Anxiety stress and diarrhea are often intertwined, with the connection running deeper than many realize. This blog post delves into the physiological mechanisms linking anxiety and stress to digestive issues like diarrhea. We’ll explore the role of the autonomic nervous system, the impact on the gut microbiome, and common symptoms. Understanding this complex interplay is key to effectively managing these challenging issues.
The content will cover the range of symptoms, diagnostic approaches, and effective management strategies, including relaxation techniques, dietary modifications, and the role of medication. We will also examine the impact on daily life and provide actionable strategies for coping. Finally, we will discuss preventative measures and resources for support, emphasizing the importance of professional help.
Understanding the Connection: Anxiety Stress And Diarrhea
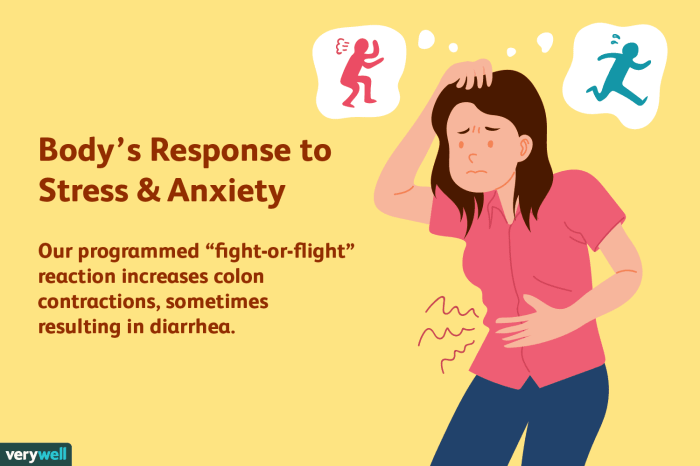
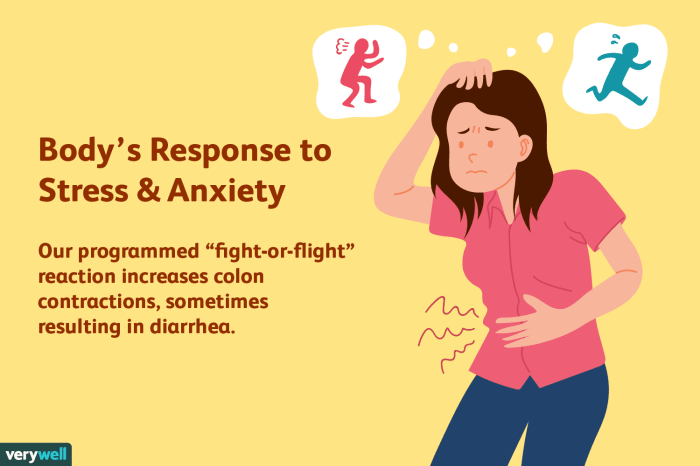
The gut-brain axis, a bidirectional communication system between the central nervous system and the enteric nervous system (the nervous system of the gut), plays a crucial role in mediating the effects of stress and anxiety on digestive health. This intricate connection highlights the profound influence our emotional state has on our physical well-being, particularly regarding gastrointestinal function. Understanding the physiological mechanisms behind this connection can help us develop strategies to manage stress-related digestive issues.The autonomic nervous system, specifically the sympathetic nervous system’s activation during stress, significantly impacts the gut.
This activation triggers a cascade of physiological responses, often leading to the release of stress hormones like cortisol. These hormones can alter gut motility, reducing the time food spends in the digestive tract and increasing the likelihood of diarrhea. Simultaneously, the parasympathetic nervous system, responsible for the “rest and digest” response, is suppressed. This disruption of the delicate balance between these two systems disrupts normal digestive processes, often manifesting as diarrhea.
Physiological Mechanisms
The gut microbiome, a complex community of bacteria, fungi, and other microorganisms residing in the gut, is also profoundly affected by stress. Chronic stress can lead to dysbiosis, an imbalance in the gut microbiome composition. This disruption can affect the production of beneficial metabolites, contributing to digestive issues. Conversely, a healthy gut microbiome can help regulate stress responses.
