How to stick to new year resolutions is a common struggle, but it doesn’t have to be a lost cause. This guide dives deep into the psychology behind resolutions, providing practical strategies to set realistic goals, build lasting habits, and overcome inevitable challenges. We’ll explore everything from understanding the common pitfalls to maintaining motivation throughout the year, equipping you with the tools to achieve your goals and transform your life.
We’ll examine the different types of resolutions, from fitness and finance to relationships and personal growth. Understanding the psychology behind why resolutions often falter is key, and we’ll offer insights into setting effective goals and building sustainable habits. Learn how to break down daunting tasks into manageable steps and leverage the power of self-monitoring. Plus, we’ll discuss the crucial role of support systems and rewards in keeping you motivated.
Understanding Resolutions

New Year’s resolutions are a popular tradition, but often a source of frustration. Many people embark on ambitious plans, only to fall short of their goals. Understanding the reasons behind this common experience can pave the way for more sustainable change. This section delves into the intricacies of setting resolutions, exploring the psychological factors that hinder success and emphasizing the importance of realistic expectations.A common misconception is that resolutions are solely about willpower.
In reality, a combination of psychological factors and practical planning contributes to both success and failure. Setting achievable goals and understanding the potential pitfalls is crucial for long-term commitment.
Common New Year’s Resolutions, How to stick to new year resolutions
Understanding the common themes behind resolutions can help identify areas where people often struggle. This insight can be valuable in tailoring strategies for achieving personal goals.
- Health: Weight loss, exercise, eating healthier, quitting smoking, getting more sleep.
- Finances: Saving money, paying off debt, budgeting, investing, improving credit score.
- Relationships: Spending more quality time with family, improving communication with partners, resolving conflicts, building stronger relationships with friends.
- Personal Growth: Learning a new skill, reading more books, volunteering, taking a course, improving time management.
- Productivity: Completing projects, organizing tasks, managing time effectively, working on personal goals.
Psychological Factors Hindering Resolution Maintenance
Several psychological factors contribute to the common struggle of maintaining resolutions. These factors include unrealistic expectations, lack of specific plans, and insufficient support systems.
- Unrealistic Expectations: Many resolutions are overly ambitious and difficult to maintain. Setting smaller, incremental goals that build upon each other is often more effective than aiming for drastic change overnight.
- Lack of Specific Plans: Vague resolutions are hard to track and measure. Creating detailed action plans, outlining steps and timelines, increases the likelihood of success. This includes considering potential obstacles and developing contingency plans.
- Insufficient Support Systems: Individuals struggling with resolutions may benefit from support networks like friends, family, or support groups. Encouragement and accountability can play a vital role in maintaining motivation.
- Perfectionism: Striving for flawlessness can lead to discouragement if initial attempts don’t meet unrealistic standards. It’s important to view setbacks as learning opportunities and to focus on progress rather than perfection.
- Lack of Intrinsic Motivation: Resolutions based solely on external pressures (e.g., social expectations) are often less sustainable. Focusing on intrinsic motivation, aligning goals with personal values and aspirations, fosters a deeper commitment.
Importance of Realistic Expectations
Setting resolutions requires careful consideration of personal capabilities and resources. Realistic expectations are essential for sustainable progress and avoiding feelings of failure or frustration.
Sticking to New Year’s resolutions can be tough, but consistency is key. One way to stay on track is to break down big goals into smaller, manageable steps. And while we’re on the topic of achieving goals, have you ever wondered if using toothpaste on pimples really works? The science behind that is surprisingly interesting to explore, and if you’re curious, check out this article to learn more: does using toothpaste on pimples really work.
Ultimately, finding a routine that works for you, whether it’s tackling a complex goal or treating a breakout, requires understanding what works best for your individual needs. That’s the secret to success, no matter what you set your mind to.
“Setting smaller, achievable goals that build upon each other is often more effective than aiming for drastic change overnight.”
Failure to recognize personal limitations can lead to feelings of inadequacy. Prioritizing self-compassion and understanding that setbacks are normal can foster a more supportive approach to achieving goals.
