What is CMV cytomegalovirus? This comprehensive guide delves into the world of cytomegalovirus (CMV), exploring its characteristics, transmission, diagnosis, treatment, prevention, complications, and impact on specific populations. We’ll uncover the intricacies of this common virus, providing a clear and accessible overview for anyone seeking information.
From its basic structure and lifecycle to its effects on various individuals, this article provides a detailed yet easily understandable look at CMV. Understanding CMV is crucial for recognizing symptoms, seeking appropriate medical care, and taking preventative measures.
Definition and Overview
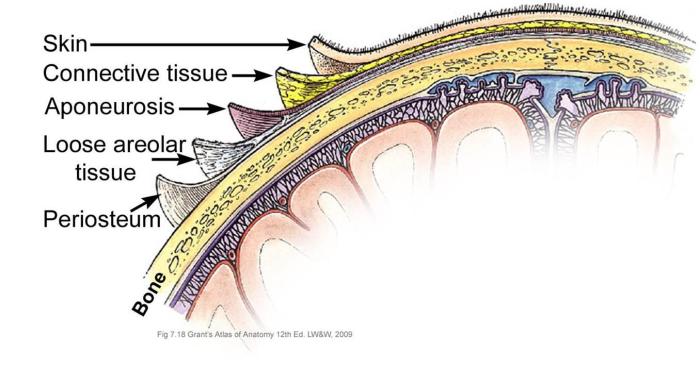
Cytomegalovirus (CMV) is a common herpesvirus that infects a significant portion of the global population. While often asymptomatic, CMV can cause severe complications, especially in individuals with weakened immune systems. Understanding its characteristics, transmission methods, and potential symptoms is crucial for effective prevention and management.CMV is a large DNA virus, typically 150-250 nanometers in size, exhibiting a characteristic enveloped structure.
The envelope contains viral proteins that facilitate infection. Its complex structure allows it to evade the host’s immune response and replicate effectively.
Transmission Methods
CMV can be transmitted through various routes. Direct contact with infected bodily fluids, such as saliva, urine, or semen, is a primary mode of transmission. This is frequently associated with close personal contact, such as between family members. Furthermore, transmission can occur through blood transfusions or organ transplants, highlighting the importance of screening for CMV in these procedures.
CMV, or cytomegalovirus, is a common virus that often causes no symptoms, but can be problematic during pregnancy. It’s important to understand that while you might be curious about getting pregnant during your period, that’s a different question entirely. Fortunately, you can find detailed information on whether pregnancy is possible during menstruation here. Regardless of your menstrual cycle, if you’re concerned about CMV, it’s crucial to talk to your doctor.
They can provide personalized advice and guidance on managing potential risks, ensuring a healthy pregnancy outcome.
Congenital transmission from a mother to her fetus during pregnancy is another significant route.
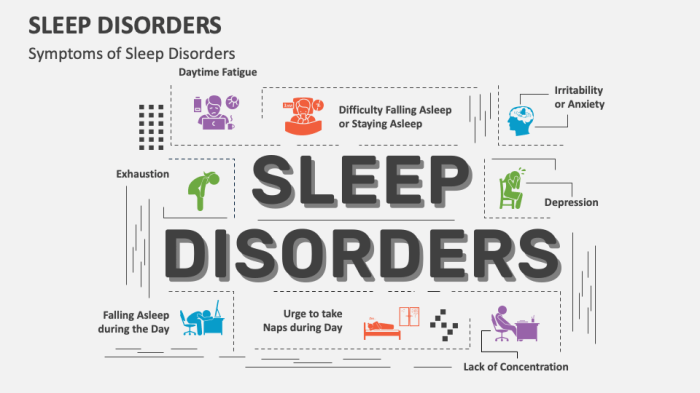
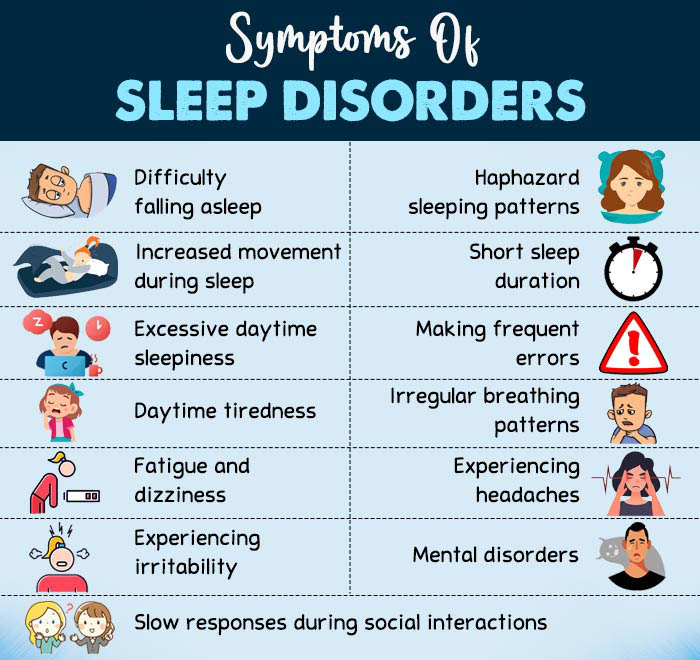
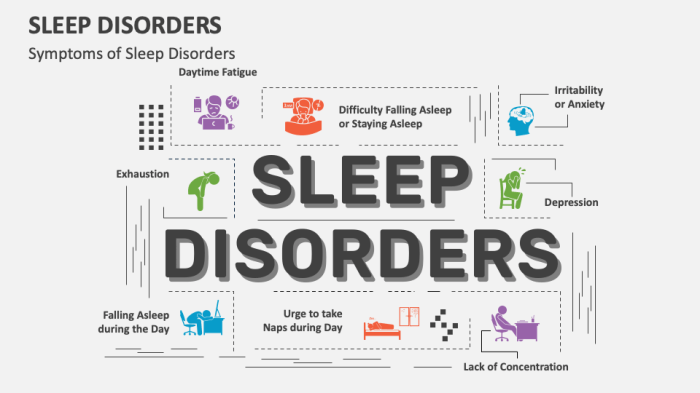
Symptoms of CMV Infection
The clinical manifestations of CMV infection are highly variable. Many individuals experience no noticeable symptoms, especially those with healthy immune systems. In symptomatic cases, symptoms may resemble those of a mild flu or mononucleosis. These include fever, fatigue, sore throat, swollen glands, and headaches. However, more severe complications can arise in immunocompromised individuals.