This reciprocal relationship emphasizes the importance of maintaining a balanced gut microbiome for overall well-being.
Effects on the Gut Microbiome
Anxiety and stress can significantly alter the gut microbiome’s composition and function. This imbalance can affect the production of beneficial metabolites and contribute to inflammation in the gut, making individuals more susceptible to digestive disorders. Research shows that stress can decrease the diversity of the gut microbiome and potentially increase the presence of harmful bacteria, leading to a less efficient digestive process.
The exact mechanisms and long-term consequences of these changes are still under investigation.
Common Stress-Related Digestive Disorders
Common stress-related digestive disorders include irritable bowel syndrome (IBS), functional dyspepsia, and inflammatory bowel disease (IBD). IBS is characterized by abdominal pain, altered bowel habits (including diarrhea), and bloating, often exacerbated by stress. Functional dyspepsia involves persistent upper abdominal discomfort, sometimes accompanied by nausea and bloating, frequently linked to psychological stress. While IBD, encompassing conditions like Crohn’s disease and ulcerative colitis, involves chronic inflammation of the digestive tract, stress can often trigger flare-ups or worsen symptoms.
Prevalence in Different Populations
The prevalence of stress-related digestive issues varies across populations. Studies suggest that individuals experiencing high levels of stress, such as those facing significant life changes or ongoing trauma, are more likely to develop or experience worsened symptoms of these disorders. Moreover, populations facing socioeconomic disparities or experiencing discrimination may also exhibit higher rates of stress-related digestive issues.
Factors Contributing to the Connection
| Factor | Mechanism | Impact |
|---|---|---|
| Stress Hormone Release | Increased cortisol and other stress hormones disrupt the balance of the autonomic nervous system, impacting gut motility and reducing the time food spends in the digestive tract. | Increased risk of diarrhea, abdominal cramps, and other digestive issues. |
| Gut Microbiome Imbalance | Chronic stress can disrupt the balance of beneficial and harmful bacteria in the gut microbiome, leading to inflammation and altered gut function. | Increased susceptibility to digestive disorders, including IBS and IBD. |
| Immune System Response | Stress-induced immune system activation can trigger inflammation in the gut, exacerbating digestive issues. | Inflammation and worsening of existing digestive conditions. |
| Neuroendocrine Pathways | Stress triggers a cascade of neuroendocrine responses, including alterations in neurotransmitters, affecting gut motility and secretion. | Changes in bowel habits and increased sensitivity to digestive stimuli. |
Symptoms and Diagnosis
Anxiety-induced diarrhea, a distressing consequence of anxiety, can significantly impact daily life. Understanding its symptoms and diagnostic process is crucial for effective management. Differentiating it from other forms of diarrhea requires careful evaluation and consideration of various factors.The experience of anxiety-induced diarrhea often involves a complex interplay of physical and emotional responses. Recognizing the range of symptoms and the diagnostic steps involved can empower individuals to seek appropriate medical attention and develop effective coping strategies.
Symptoms Associated with Anxiety-Induced Diarrhea
Anxiety-related diarrhea manifests in a variety of ways, often overlapping with other digestive issues. Common symptoms include frequent bowel movements, ranging from loose stools to watery stools. These symptoms can be accompanied by abdominal cramping, bloating, and feelings of urgency. Emotional distress and anxiety can trigger these symptoms, often exacerbating the digestive discomfort. Some individuals might also experience nausea or vomiting.
Diagnostic Process for Anxiety-Induced Diarrhea
Differentiating anxiety-induced diarrhea from other causes necessitates a thorough evaluation. A detailed medical history, including a review of current medications, recent dietary changes, and stress levels, is essential. Physicians typically begin by ruling out more serious underlying medical conditions such as infections or inflammatory bowel diseases.
