Why do people die in their sleep? This question touches upon a deeply unsettling aspect of human life, prompting us to explore the various factors that can contribute to sudden death during slumber. From underlying medical conditions to sleep disorders, drug interactions, and environmental influences, the causes are multifaceted and often complex. Understanding these factors is crucial for raising awareness and potentially preventing such tragedies.
This exploration delves into the intricate interplay of medical conditions, sleep disturbances, and external factors that can lead to sleep-related fatalities. We’ll examine the role of genetics, lifestyle choices, and even environmental conditions in increasing the risk of death during sleep. By understanding these factors, we can better appreciate the importance of preventative measures and early intervention.
Underlying Medical Conditions
Sudden death during sleep, though often alarming, can be linked to various underlying medical conditions. Understanding these conditions is crucial for recognizing potential risks and implementing preventative measures. Early detection and appropriate medical interventions can significantly reduce the likelihood of such tragic events.
Common Medical Conditions Increasing Sleep-Related Death Risk
Several medical conditions can increase the risk of sudden death during sleep. These conditions often involve disruptions to the heart’s rhythm, breathing patterns, or the body’s ability to regulate essential functions during sleep.
- Cardiovascular Diseases: Conditions like coronary artery disease, heart failure, and arrhythmias can compromise the heart’s ability to pump blood effectively. Disruptions in blood flow, especially during sleep when the body is at rest, can lead to sudden cardiac arrest. For example, a patient with undiagnosed coronary artery disease might experience a fatal arrhythmia during sleep, interrupting the normal rhythm and causing the heart to stop beating.
Early detection and management of cardiovascular conditions through regular check-ups and lifestyle modifications can greatly reduce the risk.
- Respiratory Conditions: Obstructive sleep apnea (OSA) is a common sleep disorder characterized by pauses in breathing during sleep. These pauses can reduce the amount of oxygen reaching the brain and other vital organs. In severe cases, OSA can lead to cardiac arrhythmias and, in some cases, sudden death. Asthma and other respiratory illnesses can also increase the risk of sleep-related deaths due to impaired breathing and decreased oxygen levels.
For instance, an individual with untreated asthma experiencing a severe attack during sleep might struggle to breathe, leading to oxygen deprivation and potentially fatal consequences.
- Neurological Conditions: Some neurological disorders, such as stroke, can disrupt the brain’s control over vital functions, including breathing and heart rate. A stroke affecting areas controlling breathing or the cardiovascular system during sleep can lead to fatal complications. Furthermore, certain neurological conditions can directly impact the heart’s rhythm and function, resulting in sudden cardiac arrest. For example, a patient with a history of stroke might experience a fatal arrhythmia triggered by sleep-related changes in blood pressure and oxygen levels.
Importance of Routine Check-ups and Preventative Measures
Regular medical check-ups play a vital role in identifying and managing underlying conditions that increase the risk of sleep-related fatalities. Routine screenings can detect potential problems early, allowing for prompt interventions and preventive measures. This proactive approach can significantly reduce the likelihood of sudden death during sleep.
- Lifestyle Modifications: Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking, can significantly reduce the risk of various medical conditions. For instance, adopting a heart-healthy diet can reduce the risk of cardiovascular diseases, a major contributor to sleep-related deaths.
- Medication Adherence: Proper adherence to prescribed medications is essential for managing underlying conditions and minimizing complications. Consistent medication use helps to control blood pressure, cholesterol levels, and other factors associated with cardiovascular and respiratory diseases. Furthermore, it is important to consult with a healthcare provider if there are concerns about side effects or drug interactions.
- Sleep Hygiene Practices: Establishing healthy sleep habits, such as maintaining a regular sleep schedule, creating a conducive sleep environment, and avoiding caffeine and alcohol before bedtime, can promote better sleep quality and reduce the risk of sleep disorders like OSA.