Short-Term vs. Long-Term Resolutions
A comparison of short-term and long-term resolutions highlights the distinct challenges and benefits associated with each.
| Feature | Short-Term Resolutions | Long-Term Resolutions |
|---|---|---|
| Definition | Goals achievable within a few weeks or months. | Goals requiring several months or years to achieve. |
| Challenges | Maintaining momentum over extended periods. | Sustaining motivation and preventing burnout. |
| Benefits | Quick wins and early progress. | Significant long-term impact. |
| Examples | Losing 5 pounds, reading a book per week, exercising 3 times per week. | Saving for a house, improving financial literacy, mastering a musical instrument. |
| Strategies | Breaking down goals into smaller, daily tasks. | Establishing a clear vision and breaking it into manageable milestones. |
Setting Effective Goals

Resolutions often fall flat because the goals are too broad or lack a clear path to achievement. Turning aspirations into tangible results requires a strategic approach. This involves breaking down ambitious targets into smaller, actionable steps, and using specific, measurable criteria to track progress. This structured approach significantly boosts the likelihood of success.Effective goal setting is the cornerstone of successful resolution keeping.
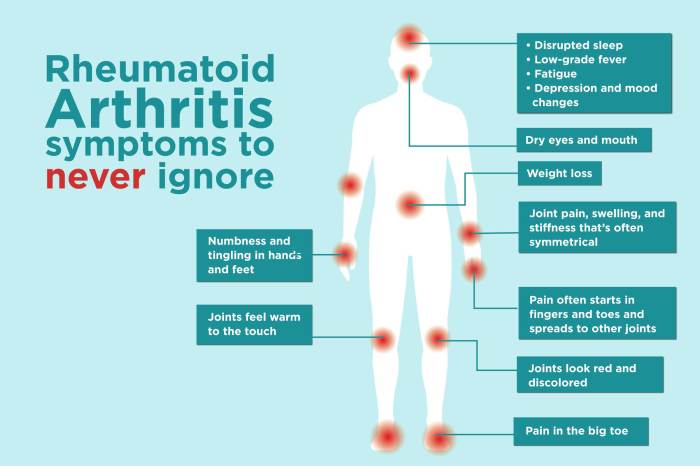
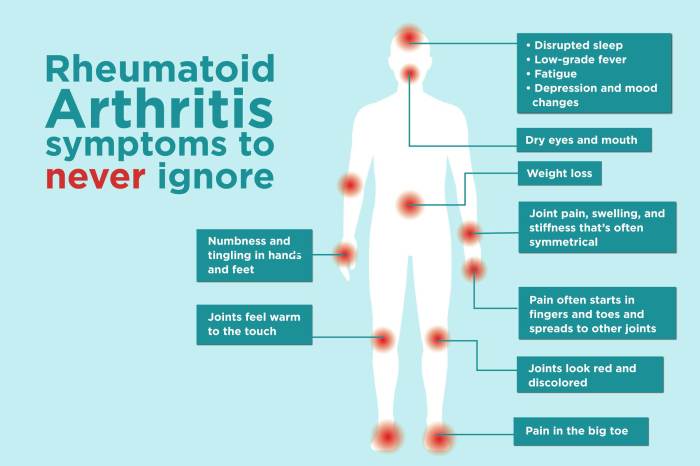
Keeping those New Year’s resolutions feels tough, right? It’s all about consistency and understanding your body’s signals. For example, chronic inflammation can manifest in surprising ways, like fatigue or skin rashes. Learning to recognize these 11 atypical signs of chronic inflammation here can help you address potential underlying issues impacting your ability to stick to your goals.
Ultimately, prioritizing self-awareness and making sustainable lifestyle changes, like incorporating healthy habits, is key to achieving those resolutions.
It’s not just about what you want to achieve, but how you plan to achieve it. A well-defined strategy, with measurable milestones, significantly increases your chances of reaching your desired outcomes.
Breaking Down Large Resolutions
Defining large resolutions into smaller, manageable steps is crucial for sustained motivation and progress. This process transforms overwhelming tasks into a series of achievable actions. This approach prevents feeling overwhelmed, fostering a sense of accomplishment as each step is completed. This ultimately contributes to maintaining motivation and achieving the overall goal.
- Divide and Conquer: Break down the resolution into smaller, more manageable tasks. For example, instead of “Lose 20 pounds,” consider “Lose 1 pound per week” or “Exercise for 30 minutes, 3 times a week.”