Diagnostic Tools for Evaluating Anxiety-Related Diarrhea
Several diagnostic tools are used to evaluate the cause of diarrhea. A physical examination, including checking for signs of infection or inflammation, is often the first step. Stool samples can be analyzed to identify pathogens or other abnormalities. Blood tests can help assess for underlying conditions and inflammatory markers. Furthermore, psychological assessments may be utilized to evaluate the level of anxiety and stress, particularly when other physical causes have been ruled out.
Distinguishing Anxiety-Related Diarrhea from Other Forms of Diarrhea
Accurate diagnosis relies on considering the overall clinical picture. Anxiety-related diarrhea is often episodic, directly linked to stressful situations or anxiety triggers. In contrast, infectious diarrhea tends to have a more sudden onset and is frequently accompanied by fever or other systemic symptoms. Other types of diarrhea, such as those related to food intolerances, might present with specific dietary patterns.
Experiencing anxiety, stress, and subsequent diarrhea can be incredibly frustrating. It’s important to be wary of potential “cures” that promise quick fixes for these issues, especially those that seem too good to be true. Many “miracle” remedies for anxiety-related digestive problems are often signs of medical quackery, and it’s crucial to seek advice from qualified medical professionals instead of falling for unsubstantiated claims.
Be sure to research any treatment options thoroughly and consult reputable sources like a doctor, a registered dietitian, or other qualified healthcare professionals before making any decisions. Learning to identify signs of medical quackery here can help you make informed choices about your health. Ultimately, addressing anxiety and stress-induced diarrhea requires a holistic approach that prioritizes your overall well-being.
Careful attention to the timing, context, and associated symptoms is crucial for differentiation.
Table of Potential Symptoms and Severity
| Symptom | Description | Severity |
|---|---|---|
| Frequent bowel movements | More than three bowel movements per day | Mild to Moderate |
| Watery stools | Stools are loose and watery in consistency | Mild to Moderate |
| Abdominal cramping | Painful contractions in the abdomen | Mild to Moderate |
| Bloating | Feeling of fullness or distension in the abdomen | Mild to Moderate |
| Urgency | Sudden, intense need to defecate | Mild to Moderate |
| Nausea | Feeling of discomfort and possible vomiting | Mild to Moderate |
| Fever | Elevated body temperature | Moderate to Severe (if present) |
| Blood in stool | Visible blood in the stool | Severe (requires immediate medical attention) |
Management and Treatment

Anxiety-related diarrhea can significantly impact daily life, but effective management strategies exist. Understanding the triggers and employing a multifaceted approach, encompassing lifestyle changes, dietary modifications, and potentially medication, can help alleviate symptoms and improve overall well-being. This section explores various techniques for managing this condition.Addressing anxiety-related diarrhea requires a personalized strategy that considers individual needs and preferences. Effective management combines proactive lifestyle adjustments, targeted dietary interventions, and, in some cases, the appropriate use of medication.
It is crucial to work collaboratively with healthcare professionals to develop a comprehensive plan tailored to specific circumstances.
Strategies for Managing Anxiety-Related Diarrhea
Effective management of anxiety-related diarrhea involves a multi-pronged approach that tackles the underlying anxiety and addresses the digestive symptoms. This proactive approach involves lifestyle changes, dietary modifications, relaxation techniques, and, in certain cases, medication.
- Relaxation Techniques: Mindfulness and deep breathing exercises can be highly effective in reducing stress and calming the nervous system. These techniques promote a sense of calm and relaxation, thereby mitigating the physiological responses that can trigger diarrhea. Examples include progressive muscle relaxation, guided imagery, and yoga. These techniques can help regulate the body’s response to stress and reduce the likelihood of anxiety-induced digestive issues.