Comparison with Other Viral Infections
CMV infections often present with nonspecific symptoms, making them difficult to distinguish from other viral illnesses like Epstein-Barr virus (EBV) infections or influenza. Diagnostic tests are crucial for accurate identification. Key differences lie in the specific symptoms, as well as the underlying immunological response of the host. For instance, EBV infections typically result in a more pronounced lymphadenopathy (swollen lymph nodes) than CMV.
CMV Replication Lifecycle
Understanding the stages of CMV replication is vital for developing effective antiviral therapies. The virus’s complex lifecycle involves multiple steps, starting with entry into the host cell and culminating in the release of new virions.
| Stage | Description |
|---|---|
| Entry | The virus binds to specific receptors on the host cell surface, facilitating entry into the cell. |
| Replication | Viral DNA is transcribed into mRNA, which is then translated into viral proteins. Viral DNA is also replicated, leading to the production of numerous viral components. |
| Assembly | Viral components are assembled to form new virions. This intricate process involves the assembly of structural proteins and viral genetic material. |
| Release | Mature virions are released from the infected cell, potentially infecting other cells, continuing the cycle. The release process often involves lysis of the host cell. |
Types and Strains

Cytomegalovirus (CMV) isn’t a single entity; it encompasses a diverse range of strains. Understanding these variations is crucial for comprehending the virus’s behavior and developing targeted treatments. While these variations don’t fundamentally change the nature of the disease, they do affect its severity and potential complications, particularly in immunocompromised individuals. This knowledge helps clinicians tailor management strategies and anticipate potential outcomes.
Different Strains of CMV
Various strains of CMV exhibit slight genetic variations. These differences, while subtle, can influence the virus’s replication rate, immune response activation, and overall clinical manifestations. Though the basic mechanisms of infection remain similar, the specific way each strain interacts with the host can lead to differing disease presentations.
Prevalence of CMV Strains
The prevalence of specific CMV strains can vary geographically and within different populations. Factors like exposure patterns, hygiene practices, and overall health conditions in a community can all influence the relative frequency of specific CMV strains. Studies have shown a correlation between the prevalence of certain strains and the incidence of specific CMV-related complications.