Risk Assessment Table
| Condition | Risk Factors | Symptoms | Preventive Measures |
|---|---|---|---|
| Cardiovascular Disease | High blood pressure, high cholesterol, smoking, obesity | Chest pain, shortness of breath, dizziness | Regular check-ups, medication adherence, healthy diet, exercise |
| Obstructive Sleep Apnea (OSA) | Obesity, large neck circumference, family history | Loud snoring, gasping for air during sleep, daytime sleepiness | Weight loss, CPAP therapy, lifestyle modifications |
| Neurological Disorders | History of stroke, brain injury, neurological conditions | Headache, weakness, numbness, loss of coordination | Regular check-ups, medication adherence, management of underlying conditions |
Sleep Disorders: Why Do People Die In Their Sleep
Sleep, a fundamental human need, is often overlooked as a crucial factor in overall health. Beyond simply feeling rested, adequate sleep plays a vital role in regulating numerous bodily functions, including breathing, heart rate, and hormone production. Disruptions to this delicate balance, often stemming from sleep disorders, can increase the risk of serious health problems, some of which can lead to sudden death.
Sleep Apnea and Sudden Death
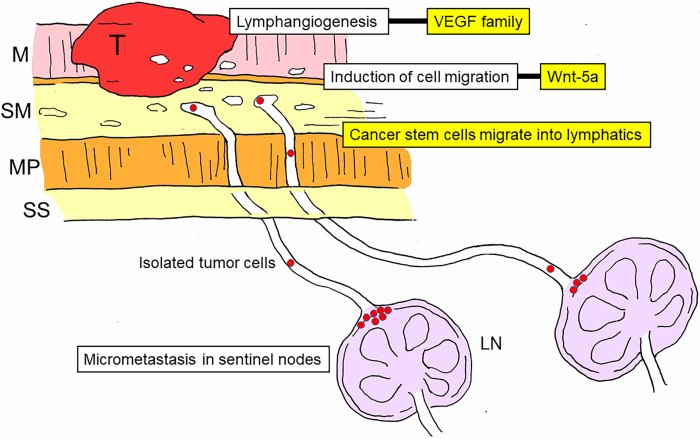
Sleep apnea, characterized by pauses in breathing during sleep, is a serious sleep disorder. These pauses, called apneas, can drastically reduce the amount of oxygen reaching the brain and body. Repeated episodes of oxygen deprivation over time can strain the cardiovascular system, increasing the risk of high blood pressure, heart disease, and stroke. Furthermore, the constant disruption of normal breathing patterns during sleep can trigger irregular heart rhythms, potentially leading to sudden cardiac death.
The risk is particularly elevated in individuals with pre-existing cardiovascular conditions. A significant number of sudden unexplained deaths have been linked to sleep apnea.
Impact of Other Sleep Disorders
Beyond sleep apnea, other sleep disorders can also negatively affect sleep-related mortality. Narcolepsy, a neurological disorder characterized by excessive daytime sleepiness and sudden attacks of sleep, can disrupt normal sleep patterns and increase the risk of accidents. Restless legs syndrome, marked by uncomfortable sensations in the legs and an irresistible urge to move them, can lead to poor sleep quality, affecting overall health.
Both narcolepsy and restless legs syndrome, while not directly causing sudden death in the same way as sleep apnea, can contribute to a decline in health, increasing vulnerability to other life-threatening conditions.
Disruptions to Breathing Patterns and Heart Function
Sleep disorders can severely disrupt breathing patterns and heart function during sleep. In sleep apnea, the repeated pauses in breathing cause a significant drop in oxygen levels, placing a strain on the cardiovascular system. This can lead to irregular heart rhythms and high blood pressure, increasing the risk of heart attack or stroke. Narcolepsy can cause sudden, unexpected episodes of muscle weakness, which can compromise breathing.
Similarly, restless legs syndrome can disrupt sleep, reducing the time spent in restorative deep sleep and leading to fatigue and potential health issues.