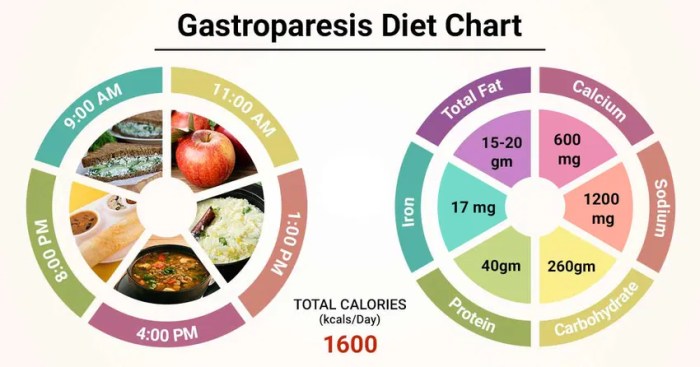
- Dietary Modifications: A diet rich in fiber can promote regularity, but certain foods may exacerbate symptoms. Identifying trigger foods through a food diary and gradually eliminating potential irritants is crucial. Examples of foods that can trigger symptoms include spicy foods, caffeine, alcohol, and processed foods. A balanced diet that emphasizes whole grains, fruits, and vegetables can often reduce symptoms.
A registered dietitian can provide personalized dietary recommendations.
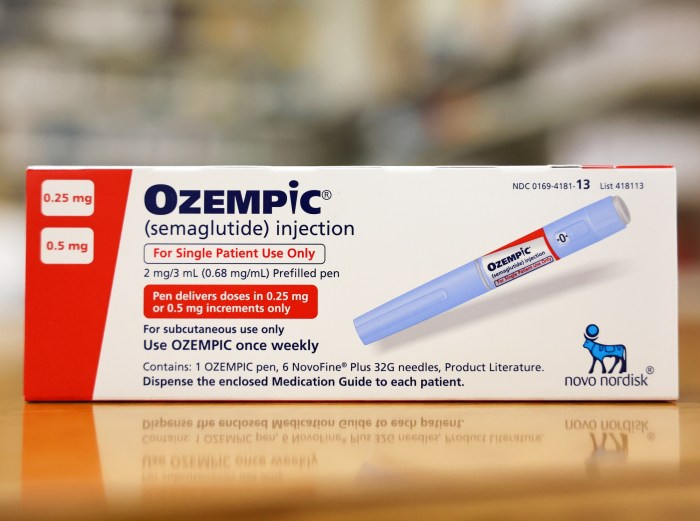
- Medication: In some cases, medication may be necessary to manage anxiety and its associated symptoms. Selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed for anxiety disorders. These medications can impact gut motility and potentially alleviate diarrhea. However, this is an aspect that must be discussed with a physician. The specific medication and dosage will depend on individual needs and should be determined in consultation with a healthcare professional.
Role of Medication in Treating Anxiety and its Impact on Diarrhea
Medication plays a vital role in managing anxiety and its associated symptoms, including diarrhea. However, medication should only be considered after consulting with a healthcare professional to ensure it’s the right approach. The specific medication and dosage will vary depending on individual needs.
The impact of medication on diarrhea is complex. Some medications, particularly those used to treat anxiety, can influence gut motility. SSRIs, for example, are often prescribed for anxiety disorders but can sometimes affect bowel function. This impact can either exacerbate or alleviate diarrhea, depending on the individual. Therefore, careful monitoring and adjustment of medication dosage under a doctor’s supervision is crucial to optimize treatment effectiveness and minimize side effects.
Flowchart for Managing Anxiety-Related Diarrhea

The flowchart illustrates a potential approach to managing anxiety-related diarrhea. It emphasizes the importance of a stepwise approach, involving initial self-assessment, consultation with healthcare professionals, and implementing tailored management strategies. This step-by-step approach allows for the most effective management and treatment of the condition.
Ugh, anxiety, stress, and the dreaded diarrhea… it’s a rough combo. I’ve been researching ways to manage the gut issues that often accompany these feelings, and magnesium l-threonate seems promising. Finding the right magnesium l threonate dosage is key, as too much or too little can be problematic. Hopefully, this supplement can help calm my digestive system and ease the anxiety stress cycle.
I’m keeping my fingers crossed!