Comparison of CMV Strains
| Strain | Replication Rate | Immune Response Activation | Associated Characteristics | Prevalence (Example) ||—|—|—|—|—|| Strain A | Moderate | Moderate | Mild symptoms, often asymptomatic; higher prevalence in developed nations. | 60% in North America || Strain B | High | High | Severe symptoms, rapid progression; common in immunocompromised individuals; higher prevalence in developing nations. | 40% in Sub-Saharan Africa || Strain C | Low | Low | Relatively benign; often asymptomatic or with mild symptoms; prevalence linked to specific geographic regions.
| 20% in Eastern Europe || Strain D | High | High | Associated with severe congenital infections; higher prevalence in populations with poor sanitation practices. | 10% in South Asia |Note: These are illustrative examples, and the prevalence figures are not absolute. More detailed research is required to accurately quantify the prevalence of specific CMV strains across diverse populations.
Additionally, the characteristics of a strain can vary depending on the host’s immune status. The table provides a generalized overview, and individual cases may deviate.
Diagnosis and Testing
CMV, or cytomegalovirus, can be tricky to diagnose, especially in the absence of obvious symptoms. Accurate diagnosis is crucial for appropriate treatment and management, particularly in vulnerable populations. Various methods are employed to detect the presence of CMV and its impact on the body.
CMV, or cytomegalovirus, is a common virus that often causes mild or no symptoms. While it can sometimes be problematic for those with weakened immune systems, interestingly, some research suggests potential benefits from incorporating foods like moringa into your diet. This plant, as detailed in the uses and benefits of moringa , boasts various nutrients and antioxidants.
Ultimately, understanding CMV is key to managing your overall health.
Common Diagnostic Methods
Several methods are used to detect CMV infection, ranging from simple blood tests to more complex molecular assays. These methods aim to identify the virus itself, its genetic material, or the immune response to the infection. Understanding the specific characteristics of each method is vital for interpreting the results accurately.
Polymerase Chain Reaction (PCR)
PCR is a powerful molecular technique that detects CMV DNA or RNA in various samples, including blood, urine, and tissue biopsies. The procedure involves isolating the viral genetic material from the sample and then amplifying it through repeated cycles of heating and cooling. This process creates millions of copies of the viral genetic material, making it detectable even when the viral load is low.
The interpretation of PCR results depends on the specific threshold for detection. A positive result indicates the presence of CMV, while a negative result suggests the absence of CMV. The sensitivity of PCR is high, allowing for early detection of CMV infection, even before the appearance of clinical symptoms. The specificity of PCR is also generally high, meaning that false-positive results are rare.
Antibody Testing
Antibody tests are used to detect the immune response to CMV. These tests measure the presence of antibodies produced by the body in response to the CMV infection. The procedure involves analyzing a blood sample for the presence of specific antibodies. These antibodies can be IgM or IgG, and the presence and levels of each type of antibody can provide valuable information about the timing and severity of the infection.
CMV, or cytomegalovirus, is a common virus that often causes mild or no symptoms. While it’s usually harmless, it can be a concern for those with weakened immune systems. Interestingly, some research explores potential links between inositol supplementation and managing PCOS symptoms, a condition that sometimes affects women’s fertility. Learning more about inositol for pcos info might provide insight into how certain nutrients can impact overall health.
Regardless, understanding CMV and its potential implications remains important for anyone concerned about their well-being.
Interpretation of the results depends on the type of antibody detected and its concentration. A positive IgM antibody result suggests a recent CMV infection, while a positive IgG antibody result suggests a past or current infection. The accuracy of antibody tests varies depending on the stage of the infection and the specific test used.
Other Diagnostic Tests
Other diagnostic methods include viral culture, which involves growing the virus in a laboratory setting, and immunohistochemistry, which identifies CMV antigens in tissues. While these methods are sometimes used, PCR and antibody testing are more commonly used in clinical practice.