Comparison of Sleep Disorders
| Sleep Disorder | Symptoms | Diagnostic Procedures |
|---|---|---|
| Sleep Apnea | Loud snoring, gasping or choking sounds during sleep, daytime sleepiness, morning headaches, dry mouth, and waking up with a sore throat. | Polysomnography (sleep study) to measure breathing patterns, brain activity, heart rate, and oxygen levels during sleep. Medical history and physical examination. |
| Narcolepsy | Excessive daytime sleepiness, sudden attacks of sleep, cataplexy (sudden loss of muscle tone), sleep paralysis, and hypnagogic hallucinations. | Detailed medical history, sleep diaries, multiple sleep latency test (MSLT) to measure the speed of falling asleep during daytime naps, and polysomnography. |
| Restless Legs Syndrome | Uncomfortable sensations in the legs, an irresistible urge to move the legs, and worsening symptoms at night. Symptoms are often worse in the evening and at rest. | Detailed medical history, sleep diaries, physical examination, and a neurological examination to rule out other conditions. Sleep study (polysomnography) may be used to assess the sleep disruption. |
Drug Interactions and Substance Abuse
Sleep-related deaths can tragically be linked to a complex interplay of factors, including pre-existing conditions and sleep disorders. However, another significant contributor is the interaction of medications and substances with the body’s natural sleep processes. Understanding how various drugs and substances affect respiratory function and sleep patterns is crucial for recognizing potential risks. This section will explore the potential dangers of drug interactions and substance abuse in relation to sleep-related fatalities.Drug interactions can disrupt the delicate balance of physiological processes, particularly during sleep, potentially leading to fatal consequences.
Sometimes, people die peacefully in their sleep, but other times, underlying health conditions play a role. It’s easy to overlook the toll that caring for someone can take, leading to burnout. This can manifest in various ways, like exhaustion, irritability, or a lack of motivation. Understanding the signs of caregiver burnout is crucial for ensuring both the caregiver and the cared-for individual receive the necessary support.
Ultimately, a multitude of factors can contribute to unexpected deaths during sleep, highlighting the importance of prioritizing health and well-being.
This disruption can involve multiple systems, including the respiratory and cardiovascular systems, both of which are crucial for maintaining life during sleep. The effects of drug interactions and substance abuse on sleep-related deaths are often compounded by the individual’s pre-existing health conditions and lifestyle choices.
Potential Drug Interactions
Many medications, when taken together or with alcohol, can have unpredictable and potentially dangerous effects on sleep. This includes medications for various conditions, including but not limited to, pain relief, anxiety, and high blood pressure. The risk is amplified when these drugs are taken in combination or at higher dosages than recommended.
Role of Alcohol and Substance Abuse
Alcohol significantly impacts sleep architecture, often leading to fragmented sleep and impaired respiratory function. This impairment is particularly dangerous during sleep, as the body’s natural defenses are reduced. Furthermore, combining alcohol with other sedatives or depressants can result in a synergistic effect, increasing the risk of respiratory depression and potentially fatal consequences. Similarly, the abuse of other substances, such as opioids, can have a detrimental impact on respiratory function during sleep.
Effects of Different Drugs on Sleep Patterns and Respiratory Function, Why do people die in their sleep
Different drugs affect sleep patterns and respiratory function in various ways. Some drugs, such as benzodiazepines, can promote relaxation and sleep but also depress respiratory function, increasing the risk of sleep apnea and cessation. Opioids, known for their pain-relieving properties, can also depress breathing, especially when combined with other sedatives or alcohol. Stimulants, while often used to combat sleepiness, can lead to insomnia and disrupt sleep patterns, potentially increasing stress on the respiratory system.