- Timeline Implementation: Create a realistic timeline for each step. This creates a clear picture of the progress needed and helps in maintaining focus.
- Prioritization: Determine which tasks are most critical to the overall resolution. Prioritizing tasks helps to focus energy and time effectively.
SMART Goals
SMART goals are specific, measurable, achievable, relevant, and time-bound. They provide a framework for creating resolutions that are attainable and well-defined. This framework enables effective progress monitoring and provides clear direction.
- Specific: Instead of “Get healthier,” a SMART goal might be “Exercise for 30 minutes three times a week, focusing on cardio and strength training.”
- Measurable: “Reduce sugar intake by 50% over the next month.” This is measurable because the reduction is quantified.
- Achievable: “Learn a new language” is less achievable than “Learn 10 new vocabulary words and 5 basic phrases each week.”
- Relevant: “Save $1,000 for a down payment” is relevant to the goal of homeownership.
- Time-bound: “Read a book a week” is vague. “Read one chapter of a book every day for the next month” is time-bound and more effective.
Self-Monitoring and Tracking Progress
Regularly monitoring progress is essential for staying motivated and adjusting strategies as needed. Tracking progress can be done through a variety of methods, such as journaling, using apps, or simply keeping a log. This proactive approach allows for course correction, keeping you on track and maintaining motivation.
- Establish Checkpoints: Set regular checkpoints to review progress and make adjustments if necessary. This ensures that the resolution remains relevant and achievable.
- Use Visual Aids: Visual aids like charts or graphs can help visualize progress and maintain motivation. This creates a clear picture of the journey and reinforces the accomplishment.
- Reflection and Evaluation: Regularly reflect on progress, challenges encountered, and strategies employed. This allows for self-assessment and the adjustment of approaches as needed.
Goal-Setting Techniques by Personality
Different personalities respond well to different goal-setting techniques. Understanding your personality type can lead to more effective strategies for achieving resolutions.
| Personality Type | Goal-Setting Technique | Suitability |
|---|---|---|
| Highly Organized | Detailed action plans, timelines, and checklists | Excellent |
| Creative | Brainstorming, visualization, and flexible timelines | Good |
| Impulsive | Small, immediate rewards for progress, visual reminders | Good |
| Introspective | Journaling, self-reflection, and personal goal setting | Excellent |
Building Habits: How To Stick To New Year Resolutions
Turning resolutions into lasting habits requires more than just good intentions. It’s about understanding the process of habit formation and strategically implementing methods that support your goals. This involves identifying the specific behaviors you want to cultivate and understanding the underlying mechanisms that drive consistent action. The key lies in making these new habits feel natural and integrated into your daily life.The journey to establishing new habits is often a process of trial and error.
There’s no one-size-fits-all solution, but understanding different approaches can help you find what works best for you. A critical aspect of habit formation is recognizing that consistency and routine play a pivotal role in solidifying these new behaviors. This section explores various techniques for building lasting habits, highlighting the importance of consistency and outlining potential obstacles along the way.
Habit-Building Methods
Different approaches to habit formation exist, each with its own strengths and weaknesses. Understanding these methods allows you to tailor your strategy to your personality and lifestyle. Some popular methods include the 21-day rule and habit stacking.
- The 21-Day Rule: This widely discussed method suggests that it takes 21 days to form a new habit. While the exact timeframe is debatable, the principle behind it is sound. It emphasizes consistent effort for a period of time, allowing the behavior to become ingrained. However, success depends on the individual and the complexity of the habit.
Maintaining the habit after the initial period is crucial for long-term success.
- Habit Stacking: This technique involves linking a new habit to an existing one. For instance, if you want to read more, you might make it a habit to read for 15 minutes after you brush your teeth. This method leverages the power of existing routines to make the new habit more automatic and less disruptive to your daily schedule.
It’s adaptable and allows for integration with existing routines, making it a potentially effective approach.
Consistency and Routine
The importance of consistency in habit formation cannot be overstated. Regularity and predictability are key to embedding a new behavior into your daily life. A structured routine provides a framework for incorporating the habit seamlessly. This structured approach reduces the cognitive load associated with remembering to perform the new behavior. A daily routine can significantly contribute to the success of establishing and maintaining new habits.