Comparison of Diagnostic Tests
| Diagnostic Test | Procedure | Pros | Cons | Accuracy/Sensitivity |
|---|---|---|---|---|
| PCR | Detects CMV DNA/RNA in samples | High sensitivity, can detect low viral loads, early detection possible | Requires specialized equipment and trained personnel, can be expensive | Generally high, with low false-positive rates |
| Antibody Testing | Detects antibodies produced in response to CMV | Relatively inexpensive, readily available | Lower sensitivity than PCR, may not detect acute infections, can be affected by past infections | Moderate, accuracy varies depending on the stage of infection |
| Viral Culture | Growing the virus in a laboratory | Direct confirmation of CMV presence | Time-consuming, requires specialized facilities, low sensitivity | Low, not a preferred method |
| Immunohistochemistry | Identifies CMV antigens in tissues | Useful for tissue-based diagnoses | Can be less sensitive than PCR, requires specialized expertise | Moderate, dependent on the tissue sample |
Treatment and Management
Cytomegalovirus (CMV) infection, while often manageable, requires careful monitoring and tailored treatment approaches. Understanding the various treatment options, their efficacy, and potential side effects is crucial for effective patient management. This section delves into the specifics of CMV treatment, focusing on diverse patient populations and the importance of proactive measures to prevent complications.The available treatments for CMV infection are primarily antiviral medications.
Their effectiveness varies depending on the severity of the infection and the patient’s overall health. Early detection and prompt initiation of treatment are critical to minimizing the risk of long-term complications. Careful consideration of potential side effects and adherence to treatment protocols are essential aspects of managing CMV infection.
Antiviral Medications
A range of antiviral medications are used to treat CMV infections, primarily targeting the viral replication process. These drugs often have different mechanisms of action and varying degrees of efficacy.
- Ganciclovir is a commonly prescribed antiviral that inhibits viral DNA synthesis. It’s often the first-line treatment for CMV retinitis and other serious infections. However, it can cause significant side effects, including neutropenia (low white blood cell count), thrombocytopenia (low platelet count), and gastrointestinal issues. Monitoring blood counts is crucial during treatment with ganciclovir.
- Valganciclovir is a prodrug of ganciclovir, offering improved oral bioavailability and reduced frequency of administration. Its efficacy is similar to ganciclovir, but with a more convenient dosing schedule. Similar side effects to ganciclovir may occur.
- Cidofovir is another antiviral that inhibits viral DNA synthesis. It is often used in cases where ganciclovir or valganciclovir is not effective or is poorly tolerated. Cidofovir can cause nephrotoxicity (kidney damage), and careful monitoring of kidney function is necessary. It’s often administered intravenously.
- Foscarnet is a broad-spectrum antiviral that inhibits viral DNA polymerase. It’s typically used as a second-line treatment for CMV infections, particularly when other drugs are ineffective or not well-tolerated. Foscarnet can also cause nephrotoxicity, and close monitoring of kidney function is crucial.
Patient-Specific Management Strategies
Effective CMV management considers the specific needs of different patient populations. This involves tailoring treatment duration, dosage, and monitoring protocols based on factors like the patient’s underlying health conditions, the severity of the infection, and the presence of other infections.
- Immunocompromised Patients: Patients with weakened immune systems, such as those undergoing organ transplantation or with HIV/AIDS, are at higher risk of severe CMV infections. Treatment durations may be longer, and close monitoring is essential to manage potential side effects and prevent complications.
- Pregnant Women: CMV infections during pregnancy can pose risks to the developing fetus. Treatment options and monitoring strategies are carefully chosen to balance the benefits of treatment against potential risks to both the mother and the baby.
- Children: CMV infections in children may manifest differently than in adults, and treatment approaches are adapted accordingly. Monitoring for long-term effects and potential developmental delays is important.
Importance of Early Detection and Treatment
Early detection and prompt initiation of treatment are vital in preventing severe complications from CMV infection. Early intervention can reduce the severity of the infection and minimize the risk of long-term organ damage or other complications. Early diagnosis often translates to better outcomes and a more favorable prognosis.
Precautions During Treatment
Adherence to treatment protocols and careful monitoring of potential side effects are crucial during CMV treatment. Patients should report any unusual symptoms to their healthcare provider immediately.
- Monitoring Blood Counts: Regular blood tests to monitor white blood cell and platelet counts are essential, particularly when using ganciclovir or valganciclovir, to prevent serious side effects.
- Hydration: Maintaining adequate hydration is important, especially when taking medications that can cause kidney damage.
- Dietary Considerations: Following a balanced diet and adhering to any specific dietary recommendations provided by the healthcare team can help manage potential side effects.
