairy products, vegetable-based meals |
| High-fiber foods (e.g., raw vegetables, whole grains) | Well-cooked vegetables, finely ground grains, low-fiber options |
| Highly processed foods | Fresh, whole foods, and minimally processed options |
| Foods high in simple sugars (e.g., candy, sugary drinks) | Fruits, complex carbohydrates, controlled portion sizes |
| Spicy foods | Mild spices, blander options |
This table provides a basic overview. The precise dietary restrictions and suitable alternatives are determined by the individual’s specific needs and medical advice. Consult with a registered dietitian or healthcare professional for personalized dietary guidance.
Lifestyle Adjustments and Management
Living without a pancreas necessitates significant lifestyle adjustments to maintain optimal health and well-being. This includes meticulous management of blood sugar levels, digestive issues, and adherence to prescribed medications. A proactive approach to these areas is crucial for preventing long-term complications and improving quality of life.The absence of the pancreas’s crucial digestive enzymes and insulin-producing cells requires careful planning and execution of daily routines.
This necessitates a profound understanding of how the body functions and how lifestyle choices directly impact health outcomes.
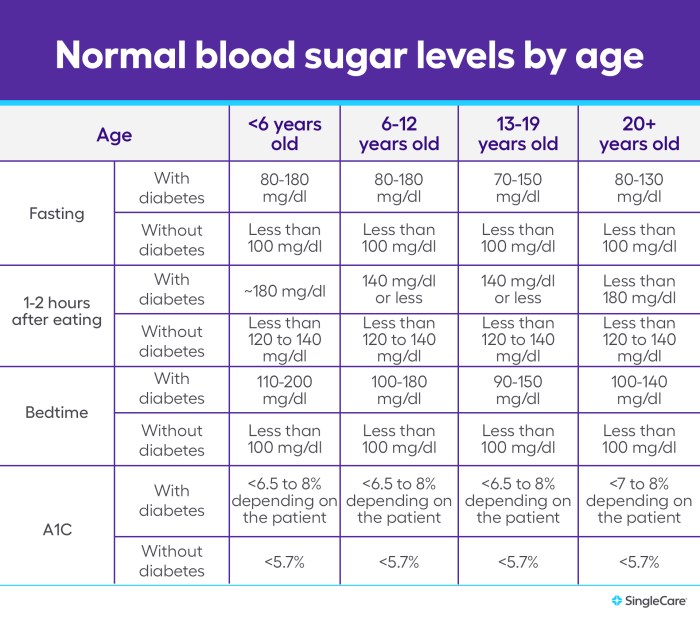
Regular Blood Glucose Monitoring and Management
Maintaining stable blood glucose levels is paramount for individuals without a pancreas. Frequent monitoring and meticulous management are essential to avoid potentially serious complications like hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar). This requires consistent self-testing and adjustments to diet and medication as needed.Regular blood glucose monitoring, typically performed multiple times daily, allows for real-time adjustments to diet and insulin administration.
This ensures that blood glucose levels remain within a target range. Regular consultations with healthcare professionals are vital to fine-tune the monitoring and management strategies.
Managing Digestive Issues and Complications
The absence of pancreatic enzymes can lead to malabsorption of nutrients, causing digestive issues. Dietary modifications are crucial to mitigate these issues. A balanced diet, rich in easily digestible foods, and enzyme supplements are often prescribed.Careful dietary planning plays a vital role in managing digestive complications. The focus should be on easily digestible foods, avoiding high-fat meals and foods that trigger discomfort.
Consultations with registered dietitians are valuable for creating personalized dietary plans that address individual needs and preferences. Enzyme supplements are often required to aid in the digestion of fats, proteins, and carbohydrates.
Adhering to Prescribed Medication and Treatments
Strict adherence to prescribed medications and treatments is critical for managing the various aspects of pancreatic insufficiency. This includes insulin therapy, enzyme replacement therapy, and other medications as needed. Regular follow-up appointments with healthcare providers are essential for monitoring treatment effectiveness and making necessary adjustments.Missing or inconsistent medication can have severe consequences for those living without a pancreas.