Table of Drugs and Potential Risks During Sleep
| Drug Type | Potential Risks During Sleep |
|---|---|
| Benzodiazepines | Increased risk of respiratory depression, sleep-disordered breathing, and fatal outcomes, especially when combined with alcohol or other sedatives. |
| Opioids | Significant risk of respiratory depression, potentially leading to cessation during sleep, particularly in combination with other central nervous system depressants. |
| Sedatives (e.g., barbiturates) | Highly increased risk of respiratory depression, significantly impacting breathing during sleep and posing a life-threatening risk, especially when combined with alcohol or other sedatives. |
| Alcohol | Disrupts sleep architecture, leading to fragmented sleep, impaired respiratory function, and increased risk of sleep-related death, especially when combined with other sedative substances. |
| Stimulants | May cause insomnia and disrupt sleep patterns, potentially increasing stress on the respiratory system, but not typically leading to respiratory arrest in isolation. |
External Factors and Environmental Influences
Sleep-related deaths aren’t always due to internal medical issues. External factors, including environmental conditions and sleep positions, can significantly impact breathing and heart function during sleep, sometimes leading to fatal outcomes. Understanding these external factors is crucial for preventative measures and promoting safer sleep environments.Certain environmental conditions can create an environment that negatively affects the body’s ability to maintain healthy respiration and circulation during sleep.
This can be particularly dangerous for individuals with underlying health issues or those who are already vulnerable.
Environmental Conditions Affecting Breathing
Environmental conditions significantly influence sleep quality and safety. Factors like temperature, humidity, and even air quality can alter breathing patterns and heart rate, potentially leading to respiratory distress and sleep-related fatalities. For instance, extremely cold temperatures can constrict airways, making breathing more difficult. Conversely, excessive heat can lead to hyperthermia, further compromising breathing function. Exposure to allergens or pollutants in the air can exacerbate existing respiratory conditions or trigger allergic reactions during sleep.
Sleep Positions and Their Impact
Sleep positions can also play a critical role in sleep-related deaths. Certain positions can obstruct breathing pathways, particularly for individuals who are predisposed to sleep apnea or respiratory issues. For example, sleeping on the stomach can compress the chest and abdomen, hindering the natural expansion of the lungs. Similarly, sleeping in positions that put pressure on the airways can disrupt breathing patterns, increasing the risk of sleep apnea and related complications.
It is also important to note that infants and children are particularly vulnerable to positional asphyxia, emphasizing the need for safe sleep practices.
Impact of Temperature, Humidity, and Other Factors
Temperature fluctuations, humidity levels, and even the presence of certain substances in the air can impact the body’s physiological responses during sleep. For example, extreme temperatures can trigger physiological responses that interfere with breathing and heart function. High humidity can also affect respiratory function and increase the risk of respiratory infections, potentially exacerbating sleep-related problems. Additionally, the presence of irritants or pollutants in the air can negatively affect breathing and cardiovascular function.
Summary Table of External Factors and Their Potential Effects
| External Factor | Potential Effect on Sleep |
|---|---|
| Extreme Temperatures (High/Low) | Increased risk of hyperthermia or hypothermia, affecting breathing and heart rate. |
| High Humidity | Increased risk of respiratory infections, potential interference with breathing. |
| Air Quality (Pollutants, Allergens) | Exacerbation of existing respiratory conditions, triggering allergic reactions, and affecting breathing. |
| Sleep Positions (e.g., Stomach Sleeping) | Potential airway obstruction, hindering breathing and oxygen intake. |
| Exposure to Irritants/Substances | Negative impact on respiratory and cardiovascular function. |
Genetic Predisposition and Family History
Understanding sleep-related deaths often requires looking beyond immediate factors. Genetic predisposition plays a significant role, influencing an individual’s susceptibility to certain conditions that can lead to unexpected sleep-related mortality. A family history of sudden death, particularly in seemingly healthy individuals, can signal an underlying genetic vulnerability that warrants further investigation.Family history of sudden death, especially in young or seemingly healthy individuals, can serve as a crucial warning sign.
This heightened risk often points to a genetic component that may predispose individuals to a range of sleep-related disorders or conditions. While environmental and lifestyle factors are crucial, a genetic predisposition can significantly increase the chances of such occurrences.
Genetic Factors in Sleep-Related Deaths
Genetic factors can contribute to a range of sleep disorders and conditions that increase the risk of sleep-related mortality. Variations in genes can affect the function of the heart, respiratory system, and brain, making individuals more prone to abnormalities during sleep. These variations can be passed down through generations, creating a familial pattern of sudden death.