Obstacles to Habit Formation and Solutions
Habits are not formed without potential obstacles. Recognizing these challenges and having strategies to overcome them is vital for long-term success.
| Obstacle | Solution |
|---|---|
| Lack of Motivation | Identify the underlying reasons for the lack of motivation. Are you facing burnout? Are you losing interest? Addressing the root cause is key. Set realistic goals, reward yourself for progress, and focus on the positive outcomes of establishing the habit. |
| Lack of Time | Break down the habit into smaller, more manageable chunks. Even 5-10 minutes dedicated to the habit can make a difference. Schedule specific times for the habit in your calendar to ensure consistency. |
| Distractions | Create a dedicated space for the habit or routine. Turn off notifications and minimize interruptions during the allocated time. If possible, schedule the habit during times when you are less likely to be interrupted. |
| Negative Self-Talk | Replace negative self-talk with positive affirmations. Focus on your progress and celebrate small victories. Consider seeking support from a friend or family member. |
Overcoming Challenges
New Year’s resolutions often fall by the wayside. We’re all familiar with the initial burst of motivation, followed by the inevitable dips and plateaus. Understanding the common hurdles and developing strategies to overcome them is crucial for long-term success. This section dives into the obstacles that frequently derail our best-laid plans and provides practical tools for navigating those challenges.
Common Pitfalls
Many factors contribute to the failure of resolutions. Procrastination, a tendency to put things off until tomorrow, is a significant obstacle. Lack of motivation, the waning enthusiasm over time, often leads to abandoning a resolution. Unrealistic goals, often set too high or lacking specific action steps, can also be a major source of frustration and discouragement. Furthermore, a lack of a structured plan, leading to a feeling of being overwhelmed, is a common reason for giving up.
Sticking to New Year’s resolutions can feel like climbing a mountain, but breaking down the goal into smaller, achievable steps is key. Just like how understanding the complexities of mental health conditions like dissociative disorder requires professional help, remembering to prioritize self-care and consistency is crucial. For instance, instead of aiming for a complete overhaul, focus on one small change at a time.
This approach, similar to the strategies used in how to treat dissociative disorder , emphasizes gradual progress. Ultimately, celebrating small victories along the way is vital for maintaining motivation and ensuring long-term success with your resolutions.
Finally, external factors like unexpected life changes or stress can derail even the most well-intentioned resolutions.
Strategies for Overcoming Pitfalls
Strategies for overcoming these obstacles should be tailored to the individual. Setting realistic goals is paramount. Breaking down large goals into smaller, manageable steps is a crucial strategy. Each step provides a sense of accomplishment, fueling motivation and preventing feelings of being overwhelmed. Prioritizing tasks and creating a schedule that incorporates the new habits can further enhance the likelihood of success.
Employing time management techniques, like the Pomodoro Technique, can help maintain focus and prevent procrastination.
The Role of Support Systems
Strong support systems are invaluable for staying on track with resolutions. Friends, family, and even support groups provide encouragement, accountability, and a sense of community. They can offer emotional support during challenging times and help you stay motivated when your enthusiasm wanes. Sharing your goals with trusted individuals can foster a sense of responsibility and make you more likely to follow through.
This social support is a critical component of long-term success.
Maintaining Motivation
| Strategy | Description | Example |
|---|---|---|
| Positive Reinforcement | Rewarding yourself for progress, no matter how small. | Treating yourself to a favorite activity after achieving a milestone. |
| Visual Reminders | Using visual cues to reinforce habits. | Placing motivational posters or sticky notes in visible areas. |
| Tracking Progress | Monitoring your progress through a journal or app. | Using a fitness tracker to record workouts or a habit tracker to record daily actions. |
| Accountability Partner | Sharing your goals with someone who can provide support and encouragement. | Having a friend who will check in with you regularly to ensure you’re staying on track. |
| Celebrating Milestones | Acknowledging and rewarding your achievements. | Scheduling a special treat or activity to celebrate reaching a goal. |
“Small, consistent steps add up to significant progress over time.”