Consistent intake, as prescribed by medical professionals, is essential to manage blood glucose levels and digestive processes. Understanding the importance of each medication and its role in maintaining overall health is paramount.
Typical Daily Routine for Someone Without a Pancreas
| Time | Activity | Description |
|---|---|---|
| 7:00 AM | Morning Blood Glucose Check | Checking blood glucose levels upon waking. |
| 7:30 AM | Breakfast | Consuming a balanced breakfast with easily digestible foods. May include enzyme supplements. |
| 8:00 AM | Insulin Injection (if applicable) | Administering insulin as prescribed. |
| 12:00 PM | Lunch | Consuming a balanced lunch with easily digestible foods and enzyme supplements as needed. |
| 3:00 PM | Blood Glucose Check | Monitoring blood glucose levels. |
| 6:00 PM | Dinner | Consuming a balanced dinner with easily digestible foods and enzyme supplements as needed. |
| 8:00 PM | Blood Glucose Check | Monitoring blood glucose levels before bed. |
| 9:00 PM | Evening Insulin Injection (if applicable) | Administering insulin as prescribed. |
This sample routine provides a framework; individual needs may vary. Adjustments are crucial based on individual blood glucose patterns, digestive symptoms, and medication requirements. Regular consultations with healthcare professionals are necessary to adapt the routine as needed.
Long-Term Effects and Quality of Life
Living without a pancreas necessitates a profound adjustment to daily life, impacting various aspects of health and well-being. Managing the chronic conditions that arise demands dedication and resilience. This section explores the long-term effects, the crucial role of support systems, and the strategies for maintaining a fulfilling life despite this significant change.The absence of a pancreas profoundly alters the body’s ability to process nutrients.
This necessitates meticulous dietary management, consistent medication adherence, and proactive monitoring of blood sugar levels. Sustaining a healthy lifestyle, while crucial, can present unique challenges that require careful planning and adaptability.
Impact on Overall Health
Maintaining stable blood sugar levels and managing digestive issues are paramount. The long-term effects of diabetes, a common complication, encompass potential damage to nerves, kidneys, eyes, and cardiovascular system. Furthermore, individuals without a pancreas may experience a heightened risk of developing other complications like pancreatitis or gallstones. Regular medical checkups and adherence to prescribed treatment plans are essential for mitigating these risks and ensuring long-term well-being.
Potential Impact on Physical Well-being
Living without a pancreas requires diligent attention to dietary needs and consistent monitoring of blood glucose levels. This involves meticulous planning of meals and careful selection of foods to manage blood sugar fluctuations. The need for frequent blood glucose monitoring, injections, or digestive enzyme supplements, can become a significant part of daily routines. This requires a high level of self-management and responsibility, and it can significantly impact physical energy levels and lifestyle choices.
So, can you live without your pancreas? The short answer is yes, but it’s not a simple, breezy life. A healthy pancreas is crucial for digestion, and losing that function can be tough. Interestingly, managing the physical and emotional stress that can arise from this condition is vital. If you’re looking into ways to manage stress, checking out this resource on how beta blockers can affect anxiety could be helpful: do beta blockers work for anxiety.
The key is finding healthy ways to cope with the challenges, and ultimately, living a full life despite the pancreatic condition.
For example, strenuous physical activities might require careful planning to avoid hypoglycemia or hyperglycemia.
Potential Impact on Emotional Well-being
The emotional toll of managing a chronic condition like pancreatic insufficiency can be significant. Coping with dietary restrictions, medication schedules, and potential complications can lead to feelings of frustration, anxiety, or even depression. Building a strong support network, including family, friends, and support groups, can be vital in navigating these emotional challenges.