Examples of Genetic Conditions
Certain genetic conditions are directly linked to sleep-related deaths, impacting the body’s ability to regulate vital functions during sleep. These conditions can manifest subtly, and individuals may not exhibit any symptoms during wakefulness.
- Long QT Syndrome: This genetic disorder affects the electrical activity of the heart. Prolonged QT intervals can increase the risk of sudden cardiac arrest, often occurring during sleep. Examples include cases where young athletes unexpectedly collapse during exercise or sleep, or individuals with a family history of sudden cardiac arrest without clear cause.
- Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC): This condition leads to structural abnormalities in the heart, particularly the right ventricle. These abnormalities can disrupt the heart’s rhythm, potentially causing fatal arrhythmias during sleep. Individuals with a family history of unexplained cardiac events, especially those involving the right ventricle, should be evaluated for this condition.
- Sudden Infant Death Syndrome (SIDS): While the exact cause of SIDS remains largely unknown, some genetic predispositions may play a role in the vulnerability to this condition, especially in certain ethnic groups. This is a crucial area of ongoing research. A family history of SIDS in multiple children can suggest a need for genetic testing and careful monitoring of subsequent children.
Table of Genetic Conditions Associated with Sleep-Related Deaths
The following table Artikels some genetic conditions associated with sleep-related deaths, highlighting their potential impact on cardiac function and the importance of familial history assessment.
Sometimes, people die in their sleep due to underlying conditions. While a seemingly unrelated issue like shoulder pain when throwing shoulder pain when throwing might not directly cause death, it can be a symptom of more serious health problems. These issues, if left unchecked, can contribute to unexpected fatalities during sleep. So, while sleep is often a time of rest, it’s crucial to address potential health concerns to improve your overall well-being.
| Genetic Condition | Potential Impact on Sleep | Impact on Mortality |
|---|---|---|
| Long QT Syndrome | Disrupts heart’s electrical activity, potentially causing fatal arrhythmias during sleep. | Increased risk of sudden cardiac arrest, often during sleep. |
| Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) | Structural abnormalities in the heart disrupt rhythm, potentially causing fatal arrhythmias during sleep. | Increased risk of sudden cardiac arrest, often during sleep. |
| Familial Hypertrophic Cardiomyopathy | Thickening of heart muscle can interfere with blood flow and potentially lead to abnormal heart rhythms during sleep. | Increased risk of sudden cardiac arrest, especially during strenuous physical activity or stress, but also potentially in sleep. |
Age and Life Stage
The delicate balance of life, from infancy to old age, often impacts the susceptibility to sleep-related deaths. Different stages of life present varying vulnerabilities due to developmental factors, physiological changes, and environmental exposures. Understanding how age influences sleep-related fatalities is crucial for preventative measures and appropriate interventions.The risk of sleep-related deaths is not uniform across all age groups.
Factors like the immaturity of the nervous system in infants, the ongoing development of the body and brain in children, and the physiological changes associated with aging in adults and the elderly all contribute to the distinct patterns of sleep-related fatalities.
Infancy
Infant mortality is unfortunately a significant concern, and sleep-related deaths in this stage are often associated with Sudden Infant Death Syndrome (SIDS). Factors like unsafe sleep environments, soft bedding, and overheating contribute to this risk. The immaturity of the infant’s nervous system, respiratory system, and thermoregulation mechanisms make them vulnerable to disruptions in breathing during sleep. Premature babies and those with underlying health conditions are at an even higher risk.
Childhood
Childhood sleep-related deaths, though less common than in infancy, can be associated with underlying medical conditions, sleep disorders, or accidental suffocation. Children may experience sleep apnea, which can disrupt breathing during sleep. They might also be susceptible to accidents if the sleep environment is not adequately monitored or safe. Furthermore, conditions like certain types of epilepsy or heart conditions can increase risk.