Importance of Professional Help
Seeking professional help is crucial for effective management of anxiety-related diarrhea. A healthcare professional can conduct a comprehensive evaluation, identify underlying causes, and develop a personalized treatment plan. This personalized plan may include relaxation techniques, dietary modifications, and, if necessary, medication. This ensures that the treatment plan is tailored to the specific needs of the individual.
Impact on Daily Life
Anxiety-related diarrhea can significantly disrupt daily life, impacting routines, relationships, and overall well-being. This chronic digestive issue, often triggered or exacerbated by anxiety, can range from mild discomfort to debilitating episodes, making it challenging to maintain a normal lifestyle. The emotional toll can be profound, leading to feelings of isolation and frustration.The constant fear of needing to rush to the bathroom, the embarrassment of public bathroom situations, and the physical discomfort can create a cycle of avoidance and anxiety.
This can affect various aspects of daily life, from work performance to social interactions and personal activities. Understanding the impact of this condition is crucial for developing effective coping strategies and seeking appropriate support.
Impact on Routines and Activities
Anxiety-related diarrhea can severely disrupt daily routines, making it difficult to engage in planned activities or maintain a sense of normalcy. The unpredictable nature of the condition often leads to avoidance of social gatherings, travel, or even simple outings. Individuals may feel restricted in their choices, limiting their ability to participate in activities they once enjoyed. For instance, a person might avoid restaurants or large gatherings due to the fear of needing to use a restroom.
Ugh, anxiety, stress, and diarrhea – a terrible trio! It’s all so interconnected, isn’t it? While dealing with these digestive issues, it’s also important to consider your overall health and how to maintain strong bones. A healthy diet and lifestyle, including weight-bearing exercise, can significantly reduce your risk of osteoporosis, a condition where bones become weak and fragile.
Checking out how to prevent osteoporosis can give you some great ideas. Luckily, focusing on stress management and healthy eating habits can help alleviate these uncomfortable digestive symptoms too. It’s a whole-body approach!
This avoidance can further exacerbate anxiety and contribute to a cycle of social isolation.
Social and Emotional Consequences
The social and emotional consequences of anxiety-related diarrhea can be substantial. Embarrassment and fear of public restrooms can lead to social withdrawal, impacting friendships and relationships. The constant worry about the next episode can lead to feelings of isolation and shame. People may struggle to maintain close relationships due to the unpredictable nature of their condition. They may also experience reduced self-esteem and confidence.
This can lead to a downward spiral of anxiety and depression.
Impact on Relationships and Work Performance, Anxiety stress and diarrhea
Anxiety-related diarrhea can strain relationships, both personal and professional. Frequent bathroom trips and the need for accommodations can be disruptive to partners, family members, and colleagues. Missed appointments, deadlines, or work meetings due to diarrhea episodes can negatively impact work performance and career prospects. Relationships may suffer from a lack of understanding and support. Work performance can be affected by the anxiety associated with the condition and the need to manage the symptoms.
For example, an employee might experience decreased productivity due to frequent bathroom breaks and the stress of worrying about diarrhea episodes.
Coping Strategies
Effective coping strategies are essential for managing the impact of anxiety-related diarrhea on daily life. These strategies should focus on both physical and emotional well-being. The following strategies may help:
- Regular Exercise: Regular physical activity can help reduce stress and improve digestion.
- Stress Reduction Techniques: Mindfulness, meditation, yoga, or deep breathing exercises can help manage anxiety and improve overall well-being.
- Dietary Modifications: Identifying and avoiding trigger foods can help minimize the frequency and severity of episodes.
- Maintaining a Healthy Diet: A balanced diet with adequate fiber can help regulate bowel movements.
- Seeking Professional Support: Consulting a therapist or counselor can help address the underlying anxiety and develop coping mechanisms.
- Communicating with Loved Ones: Open communication with partners, family members, and colleagues can help them understand and support the individual’s needs.
- Utilizing Support Groups: Support groups can provide a safe space to share experiences and learn from others facing similar challenges.