Treatment Comparison Table
| Treatment | Mechanism of Action | Common Side Effects | Effectiveness |
|---|---|---|---|
| Ganciclovir | Inhibits viral DNA synthesis | Neutropenia, thrombocytopenia, GI issues | Generally effective, but can cause severe side effects |
| Valganciclovir | Prodrug of ganciclovir | Neutropenia, thrombocytopenia, GI issues | High bioavailability, convenient dosing |
| Cidofovir | Inhibits viral DNA polymerase | Nephrotoxicity | Effective in some cases, requires careful monitoring |
| Foscarnet | Inhibits viral DNA polymerase | Nephrotoxicity, neurological issues | Used as a last resort |
Prevention and Control

Cytomegalovirus (CMV) infection, while often asymptomatic, can have severe consequences for vulnerable populations. Proactive prevention and control strategies are crucial in mitigating the risk of infection and its associated complications. Understanding the measures available, particularly in high-risk settings like healthcare facilities, is essential for safeguarding individuals and preventing outbreaks.
Preventive Measures
Effective prevention hinges on a multi-faceted approach that encompasses individual hygiene practices, targeted screening, and meticulous control measures in high-risk environments. This proactive approach is vital in limiting the spread of CMV and protecting those most susceptible.
- Hygiene Practices: Maintaining meticulous hand hygiene is paramount in preventing CMV transmission. Frequent and thorough handwashing with soap and water, particularly after contact with potentially contaminated surfaces or individuals, is crucial. Proper disposal of contaminated materials, like used tissues or medical waste, is also critical to interrupt the transmission cycle. Using disposable items where possible and proper disinfection of surfaces in shared spaces are essential practices.
- Vaccination: Currently, there is no widely available CMV vaccine. Research into CMV vaccines is ongoing, but at present, preventive measures focus on avoiding exposure and reducing transmission.
- Screening High-Risk Populations: Routine screening for CMV is recommended for pregnant women and individuals with weakened immune systems, such as transplant recipients. Early detection allows for appropriate management and minimizes the risk of complications. Identifying those with latent CMV infections enables targeted interventions and reduces the potential for transmission.
Controlling CMV Spread in Healthcare Settings
Controlling CMV transmission in healthcare settings is a critical component of patient safety. A robust system for preventing transmission, especially in areas with high patient turnover or immunocompromised individuals, is essential.
- Infection Control Protocols: Implementing strict infection control protocols is paramount. These protocols should include dedicated equipment for each patient, appropriate disposal of contaminated materials, and rigorous hand hygiene practices for all staff. Proper cleaning and disinfection of surfaces and equipment are essential components of effective infection control.
- Contact Precautions: Implementing contact precautions, including the use of personal protective equipment (PPE), for patients with suspected or confirmed CMV infections is critical. This includes the use of gowns, gloves, and eye protection to minimize direct contact with potentially contaminated fluids or surfaces.
- Patient Isolation: Isolation procedures for patients with active CMV infections are crucial to contain the spread. This may involve isolating patients in designated rooms or using other appropriate methods to limit contact with susceptible individuals.
High-Risk Populations
Certain populations are at increased risk of severe CMV complications. Understanding these risk factors is vital for targeted preventative measures.
- Immunocompromised Individuals: Individuals with weakened immune systems, such as transplant recipients, patients with HIV/AIDS, or those undergoing chemotherapy, are particularly vulnerable to CMV infections and their associated complications. Their compromised immune systems make them more susceptible to severe disease.
- Pregnant Women: CMV infection during pregnancy can pose significant risks to the developing fetus. Pregnant women, especially those with a compromised immune system or those exposed to high-risk individuals, should be aware of their risk and take appropriate precautions.
Flowchart: Preventing CMV Transmission in Healthcare
This flowchart illustrates the steps involved in preventing CMV transmission in a healthcare setting. Each step is crucial in minimizing the risk of infection.“`[Diagram: A simple flowchart would depict these steps:
1. Patient Assessment
Screening for CMV risk factors
2. Infection Control Protocols
Implementing standard and transmission-based precautions
3. Personal Protective Equipment (PPE)
Use of appropriate PPE
4. Hand Hygiene
Frequent and thorough handwashing
5. Equipment Management
Dedicated equipment for each patient
6. Waste Management
Proper disposal of contaminated materials
7. Environmental Cleaning
Regular cleaning and disinfection of surfaces
8. Monitoring and Reporting
Ongoing monitoring and reporting of infections]“`
Complications and Long-Term Effects
Cytomegalovirus (CMV) infection, while often asymptomatic, can lead to severe complications, especially in individuals with weakened immune systems. Understanding these potential outcomes is crucial for proactive management and prevention. The long-term effects can vary significantly depending on factors like age, overall health, and the presence of pre-existing conditions.The severity of CMV complications can range from mild discomfort to life-threatening conditions.