Support Systems Available
Access to comprehensive medical care is crucial for effective management. This includes endocrinologists, gastroenterologists, and diabetes educators, who can provide expert guidance and support. Support groups for individuals with pancreatic conditions offer a valuable platform for sharing experiences, exchanging advice, and receiving emotional support from peers. Furthermore, many healthcare systems provide specialized care and support groups specifically for those who have undergone pancreatic surgeries.
Maintaining a High Quality of Life
Despite the challenges, maintaining a high quality of life is entirely possible. Individuals without a pancreas can lead fulfilling lives by prioritizing their health, managing their condition effectively, and seeking support when needed. Adopting healthy coping mechanisms, maintaining a balanced lifestyle, and nurturing social connections are key elements in this process. This often involves finding activities that provide joy and a sense of purpose, whether it’s pursuing hobbies, engaging in social interactions, or participating in support groups.
Managing the Condition and Maintaining Well-being
Individuals without a pancreas typically manage their condition through a combination of dietary modifications, medication adherence, regular medical checkups, and diligent monitoring of blood glucose levels. It’s essential to work closely with healthcare professionals to develop a personalized management plan. Maintaining a healthy lifestyle, including regular exercise and stress management techniques, plays a vital role in overall well-being.
Furthermore, fostering a supportive environment, whether through family, friends, or support groups, can greatly enhance emotional resilience and improve quality of life.
Ethical and Social Considerations
Living without a pancreas presents a unique set of ethical and social challenges, demanding careful consideration of individual autonomy, societal support, and evolving medical advancements. These considerations extend beyond the purely medical realm, touching upon the individual’s quality of life, their relationships, and their place within society. Navigating these complexities requires a compassionate and informed approach.The decision to undergo pancreatic removal is deeply personal, often driven by the need to alleviate severe pain or manage life-threatening complications.
So, can you actually live without your pancreas? The answer, surprisingly, is yes, but it’s not a walk in the park. Modern medical advancements, like the innovative procedures detailed in the latest updates on pancreatic transplants and related research in what’s new in mash , are making it possible for people to manage without this crucial organ.
However, it requires careful management and ongoing monitoring. Living without a pancreas isn’t a simple matter, but it’s definitely a testament to medical progress.
However, the long-term implications, including dietary restrictions, medication management, and potential for long-term health complications, must be fully understood and weighed against the potential benefits. This necessitates open communication and shared decision-making between the patient, family, and medical team.
Ethical Considerations Surrounding Pancreatic Removal
The ethical landscape surrounding pancreatic removal encompasses several key aspects. Informed consent, a fundamental principle in medical ethics, becomes crucial. Patients must be fully informed about the procedure’s potential benefits, risks, and alternatives before making an autonomous decision. This includes understanding the long-term effects on their health and lifestyle. Furthermore, the ethical considerations extend to the allocation of scarce resources in healthcare systems, especially when dealing with complex and costly treatments.
Balancing individual needs with societal resources is a critical aspect of ethical practice in healthcare.
Social Implications of Living with a Chronic Health Condition
Living with a chronic health condition like the absence of a pancreas can significantly impact social interactions. Individuals may experience challenges in social settings, including mealtimes, social events, and even simple everyday interactions. They may face stigma or misunderstandings about their condition, potentially impacting their relationships and opportunities. Social support systems play a crucial role in mitigating these difficulties.
They provide emotional support, practical assistance, and a sense of community.
Support Systems and Resources
Adequate support systems are essential for individuals living without a pancreas. These include family, friends, and support groups. Patient advocacy organizations offer valuable resources, connecting individuals with others who share similar experiences. These groups provide a platform for sharing information, coping strategies, and mutual support. Medical professionals, including endocrinologists, dieticians, and psychologists, also play a vital role in providing comprehensive care.
Accessible and tailored support programs are essential to maintain a positive quality of life.
Ever wondered if you could live without your pancreas? While it’s a vital organ, a person can indeed survive with a transplant or by managing the resulting complications. This, however, often leads to digestive issues. Understanding these digestive concerns is key when considering the potential differences between Irritable Bowel Syndrome (IBS) and colon cancer, as they can sometimes share similar symptoms.