Real-Life Stories/Case Studies
(Space for hypothetical case studies/stories, illustrating impact on daily life)Many individuals struggle with the invisible burden of anxiety-related diarrhea. It’s a condition that can profoundly impact every aspect of daily life, from simple social interactions to career aspirations. Developing effective coping strategies and seeking appropriate support are crucial for managing the challenges and improving quality of life.
Prevention and Support
Anxiety-related diarrhea can significantly impact daily life, but proactive steps and supportive environments can make a substantial difference. Understanding the triggers and fostering a supportive network are crucial for managing this condition effectively. This section explores strategies for preventing or minimizing symptoms and building a strong support system.
Factors Contributing to Anxiety-Related Diarrhea
Several factors can contribute to the development of anxiety-related diarrhea. These factors often involve the interplay between psychological stress and the body’s physiological responses. Common triggers include stressful life events, such as job loss, relationship problems, or major life transitions. Additionally, chronic anxiety, social anxiety, and performance anxiety can all contribute to the development of this condition.
The anticipation of stressful events can also be a significant trigger. For example, a student experiencing anxiety about an upcoming exam may experience diarrhea in the days leading up to the exam.
Proactive Steps for Prevention
Implementing proactive strategies can help prevent or minimize the symptoms of anxiety-related diarrhea. These strategies aim to reduce stress and improve overall well-being. Practicing relaxation techniques, such as deep breathing exercises, progressive muscle relaxation, or mindfulness meditation, can effectively manage anxiety and its physiological effects. Regular exercise, a balanced diet, and sufficient sleep are also vital components of a preventative approach.
Adequate hydration is also essential, as dehydration can worsen the symptoms of diarrhea.
Supportive Environments
Creating supportive environments is critical for managing anxiety-related diarrhea. A supportive environment includes individuals who understand the condition and provide encouragement and understanding. Family members, friends, and partners can play a significant role in creating a supportive atmosphere. Open communication about the condition and its impact can help to reduce feelings of isolation and shame. This can help individuals feel more comfortable discussing their experiences and seeking help when needed.
For example, a supportive partner might help create a calming atmosphere at home during periods of high stress.
Professional Support and Resources
Seeking professional support is crucial for effectively managing anxiety-related diarrhea. A therapist or counselor can help identify underlying anxieties and develop coping mechanisms. A gastroenterologist can assess the physical aspects of the condition and rule out other medical causes. These professionals can provide guidance and support tailored to individual needs. Furthermore, exploring available resources like support groups and online communities can offer valuable peer-to-peer support.
Support Groups and Online Communities
Support groups or online communities provide a platform for individuals experiencing anxiety-related diarrhea to connect with others who understand their struggles. Sharing experiences and coping strategies can be empowering and offer a sense of belonging. These communities can also provide valuable information and advice from those who have firsthand experience with the condition. For instance, online forums dedicated to anxiety-related digestive issues can offer a space for individuals to ask questions, share their experiences, and connect with others facing similar challenges.
Resources for Anxiety-Related Diarrhea
| Resource | Description | Contact Information |
|---|---|---|
| Anxiety and Depression Association of America (ADAA) | Provides information and resources on anxiety disorders, including coping mechanisms and support groups. | 1-800-950-NAMI (6264) |
| National Institute of Mental Health (NIMH) | Offers information and research on mental health conditions, including anxiety disorders. | (301) 443-4513 |
| The Mayo Clinic | Provides comprehensive information on various medical conditions, including anxiety-related disorders and digestive issues. | 1-800-662-5643 |
| The American College of Gastroenterology | Offers information on digestive health, including potential connections between anxiety and digestive symptoms. | (214) 638-0500 |
Final Wrap-Up
In conclusion, anxiety stress and diarrhea are not isolated issues. They are interconnected problems with significant impacts on daily life. Understanding the physiological mechanisms, recognizing the symptoms, and adopting effective management strategies are crucial for navigating these challenges. Seeking professional help is vital for developing personalized solutions. By understanding the factors contributing to this connection and employing effective coping mechanisms, individuals can actively manage their symptoms and improve their quality of life.