Maintaining Motivation
Staying motivated throughout the year is crucial for achieving New Year’s resolutions. The initial enthusiasm often fades, and maintaining consistent effort requires proactive strategies. Understanding the psychological factors behind motivation loss and implementing effective techniques can help you stay on track and achieve your goals. This section delves into strategies for sustaining motivation, incorporating rewards, adjusting to changing circumstances, and embracing self-compassion.Motivation is not a constant; it fluctuates based on various internal and external factors.
Recognizing this natural ebb and flow is the first step towards maintaining a sustainable approach to achieving your resolutions. It’s about understanding that dips in motivation are normal and implementing strategies to navigate those moments effectively.
Strategies for Sustaining Motivation
Maintaining motivation involves recognizing the importance of consistent effort and proactively managing potential obstacles. A key element is creating a supportive environment that fosters a sense of accomplishment.
- Regular Check-ins: Scheduling regular check-ins with yourself or a accountability partner allows for progress tracking and adjustments to your approach. This helps to stay on schedule and prevents feelings of being overwhelmed. For example, if you’re aiming to read a book a month, set a weekly review to monitor your progress and make necessary adjustments to the reading schedule.
- Visual Reminders: Visual cues, like a chart or a motivational poster, can serve as constant reminders of your goals and encourage you to stay on track. This visual reinforcement can be particularly helpful when motivation wanes.
- Breaking Down Large Goals: Dividing large, complex goals into smaller, more manageable tasks makes the process less daunting and provides a sense of accomplishment as you complete each step. This approach fosters a positive feedback loop that sustains motivation.
The Role of Rewards and Positive Reinforcement
Positive reinforcement plays a significant role in maintaining motivation. Rewards, both tangible and intangible, act as incentives and reinforce desired behaviors. They should be aligned with your values and goals, and carefully considered to avoid creating dependency or undue pressure.
- Setting Up a Reward System: A well-structured reward system can significantly boost motivation. Reward yourself for achieving milestones, celebrating progress, and maintaining consistency. For example, if you’re trying to eat healthier, reward yourself with a new cookbook after reaching a specific number of healthy meals.
- Recognizing Small Wins: Celebrating small victories along the way is crucial. This reinforces the positive behaviors and keeps the momentum going. Acknowledging and appreciating your efforts, no matter how small, is essential to maintain enthusiasm and self-belief.
Adjusting Resolutions as Circumstances Change
Life circumstances inevitably change, requiring flexibility in your approach to resolutions. Adaptability is a key factor in achieving long-term success.
- Flexibility and Adaptability: Life throws curveballs, and resolutions need to be adjusted to accommodate these changes. Being adaptable and flexible in your approach allows you to stay on track even when faced with unexpected obstacles. For instance, if your workout routine needs to be adjusted due to an injury, you can adapt by using alternative exercises.
- Re-evaluation and Re-prioritization: Regularly evaluate your progress and prioritize tasks based on current circumstances. If a resolution no longer aligns with your needs or priorities, re-evaluate and re-prioritize your goals to maintain focus and avoid frustration. This allows for a realistic and sustainable approach.
The Importance of Self-Compassion and Flexibility
Self-compassion is essential for navigating setbacks and maintaining a positive mindset. Approaching resolutions with flexibility and self-acceptance fosters a sustainable approach.
- Avoiding Perfectionism: Perfectionism often leads to disappointment and demotivation. Recognize that setbacks are a natural part of the process and practice self-compassion in handling these moments. Focus on learning from mistakes rather than dwelling on them.
- Maintaining a Positive Mindset: Cultivating a positive and supportive inner dialogue is essential. Be kind to yourself, and celebrate your progress, no matter how small. This mindset fosters motivation and helps you navigate challenges with resilience.
Addressing Setbacks
New Year’s resolutions often face setbacks. These are inevitable parts of the journey towards achieving a goal. Understanding how to navigate these hurdles is crucial for maintaining motivation and ultimately reaching your desired outcome. Instead of viewing setbacks as failures, they can be transformed into valuable learning experiences. This section will equip you with strategies to cope with setbacks, reframe them positively, and rebuild momentum.It’s important to recognize that setbacks are not personal failings, but rather natural occurrences in any significant change process.
These moments of temporary detours provide opportunities for adjustment and refinement of your approach. The key lies in recognizing them, adapting to them, and using them as stepping stones towards success.