Adulthood
Sleep-related deaths in adulthood encompass a wider range of potential causes. Cardiovascular conditions, sleep apnea, and drug interactions or substance abuse can all play significant roles. As adults age, the risk of developing conditions like heart failure or stroke increases, and these can manifest as sleep-related deaths. Sleep disorders such as sleep apnea, narcolepsy, or restless leg syndrome can increase vulnerability.
Old Age
In older adults, sleep-related deaths can be linked to various factors. Chronic conditions, like heart disease, respiratory issues, or neurological disorders, are more prevalent. These conditions can increase the risk of respiratory problems during sleep. Additionally, medications or interactions between medications can cause adverse reactions, leading to sleep-related fatalities. Cognitive decline and mobility issues can also contribute to sleep-related risks in this age group.
Correlation Between Age and Sleep-Related Deaths
| Age Group | Potential Causes | Specific Examples |
|---|---|---|
| Infancy (0-1 year) | SIDS, unsafe sleep environments, underlying medical conditions, prematurity | Improper bedding, overheating, respiratory issues |
| Childhood (1-18 years) | Sleep apnea, suffocation, underlying medical conditions, accidents | Sleep disorders, unsafe sleep environments, accidental suffocation |
| Adulthood (19-64 years) | Cardiovascular conditions, sleep apnea, drug interactions, substance abuse, underlying medical conditions | Heart disease, stroke, sleep apnea, prescription drug interactions, alcohol abuse |
| Old Age (65+ years) | Chronic conditions, medications, cognitive decline, mobility issues, respiratory issues | Heart failure, respiratory problems, neurological disorders, medication side effects |
Lifestyle Factors

Our daily habits profoundly impact our sleep quality and, consequently, our risk of sleep-related deaths. A balanced lifestyle, encompassing diet, exercise, and stress management, plays a crucial role in maintaining healthy sleep patterns. Poor sleep hygiene, in turn, can contribute to various health problems, increasing vulnerability to sleep-related complications. Understanding the link between lifestyle choices and sleep-related mortality is essential for preventative measures.
The Influence of Diet on Sleep
Diet significantly influences sleep quality. Consuming excessive amounts of caffeine, alcohol, and processed foods can disrupt sleep patterns. Conversely, a balanced diet rich in fruits, vegetables, and whole grains can promote better sleep. Foods high in magnesium and tryptophan, crucial for melatonin production, are beneficial for sleep. For example, a diet rich in sugar can lead to energy crashes and subsequent difficulty falling asleep.
Similarly, a late-night dinner laden with heavy proteins or fats can create digestive discomfort and impede sleep. A balanced diet is key to maintaining stable blood sugar levels, promoting restful sleep.
The Importance of Regular Exercise
Regular physical activity is crucial for overall health, and it significantly impacts sleep quality. Exercise releases endorphins, which have mood-boosting effects. However, exercising too close to bedtime can energize the body, making it difficult to fall asleep. Finding a suitable time for exercise, ideally several hours before bedtime, is essential for optimal sleep. For instance, a vigorous workout right before sleep can interfere with sleep onset and duration.
Conversely, regular exercise, especially aerobic activity, has been shown to improve sleep quality and duration in many studies.
Stress Management and Sleep
Chronic stress is a significant contributor to sleep disturbances. Stress hormones like cortisol interfere with the body’s natural sleep-wake cycle. Stress management techniques, such as meditation, yoga, and deep breathing exercises, can help regulate stress levels and improve sleep quality. For instance, individuals experiencing high levels of stress may find it difficult to relax and fall asleep, often resulting in insomnia and other sleep disorders.
Incorporating stress-reducing activities into daily routines can significantly improve sleep quality and reduce the risk of sleep-related issues.
Sleep Hygiene and Mortality
Maintaining good sleep hygiene is paramount for preventing sleep-related mortality. Consistent sleep schedules, a conducive sleep environment, and avoiding excessive screen time before bed are key elements of good sleep hygiene. Individuals who maintain consistent sleep schedules are more likely to experience quality sleep and reduce the risk of sleep-related mortality. For instance, irregular sleep schedules can disrupt the body’s natural circadian rhythm, making individuals more susceptible to sleep-related problems.