For a deeper dive into the subtle distinctions between IBS and colon cancer, check out this helpful resource: ibs vs colon cancer. Ultimately, the answer to living without a pancreas depends on prompt medical attention and effective management strategies.
Impact of Medical Advancements
Medical advancements, such as improved surgical techniques, diabetes management, and nutritional therapies, are continually enhancing the outlook for those living without a pancreas. These advancements have led to increased survival rates and improved quality of life. For example, advancements in insulin delivery systems have enabled more precise control of blood sugar levels, minimizing complications. These developments have created a more optimistic and realistic perspective for those navigating this challenging condition.
Importance of Empathy and Understanding
Empathy and understanding are paramount in supporting individuals living without a pancreas. It’s crucial to recognize the unique challenges they face, such as dietary restrictions, medication management, and potential long-term health complications. Educating oneself about the condition can foster empathy and understanding, creating a more supportive environment. Active listening and genuine concern for the individual’s well-being are essential components of effective support.
Creating a culture of understanding and respect can help individuals with pancreatic conditions to lead fulfilling lives.
Illustrative Case Studies
Living with a missing pancreas requires significant adjustments to daily life. Understanding the experiences of those who have undergone this procedure provides valuable insights into the challenges and triumphs of managing this condition. The following case study offers a glimpse into the personal journey of a patient who has had their pancreas removed.
Case Study: Sarah’s Journey
Sarah, a 45-year-old woman, was diagnosed with pancreatic cancer. Following extensive medical evaluations and discussions with her healthcare team, a pancreatectomy was deemed necessary. This involved the surgical removal of her pancreas.
Surgical Recovery and Initial Challenges
Sarah’s initial recovery period was marked by typical post-operative discomfort and the need for careful monitoring. She experienced nausea, fatigue, and pain, all common side effects of major abdominal surgery. Early days were focused on regaining strength and managing pain effectively. The surgical intervention significantly impacted her digestion, leading to immediate dietary restrictions and the need for specialized nutritional support.
Dietary Restrictions and Medication Management
Sarah’s post-operative diet was meticulously planned to ensure optimal nutrient intake while mitigating digestive issues. Her diet was low in fat and high in easily digestible carbohydrates. She also needed to take enzyme supplements to aid in digestion and absorption of nutrients. Her medication regimen included enzyme replacements, insulin, and other supportive medications to address potential complications.
Lifestyle Adjustments and Emotional Well-being
The removal of her pancreas required significant lifestyle adjustments. Sarah had to incorporate regular exercise into her routine to maintain her physical well-being. She also needed to manage potential long-term complications, like diabetes and exocrine pancreatic insufficiency. Her emotional journey involved adjusting to the significant life changes. She faced periods of anxiety and uncertainty, but through supportive therapy and a strong network of family and friends, she was able to navigate these challenges.
Sarah found support through online forums and support groups for pancreatic patients, connecting with others who understood her experiences.
Support System and Coping Strategies
Sarah’s support system played a crucial role in her recovery and emotional well-being. Her husband provided constant emotional support, and her close friends organized regular get-togethers to help maintain her social connections. Regular communication with her medical team, including dietitians and endocrinologists, was essential for managing her condition. She actively sought out educational resources and materials to understand her condition thoroughly.
This knowledge empowered her to take an active role in managing her health.
Long-Term Outcomes and Quality of Life
While Sarah’s life after the pancreatectomy was significantly altered, she adapted and found ways to maintain a fulfilling life. She remained committed to her dietary restrictions, medication schedule, and lifestyle adjustments. Regular follow-up appointments with her healthcare providers ensured proactive monitoring of her health. Sarah demonstrated resilience and determination in managing her condition, emphasizing the importance of proactive self-management.
Despite the challenges, she maintained a positive outlook and continued to pursue her interests, like gardening and spending time with her family. Her experiences highlight the importance of personalized care and the need for comprehensive support systems.