Coping with Setbacks and Relapses
Dealing with setbacks requires a flexible mindset and a willingness to adjust strategies. It’s crucial to avoid feeling discouraged or defeated when you stumble. Instead, view setbacks as opportunities to learn and improve your approach. Relapses, too, are part of the process. They don’t mean you’ve failed entirely; they simply indicate that you need to make adjustments.
Reframing Setbacks as Learning Opportunities
Instead of dwelling on the negative aspects of a setback, actively seek out the lessons it can teach you. Ask yourself: What went wrong? What could I have done differently? What can I learn from this experience to improve my approach in the future? By focusing on the learning aspect, you transform a potential obstacle into a valuable step in your personal growth.
Techniques for Rebuilding Momentum After a Setback
Rebuilding momentum after a setback requires a proactive approach. First, acknowledge the setback without judgment. Then, analyze what caused it. Identify the specific action or pattern that led to the setback and develop a strategy to address it. Break down large goals into smaller, achievable steps.
Focus on progress, not perfection. Celebrate small wins along the way. Finally, seek support from friends, family, or a mentor if needed. Remember that support can be a vital component in your recovery.
Comparing Approaches to Dealing with Setbacks
| Approach | Description | Potential Effectiveness | Example |
|---|---|---|---|
| Acceptance and Reflection | Acknowledge the setback without judgment and analyze the underlying causes. | High. Provides a clear understanding of the issue. | Recognizing that a busy schedule contributed to missing a workout and adjusting the schedule to incorporate exercise. |
| Adaptability and Adjustment | Adjust your strategy or goal based on the lessons learned from the setback. | High. Improves future chances of success. | Realizing that a strict diet plan wasn’t sustainable and switching to a more flexible, balanced approach. |
| Seeking Support | Leaning on friends, family, or a mentor for guidance and encouragement. | Moderate to High. Provides external perspective and motivation. | Joining a support group for weight loss or connecting with a fitness coach. |
| Positive Reinforcement | Focus on past successes and celebrate small wins to maintain motivation. | High. Keeps motivation high during setbacks. | Remembering previous fitness achievements and acknowledging progress even if the current goal is not met. |
Resolution Examples
Successfully maintaining a New Year’s resolution hinges on more than just good intentions. It demands a clear understanding of the challenges, a robust plan, and a willingness to adapt. Examining successful examples can illuminate the path to achieving personal goals and provide inspiration for overcoming obstacles.
Fitness Resolution Success
Physical fitness resolutions are among the most common, but often the most challenging to sustain. Consistency is key, and this requires a multifaceted approach that integrates exercise, nutrition, and mental well-being.
| Resolution | Steps Taken | Challenges Faced | Solutions Used |
|---|---|---|---|
| Achieve a 30-minute daily jog | Started with 10-minute jogs, gradually increasing duration. Created a jogging schedule, integrated it into the daily routine, and used a fitness tracker to monitor progress. | Lack of motivation on some days, bad weather, and fatigue. | Set small, achievable goals, listened to podcasts or music while jogging, adjusted the schedule based on weather and fatigue, and sought support from a friend. |
| Lose 15 pounds | Developed a balanced meal plan with reduced calorie intake and increased protein. Integrated regular workouts, including cardio and strength training. Used a food tracking app to monitor calorie consumption and macronutrient intake. | Cravings, lack of time, social events with unhealthy food options. | Prepared healthy meals in advance, stocked healthy snacks, identified healthy alternatives to cravings, and made adjustments to the meal plan for social occasions. |
Learning a New Skill
Learning a new skill, like coding or a musical instrument, requires patience and dedication. A structured approach, combined with consistent practice, is essential for success.
| Resolution | Steps Taken | Challenges Faced | Solutions Used |
|---|---|---|---|
| Learn basic Python coding | Followed online tutorials, practiced coding daily, solved coding challenges, and worked on small projects. | Difficulty understanding complex concepts, frustration with errors, lack of immediate results. | Used online forums for support and help, focused on understanding fundamental concepts before moving to complex topics, and broke down the learning process into manageable steps. |
| Master guitar chords | Took guitar lessons, practiced chords regularly, and actively listened to songs to identify chord patterns. | Difficulty memorizing finger positions, lack of immediate improvement, frustration with slow progress. | Used finger exercises to improve dexterity, focused on one chord at a time, and practiced regularly to develop muscle memory. |
Financial Improvement
Improving financial health requires disciplined saving and spending habits. Tracking expenses and setting realistic goals are critical for long-term success.