Correlation Between Lifestyle Choices and Sleep-Related Deaths
| Lifestyle Choice | Potential Impact on Sleep | Potential Impact on Sleep-Related Mortality |
|---|---|---|
| High caffeine intake | Difficulty falling asleep, disrupted sleep | Increased risk of sleep-related complications |
| Irregular sleep schedule | Disrupted circadian rhythm, poor sleep quality | Increased risk of sleep-related deaths |
| High stress levels | Difficulty relaxing, insomnia | Increased vulnerability to sleep-related complications |
| Lack of regular exercise | Poor sleep quality, reduced energy levels | Potential increase in sleep-related deaths |
| Unhealthy diet | Digestive issues, poor blood sugar regulation | Increased risk of sleep-related issues and health problems |
Illustrative Case Studies
Unveiling the mysteries surrounding sudden unexpected deaths in sleep requires a deep dive into specific case studies. These real-world examples, while tragic, offer valuable insights into the diverse factors contributing to sleep-related fatalities. Understanding the diagnostic process and outcomes can help medical professionals refine their approaches to prevention and treatment.Analyzing specific cases illuminates the complex interplay of underlying medical conditions, sleep disorders, and external factors that can lead to fatal consequences.
The detailed accounts highlight the critical role of accurate diagnosis and prompt intervention in mitigating the risk of sleep-related deaths.
Case Study 1: Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) is a prevalent sleep disorder characterized by pauses in breathing during sleep. These pauses can lead to a dangerous drop in blood oxygen levels and disrupt the body’s natural restorative processes.This case involves a 55-year-old male with a history of hypertension and obesity. He presented with progressively worsening sleepiness and daytime fatigue. Sleep studies revealed severe OSA, with frequent apneic episodes and low oxygen saturation.
Sudden death in sleep can be a mystery, often linked to underlying health issues. Factors like high blood pressure and, significantly, cholesterol heart disease, particularly prevalent in African Americans, cholesterol heart disease and african americans , can contribute to these tragic events. This highlights the importance of regular check-ups and proactive health management to minimize such risks.
Despite lifestyle modifications and CPAP therapy, the patient experienced a sudden cardiac arrest during sleep. Autopsy confirmed the presence of severe cardiac fibrosis and significant pulmonary hypertension, directly attributable to the chronic sleep apnea. The diagnostic process involved a thorough medical history, physical examination, and polysomnography. The outcome was a tragic and untimely death, highlighting the importance of early diagnosis and aggressive management of OSA.
Case Study 2: Underlying Cardiovascular Disease
Certain underlying cardiovascular conditions can increase the risk of sudden death during sleep. These conditions may manifest with subtle symptoms or remain undiagnosed until a critical event.A 68-year-old female with a history of coronary artery disease, hypertension, and diabetes presented with intermittent chest pain and shortness of breath. She reported experiencing palpitations and lightheadedness before the incident. An electrocardiogram (ECG) and cardiac enzyme tests were performed.
While the ECG revealed some abnormalities, the results were not immediately alarming. However, further investigation and analysis of her medical history revealed a significant risk for cardiac events. Sadly, she succumbed to a cardiac arrhythmia during sleep. The diagnostic process focused on her symptoms, medical history, and cardiac assessments. The outcome underscored the need for careful monitoring and prompt intervention for patients with known cardiovascular risk factors.
Case Study 3: Drug-Induced Respiratory Depression
The interaction of medications with natural sleep processes can sometimes have fatal consequences. Patients taking certain medications may be at a heightened risk of respiratory depression, leading to cessation of breathing during sleep.A 70-year-old male taking a combination of opioid painkillers and sedatives for chronic pain experienced sudden respiratory arrest during sleep. The patient’s medical history revealed a history of chronic pain and pre-existing respiratory conditions.
Initial investigations indicated a probable interaction between the prescribed medications, leading to respiratory depression. The diagnostic process included analyzing the patient’s medication regimen, reviewing medical history, and performing blood gas analysis. The outcome emphasized the importance of careful medication management and close monitoring in patients with pre-existing respiratory conditions.