Alternative Treatment Options and Future Research
Living without a pancreas presents significant challenges, but ongoing research offers hope for improved quality of life. This section explores promising alternative treatments and the future of pancreatic care, focusing on regenerative medicine and replacement therapies. The quest for better outcomes for individuals facing this condition is a key area of medical advancement.
Regenerative Medicine for the Pancreas
Regenerative medicine aims to repair or replace damaged tissues, holding immense potential for treating pancreatic insufficiency. Scientists are investigating various strategies to stimulate the pancreas’s natural ability to regenerate, potentially eliminating the need for lifelong enzyme supplementation. This approach involves using stem cells and growth factors to encourage the growth of new pancreatic tissue. Early-stage research has shown promising results in animal models, and clinical trials are underway to assess the safety and efficacy of these approaches in humans.
Pancreatic Replacement Therapies
Researchers are actively pursuing various pancreatic replacement therapies to alleviate the symptoms of pancreatic insufficiency. One promising area involves developing artificial pancreatic islets, which are clusters of cells that produce insulin and other hormones. These artificial islets could be implanted to regulate blood sugar levels and potentially reduce the need for insulin injections. Another area of focus involves developing bioengineered pancreatic tissue or organs.
These bioengineered constructs could potentially mimic the function of a healthy pancreas, offering a more complete replacement solution.
New Technologies and Approaches
Several innovative technologies are being explored to enhance pancreatic care. 3D bioprinting is emerging as a powerful tool for creating functional pancreatic tissues in the lab. By precisely layering cells and biomaterials, researchers aim to fabricate tissues that closely resemble natural pancreatic tissue. Gene therapy holds potential for modifying cells to produce the necessary pancreatic enzymes, addressing the underlying cause of the condition.
Nanotechnology offers the possibility of delivering drugs or therapies directly to pancreatic cells, enhancing the efficacy of treatments.
Areas for Further Research
While promising, research in pancreatic regeneration and replacement therapies faces challenges. Understanding the complex interplay of factors influencing pancreatic regeneration is crucial. Further investigation into the optimal timing and delivery methods for stem cells and growth factors is necessary. Developing reliable and cost-effective methods for large-scale production of bioengineered pancreatic tissues is vital. The long-term safety and efficacy of these therapies need rigorous evaluation in human trials.
Comparison of Treatment Approaches
| Treatment Approach | Description | Effectiveness | Limitations |
|---|---|---|---|
| Regenerative Medicine (Stem Cells) | Stimulates pancreas regeneration using stem cells and growth factors. | Promising early results in animal models; clinical trials ongoing. | Long-term efficacy and safety in humans require further evaluation. |
| Artificial Pancreatic Islets | Implanted clusters of cells to regulate blood sugar and hormone production. | Potential for reducing reliance on insulin injections. | Development of long-term compatibility and stability is essential. |
| Bioengineered Pancreatic Tissue/Organs | Mimics the function of a healthy pancreas, offering a more complete replacement. | High potential for long-term function. | Complexity of the process and cost-effectiveness of large-scale production. |
| 3D Bioprinting | Creates functional pancreatic tissue using 3D printing technology. | Potential to produce customized pancreatic tissue. | Long-term viability and integration of the printed tissue. |
| Gene Therapy | Modifies cells to produce necessary pancreatic enzymes. | Potential for addressing the underlying cause of the condition. | Potential risks associated with gene editing and long-term effects. |
Final Conclusion
In conclusion, living without a pancreas presents a unique set of challenges, but also demonstrates remarkable resilience and adaptability. The interplay of medical procedures, dietary adjustments, and lifestyle modifications underscores the importance of comprehensive support systems and ongoing research. Ultimately, this exploration highlights the dedication and strength of individuals facing this condition and the vital role of medical advancements in improving their quality of life.
We hope this guide offers a deeper understanding and compassion for those navigating this complex journey.