| Resolution | Steps Taken | Challenges Faced | Solutions Used |
|---|---|---|---|
| Reduce credit card debt | Created a detailed budget, tracked spending meticulously, and prioritized debt repayment. | Unexpected expenses, temptation to spend on non-essential items, and feelings of financial pressure. | Built an emergency fund, identified and eliminated unnecessary expenses, and sought support from a financial advisor. |
| Save $5000 for a down payment | Created a savings plan, tracked monthly savings, and identified ways to increase income. | Maintaining discipline during unexpected financial situations, and lack of motivation. | Set small savings goals, used automated transfers to savings accounts, and rewarded themselves for meeting milestones. |
External Resources
Beyond personal strategies, leveraging external resources can significantly bolster your journey toward achieving New Year’s resolutions. These resources provide diverse perspectives, support, and accountability, crucial for sustained motivation and success. Connecting with others facing similar challenges can be particularly helpful in navigating setbacks and maintaining momentum.
Reputable Resources
Various platforms and materials offer valuable support for achieving personal goals. This includes websites, books, and applications that provide structured guidance, encouragement, and practical tools.
- Websites: Many websites offer free resources and support for goal setting and habit formation. Websites like the Mayo Clinic, Harvard Health Publishing, and Psychology Today provide credible information on various topics related to well-being and self-improvement.
- Books: Books offer in-depth explorations of specific topics, like habit formation, mindfulness, or time management. “Atomic Habits” by James Clear and “The Power of Habit” by Charles Duhigg are examples of widely recognized and impactful reads in this area.
- Apps: Mobile applications can provide tailored support and tracking tools. Apps like Habitica, Streaks, and Forest use gamification and other techniques to make habit formation more engaging and enjoyable.
Professional Support
Recognizing when professional support is needed is a vital step. Mental health professionals, such as therapists or counselors, can provide guidance, coping strategies, and personalized support for individuals struggling with emotional or behavioral challenges that may hinder their progress toward resolutions. This professional support can be particularly valuable when dealing with underlying issues that may contribute to difficulties in maintaining motivation or overcoming obstacles.
Support Groups and Communities
Connecting with others facing similar challenges can be incredibly helpful. Online forums, support groups, and social media communities focused on specific resolutions (e.g., weight loss, fitness, financial goals) can provide encouragement, shared experiences, and accountability. These platforms often allow for peer-to-peer support and the exchange of practical tips and strategies.
Table of Resources
This table summarizes various resources for achieving New Year’s resolutions.
| Resource Type | Description | Link (if applicable) |
|---|---|---|
| Websites | Offer free resources and support for goal setting and habit formation, providing credible information on various topics related to well-being and self-improvement. | (e.g., Mayo Clinic, Harvard Health Publishing, Psychology Today) |
| Books | Provide in-depth explorations of specific topics, like habit formation, mindfulness, or time management. | (e.g., “Atomic Habits” by James Clear, “The Power of Habit” by Charles Duhigg) |
| Apps | Offer tailored support and tracking tools, utilizing gamification and other techniques to enhance habit formation. | (e.g., Habitica, Streaks, Forest) |
| Therapists/Counselors | Provide personalized support, guidance, and coping strategies for emotional or behavioral challenges hindering resolution progress. | (Seek a referral from a healthcare provider or online directory.) |
| Support Groups/Communities | Offer encouragement, shared experiences, accountability, and the exchange of practical tips and strategies among peers facing similar challenges. | (Search online for relevant forums or groups.) |
Wrap-Up
In conclusion, sticking to New Year’s resolutions isn’t about willpower alone; it’s about understanding yourself, setting achievable goals, building strong habits, and adapting to life’s inevitable twists and turns. This guide provides a comprehensive roadmap for success, empowering you to navigate the challenges and celebrate your triumphs. By implementing these strategies, you can turn your New Year’s aspirations into tangible, lasting improvements in your life.
Remember, self-compassion and flexibility are key—don’t be discouraged by setbacks, but learn from them. You’ve got this!