Summary of Case Studies
| Case Study | Patient Demographics | Medical History | Diagnostic Process | Outcome |
|---|---|---|---|---|
| 1 | 55-year-old male | Hypertension, obesity | Sleep studies, medical history | Sudden cardiac arrest |
| 2 | 68-year-old female | Coronary artery disease, hypertension, diabetes | ECG, cardiac enzyme tests, medical history | Cardiac arrhythmia |
| 3 | 70-year-old male | Chronic pain, pre-existing respiratory conditions | Medication review, blood gas analysis | Respiratory arrest |
Prevention Strategies

Reducing the risk of sleep-related deaths requires a multi-faceted approach that addresses both individual and societal factors. Proactive measures, combined with increased public awareness, can significantly lower the incidence of these tragic events. This involves understanding the potential contributing factors and implementing strategies to mitigate their impact.
Public Awareness Campaigns and Education Programs
Effective prevention relies heavily on educating the public about the risks associated with various sleep-related conditions and behaviors. Public awareness campaigns play a crucial role in disseminating information about recognizing the warning signs and taking preventive measures. These campaigns can highlight the importance of maintaining healthy sleep hygiene, identifying potential sleep disorders, and seeking professional help when necessary. They can also address misconceptions surrounding sleep and encourage individuals to prioritize sleep health.
Targeted educational programs can be delivered in schools, workplaces, and community centers, reaching a wide range of demographics. For example, a campaign focusing on sleep apnea in older adults could emphasize the connection between untreated sleep apnea and increased risk of cardiovascular issues.
Early Detection and Intervention in Sleep Disorders
Prompt identification and treatment of sleep disorders are vital for preventing sleep-related deaths. Early detection allows for intervention, reducing the progression of potentially life-threatening conditions. Recognizing the symptoms of sleep disorders, such as snoring, gasping for air during sleep, daytime sleepiness, and difficulty concentrating, is crucial. This early identification is often the key to successful treatment and the prevention of severe consequences.
A thorough sleep study by a qualified professional can accurately diagnose sleep disorders, including conditions like sleep apnea and narcolepsy, enabling appropriate treatment plans to be implemented. For example, an early diagnosis of sleep apnea could lead to the use of a CPAP machine, which significantly reduces the risk of sleep-related complications.
Preventive Measures and Lifestyle Adjustments
Maintaining healthy sleep habits and lifestyle choices can significantly reduce the risk of sleep-related deaths. These include establishing a regular sleep schedule, creating a relaxing bedtime routine, optimizing the sleep environment, and avoiding excessive caffeine or alcohol consumption close to bedtime. Also, a balanced diet and regular exercise can contribute to better sleep quality. A structured approach to improving sleep habits, coupled with professional guidance when needed, is essential.
For example, encouraging regular physical activity in adolescents can lead to better sleep quality and reduced risk of sleep-related breathing problems.
Examples of Successful Prevention Programs
Several successful prevention programs have been implemented in various communities and settings. These programs often combine educational components with targeted interventions for specific populations at risk. One program might focus on providing sleep hygiene education in senior centers, while another could partner with schools to promote healthy sleep habits in adolescents. For instance, a program designed to help people with pre-existing medical conditions understand the potential for sleep-related deaths would emphasize the importance of consistent medical monitoring and prompt reporting of symptoms.
The success of such programs hinges on their adaptability to diverse populations and the involvement of relevant healthcare providers and community organizations. Moreover, ongoing evaluation and adjustment based on data and feedback are critical for maximizing the impact of these prevention initiatives.
Final Review
In conclusion, the reasons behind sleep-related deaths are diverse and multifaceted. From underlying medical issues and sleep disorders to drug interactions, environmental factors, and genetic predispositions, a range of factors contribute to this often-unpredictable outcome. While some causes are unavoidable, understanding the contributing factors is vital in developing preventive strategies and promoting public awareness. Early detection and intervention remain crucial for mitigating risks and ultimately saving lives.