Early detection and appropriate medical intervention can significantly improve outcomes and reduce the long-term impact of CMV infection.
Potential Complications of CMV Infection
CMV can cause a variety of complications, particularly in those with compromised immune systems. These complications often manifest as organ damage or dysfunction. Careful monitoring and management are crucial in mitigating the severity of these outcomes.
Long-Term Effects in Different Individuals
The long-term effects of CMV infection vary greatly. Newborn infants infected during pregnancy may experience developmental delays or other neurological issues. In immunocompromised individuals, CMV can lead to chronic organ damage, impacting their quality of life. Individuals with a strong immune response often experience only mild or no long-term effects.
Risk Factors for Developing CMV Complications
Several factors increase the risk of developing complications from CMV infection. Individuals with weakened immune systems, such as those undergoing organ transplantation or battling HIV/AIDS, are at a higher risk. Pregnant women infected with CMV during pregnancy are also at risk of transmitting the virus to their unborn child.
Severity of Complications Across Age Groups
The severity of CMV complications often differs based on age. Infants and young children are more susceptible to serious neurological and developmental problems if infected with CMV. Adults, on the other hand, may experience milder symptoms or no noticeable effects. However, long-term effects in adults, particularly those with weakened immune systems, are also possible.
Signs and Symptoms of CMV Complications
Recognizing the signs and symptoms of CMV complications is vital for prompt medical attention. These can vary depending on the affected organ system. Symptoms may include fever, fatigue, liver problems, and in some cases, neurological symptoms. The presence of these symptoms necessitates immediate medical evaluation.
Summary Table of CMV Complications
| Potential CMV Complications | Associated Risk Factors |
|---|---|
| Congenital CMV Infection | Maternal CMV infection during pregnancy |
| CMV retinitis | Advanced HIV infection, immunosuppression |
| CMV pneumonia | Immunosuppression, organ transplantation |
| CMV enteritis | Immunosuppression, organ transplantation |
| CMV encephalitis | Immunosuppression, severe cases of CMV infection |
| CMV hepatitis | Immunosuppression, severe cases of CMV infection |
| CMV nephropathy | Immunosuppression, severe cases of CMV infection |
CMV in Specific Populations
Cytomegalovirus (CMV) can affect different populations in various ways, highlighting the importance of tailored approaches to diagnosis, treatment, and prevention. Understanding the unique vulnerabilities and challenges faced by specific groups is crucial for optimizing health outcomes. This section delves into the impact of CMV on pregnant women, immunocompromised individuals, children and adolescents, the elderly, and discusses the complexities in managing CMV across these diverse populations.
Impact on Pregnant Women and Fetuses
CMV infection during pregnancy can pose significant risks to the developing fetus. Congenital CMV infection, acquired by the fetus during pregnancy, can lead to a spectrum of complications, ranging from mild to severe. These complications can include hearing loss, vision problems, intellectual disability, and neurological damage. The severity of these outcomes depends on the timing of maternal infection during pregnancy and the extent of viral replication in the fetus.
Early prenatal diagnosis and appropriate management are essential to minimize the risk of congenital CMV infection.
Impact on Immunocompromised Individuals
Immunocompromised individuals, such as those with HIV/AIDS, organ transplant recipients, or those undergoing chemotherapy, are at a significantly higher risk of CMV reactivation or severe CMV disease. Reactivation of latent CMV can lead to life-threatening complications, including retinitis (inflammation of the retina), colitis (inflammation of the colon), and pneumonitis (inflammation of the lungs). Proactive monitoring and prompt treatment are vital for preventing severe disease and maintaining overall health.
CMV in Children and Adolescents
CMV infection in children and adolescents typically presents with mild symptoms, often resembling a common viral illness. However, in some cases, more severe complications can arise, particularly in those with underlying immune deficiencies. Long-term effects of CMV infection in children and adolescents can be subtle, and may not manifest until later in life. Careful monitoring and management are crucial to prevent potential complications.
Considerations for Treating CMV in the Elderly
The elderly population may exhibit unique responses to CMV infection and treatment. Age-related factors, such as decreased immune function and concomitant medical conditions, can influence the severity and management of CMV infection. Treatment regimens for CMV in the elderly may need to be adjusted based on individual factors to minimize adverse effects and maximize effectiveness. The elderly may also be more vulnerable to side effects from antiviral medications used to treat CMV.
Challenges in Managing CMV in Different Populations
Managing CMV in diverse populations presents various challenges. These challenges include the need for tailored diagnostic strategies, the variability in disease presentation, the potential for drug interactions with other medications, and the cost of treatment. Accessibility to healthcare services and the ability to adhere to complex treatment regimens can also be barriers to effective management.
Summary of Specific Considerations for Managing CMV in Different Patient Groups
| Patient Group | Specific Considerations |
|---|---|
| Pregnant Women | Early diagnosis, monitoring for fetal complications, and preventive measures. |
| Immunocompromised Individuals | Proactive monitoring, prompt treatment, and close collaboration with specialists. |
| Children and Adolescents | Careful monitoring for potential complications, and support for long-term health. |
| Elderly | Individualized treatment plans, careful monitoring for adverse effects, and consideration of comorbidities. |
Illustrative Examples
CMV, or cytomegalovirus, often lurks silently, yet its impact can be significant, especially in vulnerable populations. Understanding its diverse manifestations and the challenges in management is crucial for effective prevention and treatment strategies. This section provides case study examples to illustrate CMV’s varied presentations and the complex treatment considerations involved.
A Case Study of Congenital CMV, What is cmv cytomegalovirus
Congenital CMV infection, occurring when a pregnant woman contracts CMV, can lead to a range of complications in the newborn. A newborn may display mild symptoms, such as jaundice, or more severe ones, like neurological problems. The severity of the infection depends on several factors, including the timing of the maternal infection during pregnancy and the immune status of the infant.
For example, an infection acquired early in pregnancy often leads to more severe consequences.
Impact on Different Organ Systems
CMV can affect various organ systems, causing a wide array of symptoms. For instance, in the cardiovascular system, CMV can lead to inflammation and damage of blood vessels. In the nervous system, it can cause encephalitis (brain inflammation) or polyradiculopathy (inflammation of nerve roots). The severity and type of organ system involvement depend on the individual’s immune response and the strain of CMV.
Varied Manifestations in Individuals
CMV infection can manifest differently in different individuals, even within the same population. Some individuals may remain asymptomatic carriers, while others experience mild flu-like symptoms. In immunocompromised individuals, however, CMV can cause severe and life-threatening complications. The variation in presentation is a key factor to consider when evaluating patients. Factors like age, pre-existing health conditions, and immune status all contribute to the clinical picture.
Challenges in Treating CMV Infection in Specific Scenarios
Treating CMV infection in specific scenarios, such as in transplant recipients or those with AIDS, presents unique challenges. The immunosuppressive medications often used to prevent organ rejection or manage AIDS can make patients more susceptible to CMV infections. Treatment must be carefully tailored to address the underlying immune deficiency while minimizing the risk of drug interactions and side effects.
For example, in a patient with a recent bone marrow transplant, the choice of anti-CMV medication must carefully consider the patient’s bone marrow recovery and the potential toxicity of various drugs.
Hypothetical Case Study and Treatment Options
A 28-year-old woman, recently diagnosed with HIV, presents with fatigue, fever, and mild neurological symptoms. Laboratory tests reveal a CMV infection. Treatment options for this patient include antiviral medications, such as ganciclovir or valganciclovir, and possibly other supportive therapies. The specific regimen will depend on the severity of the infection, the patient’s overall health, and the potential for drug interactions with other medications.
Careful monitoring of the patient’s immune response and viral load is critical throughout treatment.
A Patient’s Experience with CMV
“I felt like I had the flu, but it just wouldn’t go away. The fatigue was unbelievable. I couldn’t even get out of bed some days. The doctors ran so many tests, and finally, they found CMV. It was a relief to finally have a diagnosis, but I was also scared of the long-term effects. The treatment was tough, but thankfully, I’m doing better now.”
End of Discussion: What Is Cmv Cytomegalovirus
In conclusion, understanding cytomegalovirus (CMV) is vital for informed decision-making regarding health and well-being. This comprehensive guide offers a detailed exploration of CMV, empowering readers with knowledge about its various aspects, from diagnosis to prevention. By grasping the intricacies of CMV, individuals can better navigate potential health challenges and make informed choices about their health and well-being.